Wells A. Circulation. 2021 Jul 6;144(1):23-33.
Depression and anxiety are substantial factors in cardiovascular disease (CVD), aiding to poor prognosis. Unfortunately, current psychological therapies provide mixed, usually small enhancements in these symptoms. Metacognitive therapy (MCT) is a theory-based, structured therapy perspective that may be distinctly adapted to approaching the psychological requirements of patients with CVD. Wells A, et al. reported the results of the PATHWAY trial, the first large-scale trial of group-MCT in patients with CVD patients which analysed for the first time the impacts of group MCT; 6 sessions on anxiety and depressive symptoms with the addition of cardiac rehabilitation (CR).
A multicenter, 2-arm, single-blind randomized, controlled trial compared group- MCT plus usual CR (MCT+CR) with usual CR alone with 4- and 12-month follow-up. Patients were enrolled from CR services at 5 National Health Service (NHS) Trust hospitals. A total of 3808 patients were referred to CR from July 13, 2015 to January 12, 2018, of whom 992 patients showed an increased Hospital Anxiety and Depression Scale (HADS) score and were evaluated for eligibility. Accordingly, 332 patients enlisted to the trial, of whom 163 (49.1%) were randomly assigned to MCT+CR and 169 (50.9%) to CR. Randomization was done with 1:1 minimizing balancing arms on sex and HADS scores within hospital site. The primary outcome was HADS total following therapy (4-month follow-up). Secondary outcomes were individual HADS, traumatic stress symptoms, and psychological procedures incorporating metacognitive beliefs and repetitive negative thinking. An intention to treat was used for the evaluation.
The MCT+CR arm showed substantial reduction in the primary outcome (HADS total score at 4 months) with adjusted group difference (–3.24 [95% CI, –4.67 to –1.81]; p<0.001; SMD=0.52), also with the difference at the 12-month secondary outcome point (–2.19 [95% CI, –3.72 to –0.66]; p=0.005; SMD=0.33) (Figure 1).
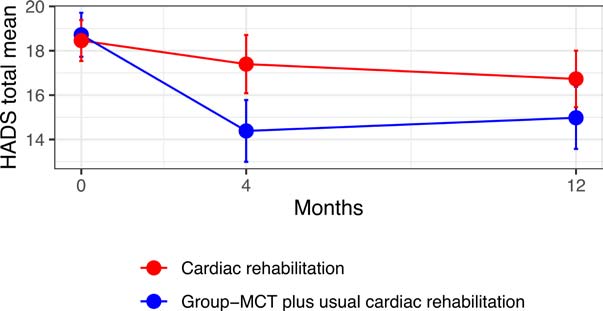
Figure 1: Unadjusted mean total HADS scores at baseline, 4-month follow-up, and 12-month follow-up. Bars are 95% CIs.
Patients in the MCT+CR arm showed substantial lower mean HADS anxiety subscale score at both 4 months (–1.67 [95% CI, –2.54 to –0.81]; p<0.001; SMD=0.44) and 12 months (–1.35 [95% CI, –2.22 to –0.48]; p=0.002; SMD=0.34), in addition of a lower HADS depression subscale mean score at 4 months (–1.58 [95% CI, – 2.37 to –0.79]; p<0.001; SMD=0.47) however not at 12 months (–0.85 [95% CI, –1.75 to 0.05]; p=0.065; SMD=0.23). The intervention enhanced outcomes substantially for both depression and anxiety symptoms than usual care while evaluating separately. Sensitivity analysis supported these outcomes with multiple imputation of missing values. MCT+CR showed favourable results in most secondary outcomes, with medium to high impact sizes for psychological mechanisms of metacognitive beliefs and repetitive negative thinking. No adverse therapy-associated incidents were outlined. (Table 1)
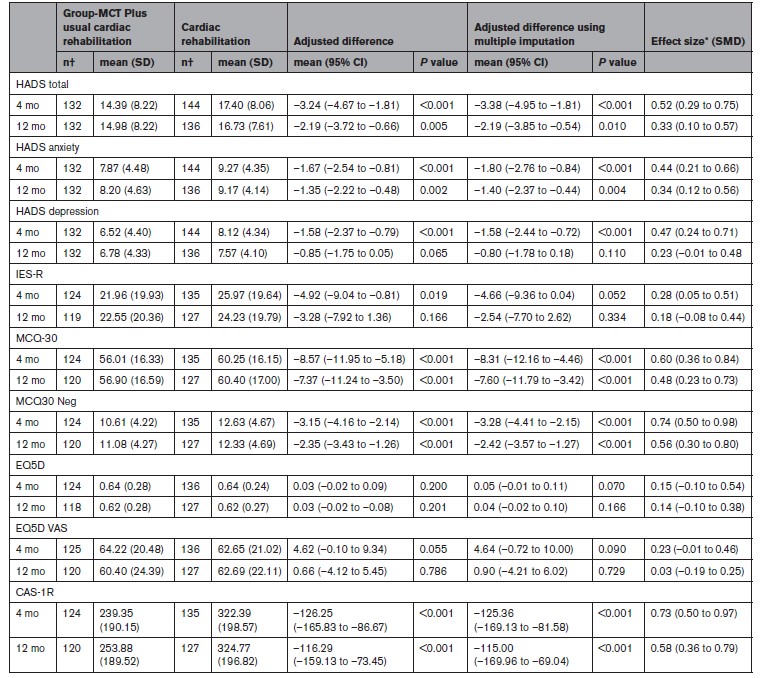
Table 1: Summary of Analyses of Primary and Secondary Outcomes
CAS-1R indicates Cognitive-Attentional Syndrome 1–Revised; HADS, Hospital Anxiety and Depression Scale; IES-R, Impact of Event Scale–Revised; MCQ-30, Metacognitions Questionnaire 30; MCQ-30 Neg, Metacognitions Questionnaire 30 negative subscale; MCT, metacognitive therapy; SMD, standardized mean difference; and VAS, visual analogue scale. *Adjusted mean difference divided by pooled SD of change scores from baseline. †Numbers of patients with useable scores varied by outcome.
Group-MCT seems to be safe and efficacious in decreasing anxiety and depression and enhancing psychological effects in routine CR further those accomplished in usual care. The advantages emerged to be stable across a 12-month follow-up period.

