Song J. Coron Artery Dis. 2020 Mar;31(2):124-129.
Non-ST-elevation acute coronary syndrome (NSTE-ACS) assigns to a range of acute conditions resisting acute myocardial ischemia and infarctions that are common because of a sudden decrease in myocardial coronary blood flow. There is rising evidence that an increased fibrinogen (FIB) level is a predictor of adverse effects of coronary heart disease and is closely associated with cardiovascular disease (CVD) and cardiovascular risk factors. Current studies largely concur that FIB is an independent predictor of long-term prognosis in patients undergoing PCI, however, research is lacking on patients with NSTE-ACS. Thus, Song J et al., conducted a study to evaluate whether FIB is a useful predictor for long-term prognosis in patients with NSTE-ACS undergoing PCI. Furthermore, the prognostic precision of FIB was compared with the GRACE score.
The study was an evaluation of prospective group successive patients with NSTE-ACS who were hospitalized and underwent PCI from 1 January 2015 to 31 December 2016. The venous blood samples of patients were accumulated in a sodium citrate tube and stored at room temperature on the first day after admission (and before each patient underwent PCI); all samples were analysed within 120 minutes of blood collection. Preoperative FIB levels were estimated with the Von Clauss method and ACL-TOP automatic hemagglutination. The left ventricular ejection fraction (LVEF) was calculated by echocardiography during hospitalization. PCI was executed as per the current guideline recommendations after validation of NSTE-ACS. The precision of serum FIB concentrations and the GRACE score for anticipating clinical endpoints were examined according to the area under the ROC (AUC) curve and compared by a nonparametric test. ROC-AUC values of higher than 0.5, 0.75, and 0.93 were contemplated with fair, good, and very good accuracy, respectively.
1211 consecutive patients were selected from a large hospital in northeast China and 84 patients were lost to follow-up. The cutoff value for FIB to anticipate all causes of death was 3.49 with an AUC of 0.71, the sensitivity of 0.92, and specificity of 0.681 by ROC curve analysis (p < 0.001; Figure 1). Hence, the enlisted patients were classified into a low FIB group (n = 826, FIB ≤ 3.49 mg/dL) and a high FIB group (n = 385, FIB > 3.49 mg/dL). Patients with a high serum FIB level exhibited substantially greater rates of hypertension and diabetes, and higher GRACE scores, leukocyte counts, platelet counts, cardiac troponin-I, creatinine, and HbA1c as compared to those with a low serum FIB level. At the one year follow-up, 31 deaths and 43 death/nonfatal reinfarctions arose in the study group. The increased baseline FIB level was a substantial variable in association to death and death/nonfatal reinfarction in patients who underwent PCI in univariate analysis (HR = 1.949, p = 0.001; HR = 1.693, p = 0.003, respectively). The increased baseline FIB level maintained this correlation with a greater rate of death/nonfatal reinfarction after adjusting for covariates (HR = 1.498, 95% CI: 1.030–2.181, p = 0.035). A ROC curve evaluation was executed and the AUC with a 95% CI was obtained to estimate the diagnostic value of serum FIB levels. The ROC-AUC of serum FIB and the GRACE score for anticipating death/nonfatal reinfarction was 0.621 and 0.699, respectively. The serum FIB showed similar prognostic performance to the GRACE system for predicting death or nonfatal reinfarction (C-statistic: z = 1.486, p = 0.14; Figure 2).
Thus, it was concluded that in patients with NSTE-ACS undergoing PCI, the plasma FIB level is a useful biomarker to anticipate death or nonfatal reinfarction within one year. FIB levels show definitive accuracy and an anticipating value as compared to the GRACE score.
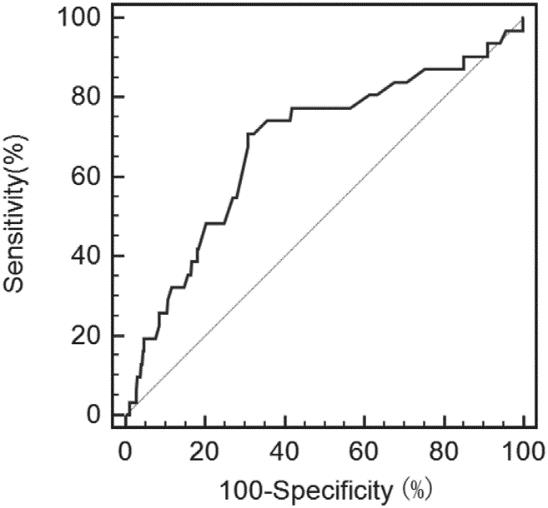
Figure 1: Receiver operating characteristic curve of all-cause mortality predicted by fibrinogen
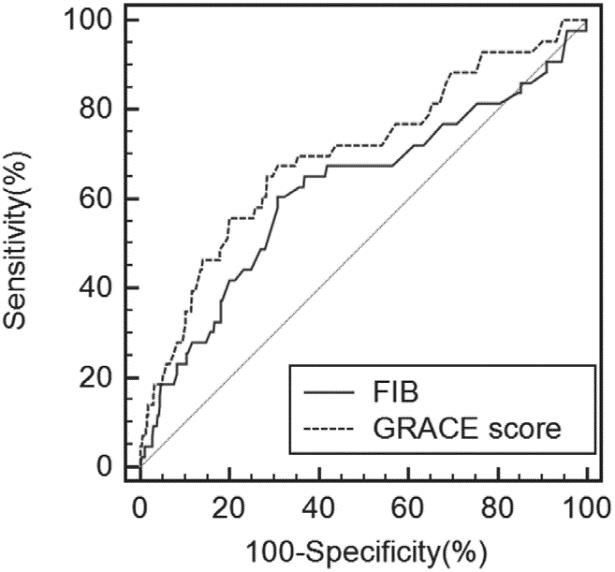
Figure 2: Receiver operating characteristic curves of fibrinogen and the GRACE risk score for death and death/nonfatal reinfarction prediction.
PCI: Percutaneous coronary intervention; GRACE: Global Registry of Acute Coronary Events; ROC: receiver operating characteristic; AUC: Area under the curve; HbA1c: Hemoglobin A1c; HR: Hazard ratio

