Mody P. Circulation. 2021 Feb 16;143(7):641-649.
Women have more poor prognostic factors associated with cardiac arrest than men was consistently shown in the studies analysing gender-based differences in outcomes following out-of-hospital cardiac arrest. Furthermore, women acquire suboptimal resuscitation care with less likelihood of obtaining bystander CPR than men impacting their discharge survival and survival with good neurological function. Inspite of this, women have a greater likelihood of ROSC compared with men after accounting for baseline characteristics. Thus, women might be expected to have higher survival because ROSC is an intermediary to surviving to hospital discharge. But, most studies have not noticed increased survival to hospital discharge for women. Thus, Mody P, et al. conducted a study to analyse gender differences in outcomes in patients successfully resuscitated from out-of hospital cardiac arrest, with the data from two large, multicenter, randomized trials to better understand this discordance among ROSC and survival to discharge.
A total 26,148 patients were enlisted in the CCC trial, following excluding patients with missing data 20,508 unique patients remained and patients co-enlisted in the Amiodarone, Lidocaine, and Placebo trial dataset. Hierarchical multivariable logistic regression models were used to analyse the correlation among gender and survival following adjustment for age, gender, cardiac arrest rhythm, witnessed status, bystander cardiopulmonary resuscitation, episode location, epinephrine dose, emergency medical services response time and duration of resuscitation. The differences in altered post resuscitation outcomes using baseline prognosis were evaluated by DNR and WLST order status. The evaluation was replicated between Amiodarone, Lidocaine, or Placebo Cardiac Arrest trial individuals.
The primary study outcome was survival to hospital discharge. A rate of survival with favorable neurological function at discharge was analysed; described as a Modified Rankin score ≤3. A DNR order rates, WLST rates, and rates of guideline-recommended procedures such as TTM and CAG were also compared.
1,825 (37.4%) were women and 3,050 (62.6%) were men in 4,875 successfully resuscitated patients. Women were older (67.5 vs. 65.3 years), acquired less bystander cardiopulmonary resuscitation (49.1% vs. 54.9%), and showed a lower proportion of cardiac arrests that were witnessed (55.1% vs. 64.5%) or showed shockable rhythm (24.3% vs. 44.6%, p<0.001 for all). A substantially greater proportion of women received DNR orders (35.7% vs. 32.1%, p=0.009) and showed WLST (32.8% vs. 29.8%, p=0.03). Women showed substantially lower discharge survival (22.5% vs. 36.3%, p<0.001, adjusted OR 0.78, 95% CI 0.66 – 0.93, p=0.005). The correlation among gender and discharge survival was altered using DNR and WLST order status such that women showed substantially decreased discharge survival in patients who were not made DNR (31.3% vs. 49.9%, p=0.005, adjusted OR 0.74, 95% C.I. 0.60 – 0.91) or did not have WLST (32.3% vs. 50.7%, p=0.002, adjusted OR 0.73, 95% C.I. 0.60 – 0.89). In contrast, no gender difference in survival was observed in patients receiving a DNR order (6.7% vs. 7.4%, p=0.90) or had WLST (2.8% vs. 2.4%, p=0.93). In the secondary group, consistent patterns of correlation among gender and post-resuscitation outcomes were noticed (Figure 1).

Figure 1: Association of women with survival to hospital discharge stratified by Do Not Resuscitate order status and Withdrawal of life-sustaining therapy
*Hierarchical multivariable logistic regression modeling was performed after adjustment for age, witnessed status, initial presenting rhythm, public location, bystander cardiopulmonary resuscitation, resuscitation duration and response time as covariates
There were no substantial differences in survival in men versus women with no ST elevation (OR for women 0.88, 95% C.I. 0.72 – 1.08, p=0.22). Finally, there was a substantial interaction among CAHP score and gender with correlation with survival to hospital discharge in restricted cubic spline analysis (pinteraction = 0.001, Figure 2).
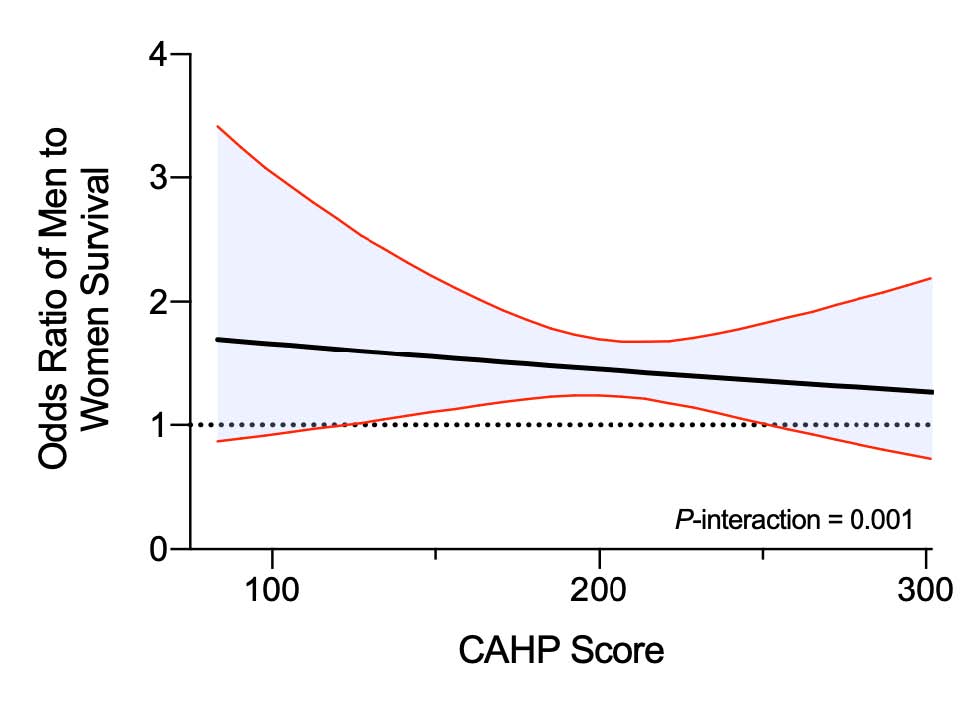
Figure 2: Association of men vs women with survival to hospital discharge across Cardiac Arrest Hospital Prognosis scores
Restricted cubic spline showing adjusted association between Cardiac Arrest Hospital Prognosis (CAHP) score and odds of men to women survival to hospital discharge. The shaded area shows the 95% confidence interval for the odds ratio point estimate. The model was adjusted for CAHP score, gender, witnessed cardiac arrest, and bystander CPR
Rates of angiography were substantially lower in women against ST segment elevation on the initial electrocardiogram. Women showed numerically lower proportion of TTM utilization not meeting statistical significance with regards to TTM in patients with initial shockable rhythm (54.5% vs. 58.9%, p = 0.10). In contrast, the use of TTM was substantially lower in women in patients with initial non-shockable rhythm (vs. men) post ROSC (28.9 vs. 33.1%, p = 0.01) (Table 1).
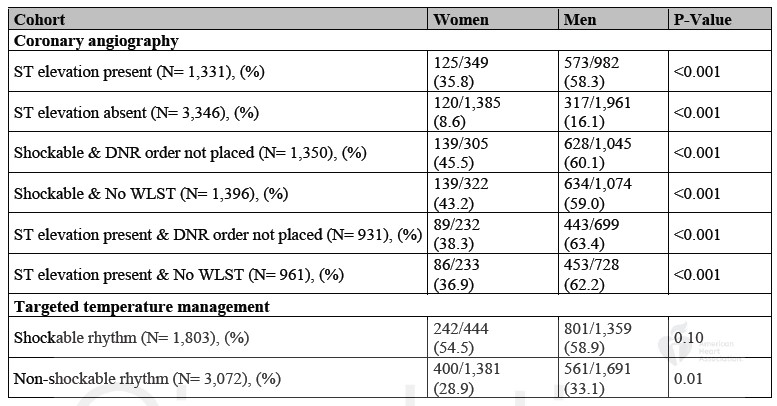
Table 1: Rates of coronary angiography and targeted temperature management among select group of resuscitated patients in primary study cohort based on presence of ST elevation on electrocardiogram, initial rhythm, and Do Not Resuscitate or withdrawal of life-sustaining status
Thus, it was concluded women less commonly survive to hospital discharge in spite of higher likelihood of return of spontaneous circulation than men that in a large, contemporary group of patients with out-of-hospital cardiac arrest. This difference in survival is most evident between women who were expected to have a beneficial prognosis. Furthermore, women less commonly acquire in-hospital procedures known to enhance survival following cardiac arrest.
CPR: Cardiopulmonary resuscitation; ROSC: Return of spontaneous circulation; DNR: Do Not Resuscitate; WLST: Withdrawal of life-sustaining therapy; TTM: Targeted temperature management; CAG: Coronary angiography; OR: Odds ratio; HR: Hazard ratio

