Heart Failure with Reduced Ejection Fraction—How to Prioritize among an Array of Available Therapies?
Kittleson M from Smidt Heart Institute, Cedars-Sinai gave a presentation on “Heart Failure with Reduced Ejection Fraction—How to Prioritize among an Array of Available Therapies?” at the American Diabetes Association (ADA) 81st Virtual Scientific Session.
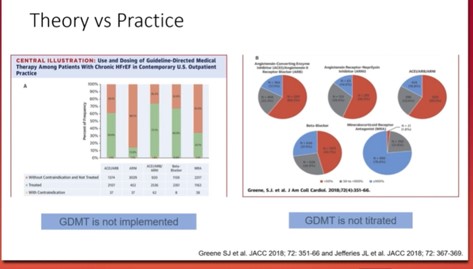
The four pillars of survival enhancing medical therapy for HErEF are angiotensin Receptor-Neprilysin Inhibitors (ARNi), β-blocker, mineralocorticoid receptor antagonist (MRA), and sodium-glucose cotransporter 2 inhibitors (SGLT2i). Cumulative risk reduction in all-cause mortality if all four evidence-based medical therapies are used- relative reduction of 72%, an absolute reduction of 25.5% and NNT=3.9 over 24 months. ACE inhibitors or ARBs or ARNI in conjunction with evidence-based beta-blockers and aldosterone antagonists are recommended for patients with chronic HFrEF to reduce morbidity and mortality. In patients with chronic symptomatic HFrEF NYHA class II or III who tolerate an ACE inhibitor or ARB, replacement by an ARNI is recommended to further reduce morbidity and mortality.
ARNI should not be administered concomitantly with ACE inhibitors or within 36 hours of the last dose of an ACE inhibitor. ARNI should not be administered to patients with a history of angioedema. One of the issues faced by clinicians in real-life scenarios is mitigating the cost for the drugs if they consider a combination therapy and if they encounter some form of intolerance, to identify which one is the causative agent.
Some ways to combat the situation with combination therapy include ensuring the patient can afford the medication stepwise. One must always ensure tolerability before proceeding and frequent use of telehealth services for follow-up.
Heart Failure with Preserved Ejection Fraction—Can We Successfully Navigate the “Black Hole” of Heart Failure?
Ibrahim NE from the Massachusetts General Hospital gave a presentation on “Heart Failure with Preserved Ejection Fraction—Can We Successfully Navigate the “Black Hole” of Heart Failure?” at American Diabetes Association (ADA) 81st Virtual Scientific Session.
Irbesartan did not improve the outcomes of patients with HFpEF. A composite endpoint in of the studies with spironolactone did not reach statistical significance however HF hospitalization was reduced. Regional variations were observed in the study, the rates of primary end-point were 4 times lower in Russia/Georgia than the Americans. The post-hoc analysis showed efficacy in Americans by not in Russia/Georgia. Appropriately selected patients with symptomatic HFpEF (LVEF≥45%, elevated natriuretic peptide (NP) level or hypotensive (HP) admission within 1 year, eGFR>30, creatinine<2.5 and potassium<5), particularly in those with elevated NP levels, use of spironolactone might be considered. Lower rates of heart failure and all-cause hospitalizations were observed in pulmonary artery pressure-guided therapy for ambulatory heart failure. A study shows that patients receiving sacubitril-valsartan were more likely to have hypotension and angioedema by less likely to have hyperkalemia. In patients with CKD and type 3 diabetes, treatment with finerenone resulted in lower risks of CKD progression and cardiovascular events than placebo.
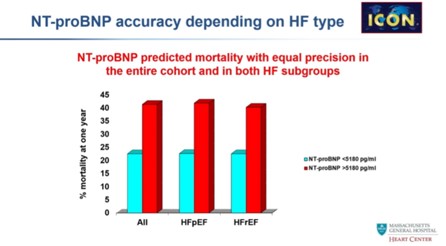
Sodium-glucose cotransporter 2 inhibitors (SGLT2i) robustly and significantly reduced the composite of total cardiovascular deaths, hospitalizations for heart failure and urgent visits for heart failure across the full range of ejection fraction, including in patients with heart failure with preserved ejection fraction. These are the first randomized data from a pre-specified analysis of clinical trials to show a significant effect of a therapy on heart failure with preserved ejection fraction, additionally demonstrating a consistent and significant benefit in women. HFpEF has low NTproBNP concentrations. NTproBNP predicted mortality with equal precision in the entire cohort and both HF groups.
HFpEF is a complex syndrome. The main goal is to manage co-morbidities. Potential drugs for HFpEF are mineralocorticoid receptor antagonist (MRA), angiotensin Receptor-Neprilysin Inhibitors (ARNi), SGLT2i and Finerenone.
Cardiovascular Risk Categories in Patients with Diabetes According to 2019 ESC/EASD Guidelines in Clinical Practice: Use of a Dedicated App (AWARE)
The 2019 ESC-EASD guidelines presented recommendations for CV risk evaluation and medical therapy in diabetic patients. 3 CV risk categories were originally described: 1) very high risk, 2) high risk and 3) moderate risk as per the presence of CVD, other target organ damage (proteinuria, renal impairment described as eGFR ≥30 mL/min/1.73 m2, left ventricular hypertrophy, retinopathy), duration of disease, age, risk factors (hypertension, dyslipidemia, smoking, obesity). In very high risk CV category SGLT2-I and GLP1-RA were recognise as therapy of choice. Berra CC, presented a session at the American Diabetes Association (ADA) 2021 81st scientific sessions: virtual which developed the web APP “AWARE”, an application software which drives on a web server and is accessed via internet browser based on this basis.
AWARE was employed as a device to evaluate CV risk of 650 type 2 diabetes patients in clinical practice from November 10th 2020 to January 10th 2021. The APP was applied with additional characteristics such as HbA1c and treatment. Total 650 patients were analysed in which 430 were very high risk patients (66%), 73 (11,2%) high risk patients, 5 (0,8%) at moderate risk while 145 patients (22%) didn’t match with any of these classifications. These patients were allocated into a further “undetermined risk” category. In all patients, median HbA1c was 7.2+1.14 (7.3+1.15% in very high risk category, 7.2+1.15% in high risk category, 6.2+0.41% in moderate risk and 6.9+1.12% in “undetermined” risk). In the very high risk category, 166 patients (38%) showed CVD, 238 patients (55%) had duration of disease >10 aa, 53 patients (12%) had proteinuria (p=0.000 vs. all other categories). In the very high risk category, either SGLT2-I or GLP1-RA were prescribed in 30% of patients.
The APP “AWARE” is convenient to recognise CV risk in diabetic. The categorization as per the criteria of 2019 ESC/EASD guidelines does not incorporates 22% of patients in clinical practice. Around 70% of patients in the very high CV risk category are not managed with the optimal drug treatment recommended by the 2019 ESC/EASD guidelines.
Early Kidney Disease—Interventions to Slow Progression of Chronic Kidney Disease
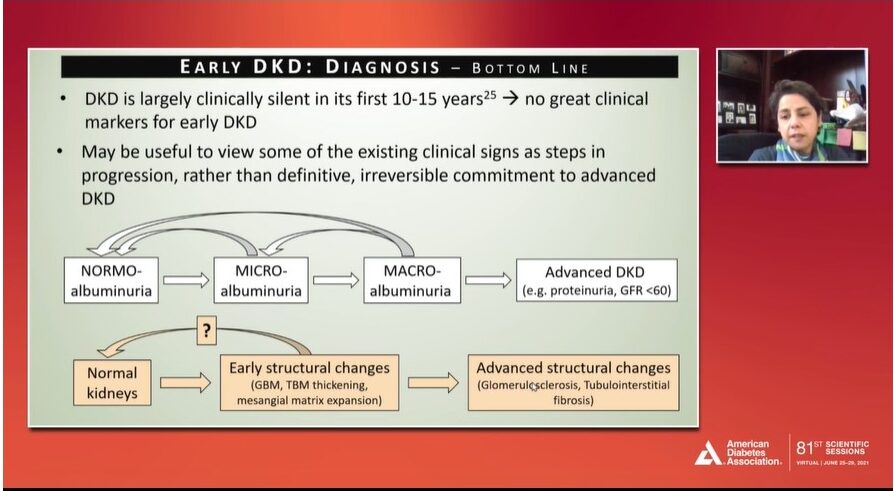
Afkarian M presented Interventions to Slow Progression of Chronic Kidney Disease on Tuesday, June 29, 2021 at American Diabetes Association (ADA) 81st Scientific Sessions, a Virtual Experience. The presentation aimed at translating diabetes and kidney disease clinical trial into clinical practice. Diagnosing diabetes kidney disease (DKD) is clinically silent for 10-15 years with no clinical markers for early DKD. Evidences suggest that hyper-filtration may not be associated with greater risk of progression of estimated GFR. Albuminuria may return to normal levels more often than progressing towards the worsening of the kidney disease challenging its utility as a key predictor of DKD progression. Structural changes are difficult to assess as it requires kidney biopsy which is not recommended in the management of early DKD.
Hypertension control is critical in slowing down the CKD progression, particularly in CKD stages, Studies have demonstrated a lower risk of mortality in patients having BP <140/90 mmHg. Although, RAAS inhibition is the cornerstone in the management of clinically relevant DKD, it has no benefit in early DKD patients with no apparent hypertension or albuminuria.
Glycemic control is critical in the management of early DKD, however, no direct trials have been performed in patients having early DKD. The drawbacks of the antidiabetic therapies such as SGLT2i, GLP-1RA and DPP4i include increased costs, limited data in slowing the progression of DKD and complex overall execution with involvement of multiple specialties in healthcare system.
It was suggested that early DKD is a complex process with no significant clinical markers and can be effectively managed with hypertension control and glycemic control in targeted population.
Advanced Kidney Disease—Mitigating Cardiorenal Risk with Renin-Angiotensin-Aldosterone System Blockade (ACEi, ARB, MRA) and SGLT2 Inhibition
Jardine MJ presented therapeutic options in Mitigating Cardiorenal Risk with Renin-Angiotensin-Aldosterone System Blockade (ACEi, ARB, MRA) and SGLT2 Inhibition on Tuesday, June 29, 2021 at American Diabetes Association (ADA) 81st Scientific Sessions, a Virtual Experience. Diabetes is the single most common cause of chronic kidney disease (CKD) leading to fall in eGFR, rise in heart failure and poor cardiovascular outcomes.
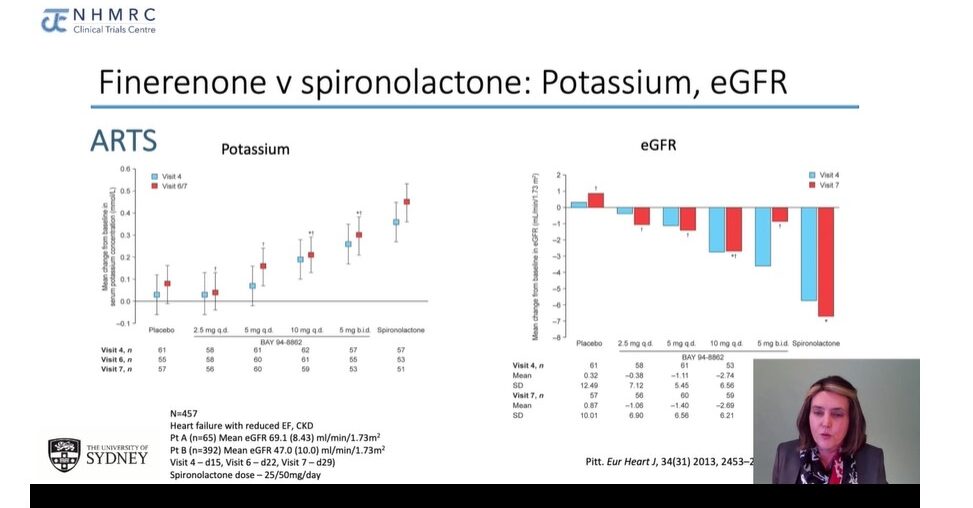
ACEi have shown reduced risk of doubling creatinine in T1D patients and contribute to slow down the DKD. They cause reduction in major cardiovascular (CV) events irrespective of the eGFR levels. ARBs are known to reduce progression of kidney disease in T2D patients. Addition of mineralocorticoid receptor anatogonists (MRAs) such as spironolactone to ACEi/ARB has shown reduced proteinuria, no change in eGFR and an increase in hyperkalaemia. A study comparing finerenone and spironolactone found a dose-dependent rise in potassium and a successful rise in eGFR. ARTS-HF study demonstrated similar results with finerenone. FIDELIO study performed on adults with T2D with kidney disease showed that finerenone reduced renal and cardiac events. It causes initial dip in eGFR followed by increase in eGFR which fell slightly after 4 months. Finerenone significantly increase potassium levels compared to placebo. Several MRAs trial are ongoing the results of which are expected to contribute significantly to the evidences. SGLT2i have been established to protect from kidney disease and preserved kidney function, the effects are achieved irrespective of diabetes status. SGLT2i may reduce risk of cardiac events and hyperkalaemia.
In patients with DKD, ACEi or ARBs, SGLT2i and non-steroidal MRAs provide cardiac and renal protection with the benefits of SGLT2i and MRA additive to ACE/ARBs.
Elevated BNP Is Associated with Higher Risk of Cardiac Arrest in Diabetic Patients Hospitalized with COVID-19
A study by Elabidin AZ was presented on Tuesday, June 29, 2021 at American Diabetes Association (ADA) 81st Scientific Sessions, a Virtual Experience. The objective of the study was to evaluate the risk factors and clinical outcomes in diabetic patients hospitalized with COVID-19.
The study comprised of 321 patients and they were stratified based on the history of diabetes mellitus and were compared using descriptive statistics. Based on the analysis, it was found that around 35% possessed a history of diabetes mellitus and they demonstrated a higher body mass index and a median HbA1c value of 7.4%. Some of the comorbidities associated with diabetes mellitus were hypertension, hyperlipidemia, chronic kidney disease (CKD), obstructive sleep apnoea, CKD and HFpEF.
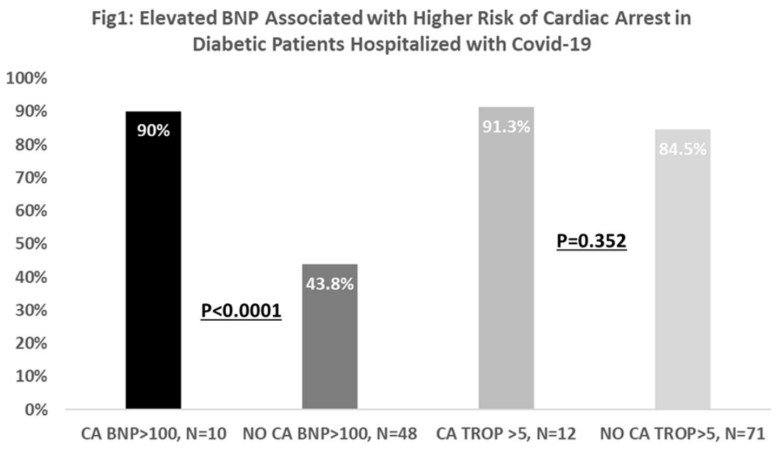
When compared to non-diabetics, the diabetes mellitus patients demonstrated longer length of stay and a greater risk of cardiac arrest (CA). Amongst the diabetic patients, around 90% patients with cardiac arrest had BNP>100 pg/ml as opposed to 43.8% in diabetic patients without CA.
These findings suggest that hospitalized diabetes mellitus patients with COVID-19 with a BNP>100 pg/ml were at a greater risk of acquiring cardiac arrest. It also highlights the importance of identifying subclinical heart failure using BNP as it may be helpful in lowering adverse cardiovascular outcomes in diabetes mellitus patients hospitalized with COVID-19.
Challenges in Glucose Management in Young Adults during the COVID-19 Pandemic
A study by Saylor J was presented on Tuesday, June 29, 2021 at American Diabetes Association (ADA) 81st Scientific Sessions, a Virtual Experience. The objective of this study was to evaluate glucose management and diabetes-related hospitalizations in young adults with Type 1 diabetes during the COVID-19 pandemic.
Surveys containing questions on hospitalization for diabetic ketoacidosis and/or severe hypoglycemia and challenges filling prescriptions were distributed electronically amongst the young adults and were associated with the College Diabetes Network at two different time points that is spring and fall.
Based on the analysis, it was found out that there was a notable increase in the hospitalizations for severe hypoglycemia from 3.4% in the spring to 10.4% in the fall. Additionally, 21% of the participants reported facing difficulties while filling prescriptions due to COVID-19 during spring as compared to 7.3% in the fall. Insulin and continuous glucose monitoring supplies were most frequently cited amongst those who reported facing difficulties while filling prescriptions. Reported hospitalizations for diabetic ketoacidosis increased from 6.7% in the spring to 10.1% in the fall.
Subsequently young adults with type 1 diabetes experienced an increased incidence of severe hypoglycemia hospitalization during COVID-19 and many of them encountered difficulty in filling and obtaining insulin and continuous glucose monitoring supplies.
Thus, these findings highlight the increased support that may be necessary to protect health outcomes during the pandemic.
Therapeutic Profile from the Canadian Registry of Chronic Kidney Disease in Diabetes Outcomes (CREDO) Study
A study by Chu L was presented on Tuesday, June 29, 2021 at American Diabetes Association (ADA) 81st Scientific Sessions, a Virtual Experience. The incidence of chronic kidney disease (CKD) in patients with type 2 diabetes (T2D) is associated with an increased risk of end stage renal disease, cardiovascular disease, hospitalizations and death.
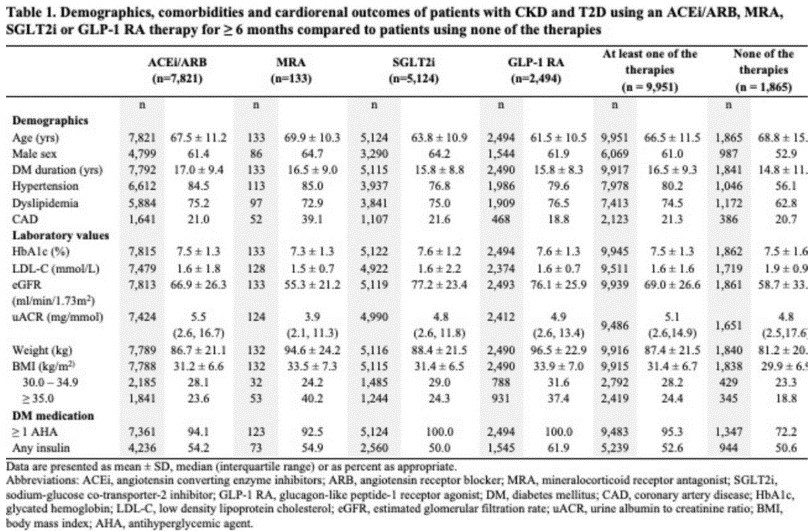
The objective of this study was to perform a subgroup analysis of the CREDO study in order to describe patients using an ACE inhibitor/Angiotensin receptor blocker or an emerging renal therapy (Mineralocorticoid receptor antagonist, Sodium glucose co-transporter 2 inhibitor or Glucagon like peptide – 1 receptor agonist) or none of the therapies. The study comprised of 11,816 patients with type 2 diabetes and chronic kidney disease.
Based on the analysis, it was found that, ACE Inhibitors/Angiotensin receptor blockers were the most frequently used medications, followed by sodium glucose co-transporter 2 inhibitors. It was further seen that a greater number of patients using an ACE inhibitor/Angiotensin receptor blocker or Mineralocorticoid receptor antagonist had hypertension, and more patients using Glucagon like peptide – 1 receptor agonist suffered from obesity as compared to the other subgroups.
Patients using ≥ 1 of the therapies demonstrated higher mean estimated glomerular filtration rate and body weight, similar HbA1c and a lower mean low density lipoprotein cholesterol as compared to patients not using any therapy.
These findings highlight the current treatment patterns amongst patients with chronic kidney disease and type 2 diabetes in Canada.
Sudden Changes in Interstitial Glucose Sensing by Remote Real-Time Continuous Glucose Monitoring as a Marker of Hypoperfusion in Critically-Ill Patients with COVID-19
A study by Hester J was presented on Tuesday, June 29, 2021 at American Diabetes Association (ADA) 81st Scientific Sessions, a Virtual Experience. The objective of this study was to assess the glucose trends surrounding cardiac arrest events to evaluate the performance of continuous glucose monitoring sensors during severe clinical instability.
The study comprised of eight cases of patients having type 2 diabetes who were diagnosed with COVID-19 requiring ICU care on IV insulin and continuous glucose monitoring therapy and were experiencing severe clinical decompensation which eventually led to cardiac arrest.
Based on the analysis, it was found that all the patients were treated with steroid therapy, vasopressors, and mechanical ventilation. Around 50% of the patients had a sudden cardiac arrest and drop in mean arterial pressure (MAP) while the other four patients had a prolonged decline in MAP prior to experiencing a cardiac arrest. In those who experienced a sudden cardiac arrest, the continuous glucose monitoring values demonstrated an abrupt fall following the cardiac arrest.
Additionally, the rapid down trending of continuous glucose monitoring values in those with prolonged hypotension occurred around 6 hours prior to cardiac arrest. During this time, the continuous glucose monitoring values stopped correlating with the point-of-care (POC) tests.
These findings suggest that real-time continuous glucose monitoring in critically-ill patients may provide clinical information beyond glucose control and also highlights the fact that rapid decline in controlled glucose monitoring values that do not correlate with POC glucose testing are associated with both sudden and prolonged changes in arterial pressure.
Impact of COVID-19 on Diabetes Self-Management and Care
Zupa M presented a study “Impact of COVID-19 on Diabetes Self-Management and Care” at American Diabetes Association (ADA) 81st Virtual Scientific Session. During the COVID-19 pandemic stay at home orders, changes in business and clinic operations and financial concerns may have affected how adults with diabetes obtained food, medications, medical care and performed diabetes self-management, especially in low-resource urban communities.
The experiences of adults with type 2 diabetes participating in a federally qualified health center diabetes management program were assessed. Among 72 patients, 61 completed telephone surveys from July to October 2020 in Spanish and English. 74% of respondents were Latino with Spanish as their preferred language. Respondents’ mean age was 54 years, 62% were female, and 57% had less than a high school degree. Almost 5 patients reported testing positive for COVID-19, and 7 lived with someone who tested positive.
61% of 33 respondents who worked outside the home prior to COVID-19 had lost their jobs or were working fewer hours. When asked how their diabetes management behaviours changed as a result of the pandemic, 53% said they did less physical activity, while 25% said they did more. 18% said they were eating less healthily, while 38% said they were eating more healthily. Healthy food was more difficult to obtain by for 43% of respondents. 15% said they took their medications more frequently, while 5% said they took them less frequently. 61% said it was becoming more difficult to get medical help. During the pandemic, 41% of people were more concerned about managing their diabetes, and 49% felt more socially isolated. Patients in this low-resource urban setting experienced both positive and negative changes in diabetes self-management behaviours as a result of COVID-19.
Patients with diabetes could benefit from programmes that facilitate access to medications and health care, provide virtual support for self-management and other healthy habits, connect patients with financial and food security concerns to community resources, and address stress and social isolation through virtual diabetes support groups, all of which could help patients adapt to pandemic changes.

