Sliwa K, et al. JACC Heart Fail. 2020 Feb;8(2):100-110.
Sliwa K, et al., conducted a study to offer much required modern data on pregnancy findings in women with uncorrected Congenital Heart Disease (CHD), as well as those at especially high risk with cyanosis or Eisenmenger syndrome.
An investigation of 10-year data from the European Society of Cardiology (ESC), EURObservational Research Programme (EORP), Registry of Pregnancy and Cardiac disease (ROPAC) Registry of women with uncorrected CHD. From January 2007 up to January 2018, pregnant women were included in this study prospectively and follow-up was conducted which includes cardiac, obstetric and fetal outcome data till 6 months post-partum. The endpoints were all-cause mortality, heart failure, arrhythmias, thromboembolic events and the occurrence of major adverse cardiac event (MACE) was considered for the analysis on maternal outcomes. Furthermore, analyses were conducted for adverse obstetric outcome and adverse fetal outcome. Of 5739 pregnancies in 53 countries, 3295 women had CHD, with 1059 uncorrected. Of the uncorrected CHD patients almost 10% (n=103) experienced PH (n = 103) and 29 (2.7%) experienced Eisenmenger syndrome. Maternal death occurred in 7 patients (0.7%) with uncorrected CHD.
In 123 (11.6%) patients, throughout pregnancy or in the first week postpartum, at least one MACE had emerged. In almost 89 patients (8.4%) pregnancy was difficult due to heart failure, of which 3 (3%) were observed solely postpartum. In almost 12 patients (1.1%), endocarditis and thrombotic events were observed (Figure 1). As compared to advanced countries, more than three-fold higher rate of hospital admission for cardiac reasons, heart failure during pregnancy and overall MACE in women were observed in emerging countries (p<0.001). Although, no significant difference was observed in maternal death (p=0.40) (Figure 2A). Of the women with uncorrected CHD, 14.3% (n=151) was observed with one or more obstetric complications during pregnancy. In almost 447 patients (42.2%), caesarean sections were conducted. Of 447 patients, 85 patients (0.8%) were observed in emergency caesarean sections. As compared to advanced countries, women coming from an emerging country showed significantly higher rate of caesarean section and intrauterine growth retardation (p<0.001) (Figure 2B). During pregnancy and ventricular tachy-arrhythmias, higher mortality and significantly greater rates of hospital admission for cardiac reasons, heart failure was observed in women with PH and cyanosis (p<0.001). Higher risk was observed if women came from an emerging country (Figure 3).
Thus, as compared to corrected CHD, a significant difference was observed in cardiac conditions in pregnant women with uncorrected CHD, with a particularly worse outcome, especially in women with Eisenmenger syndrome and from emerging countries.
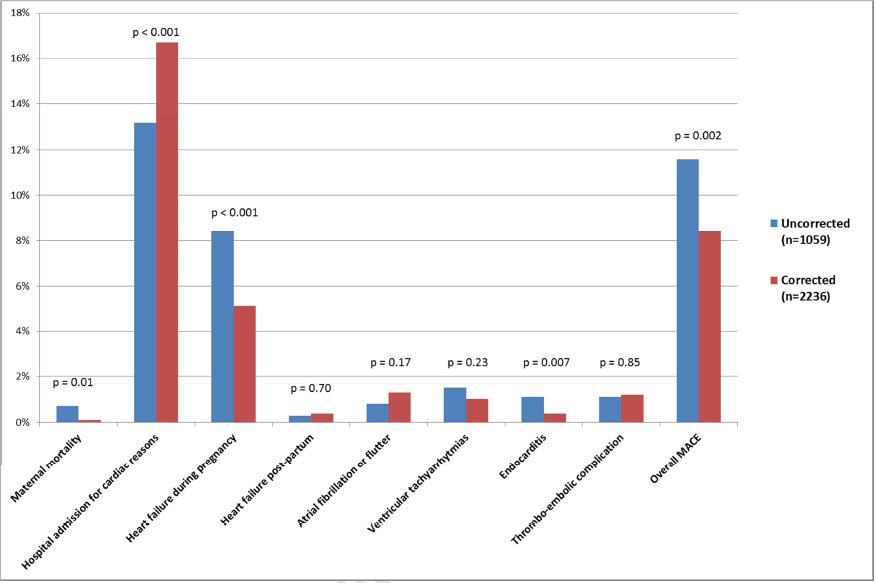
Figure 1: Comparison between uncorrected and corrected CHD in maternal cardiovascular outcome
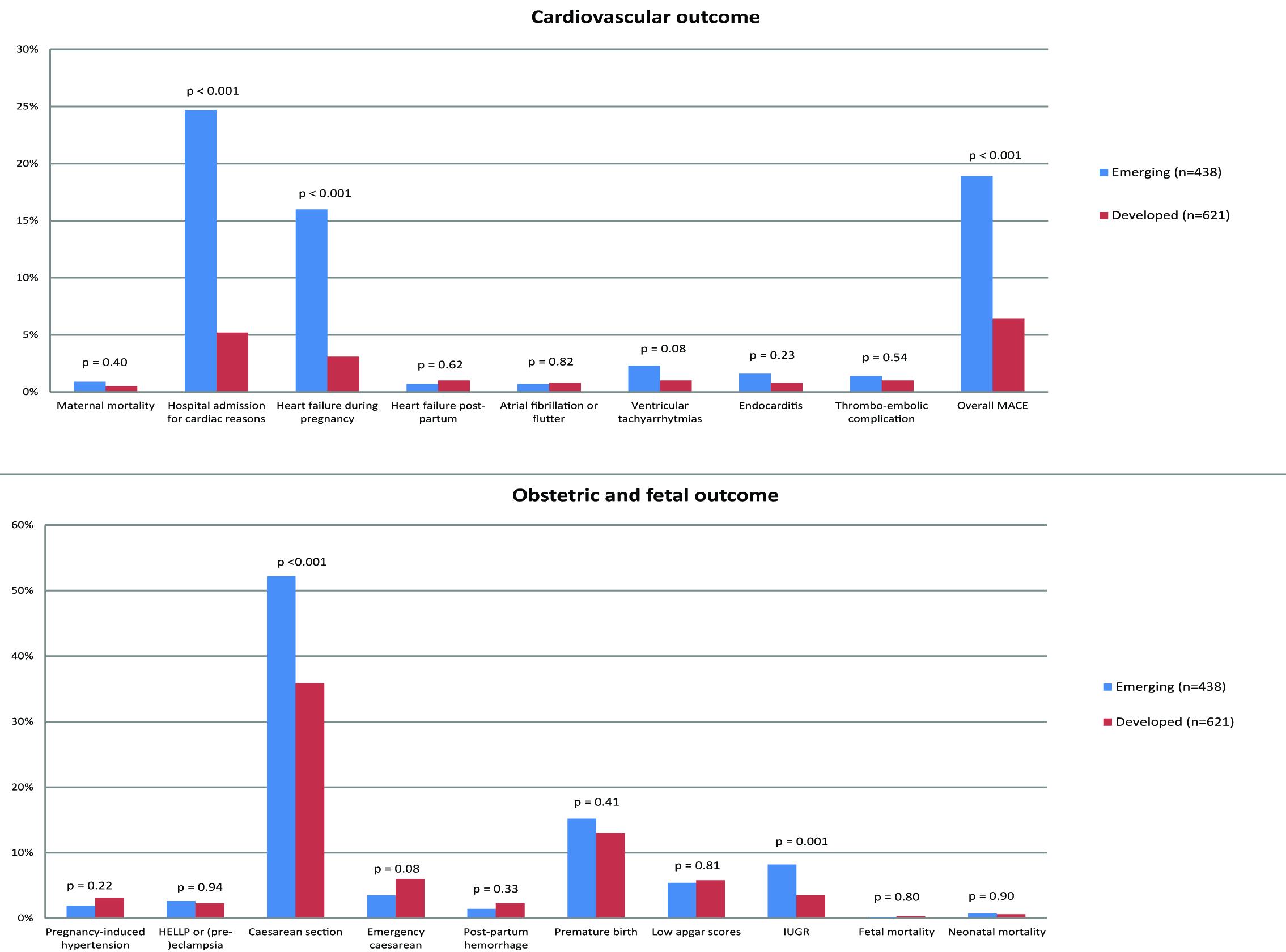
Figure 2: (A) Comparison between emerging and developed in cardiovascular outcome; (B) Comparison between emerging and developed in obstetric and fetal outcome
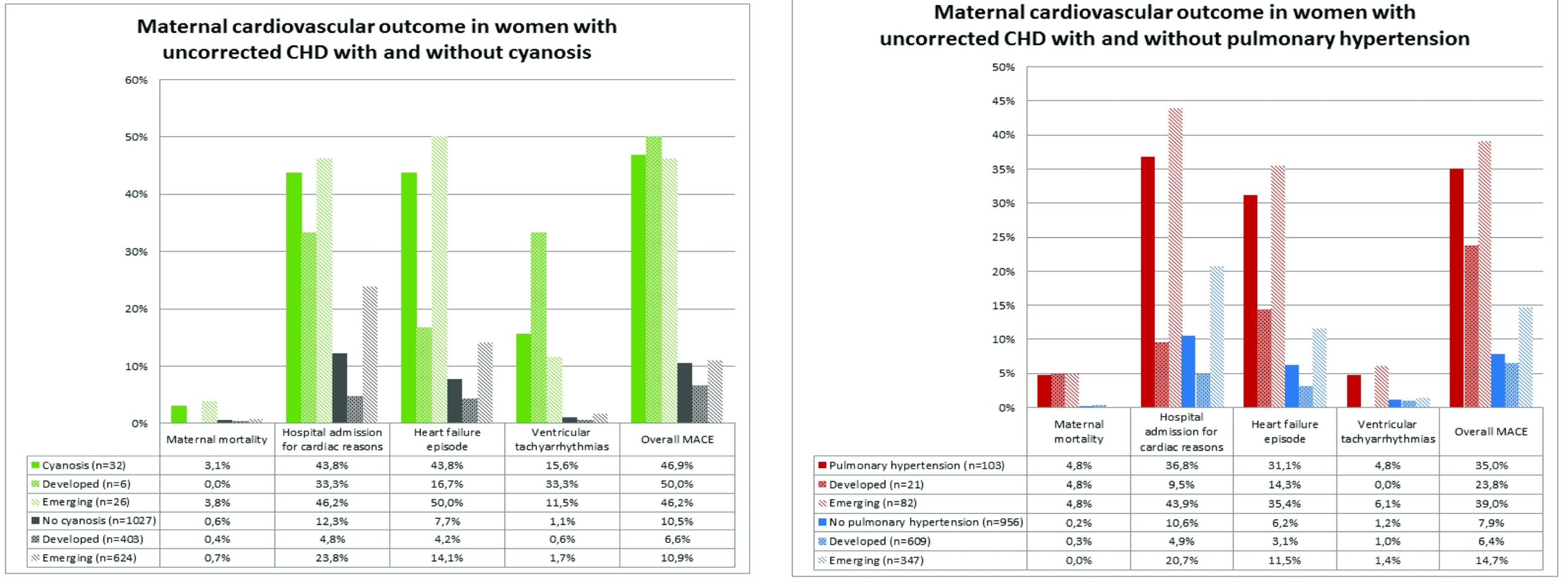
Figure 3: Maternal cardiovascular outcome in women with uncorrected CHD with and without (a) cyanosis (b) Pulmonary hypertension

