International Session – Universal Definition and Classification of HF Joint Session with the Heart Failure Association of the European Society of Cardiology (HFA-ESC) and the Japanese Heart Failure Society (JHFS)
Biykem Bozkurt from Baylor College of Medicine, presented the opening topic “What is New in the Universal Definition of HF? Summary and Future Implications” for the session International Session – Universal Definition and Classification of HF Joint Session with the Heart Failure Association of the European Society of Cardiology (HFA-ESC) and the Japanese Heart Failure Society (JHFS), at the HFSA Annual Scientific Meeting 2021.
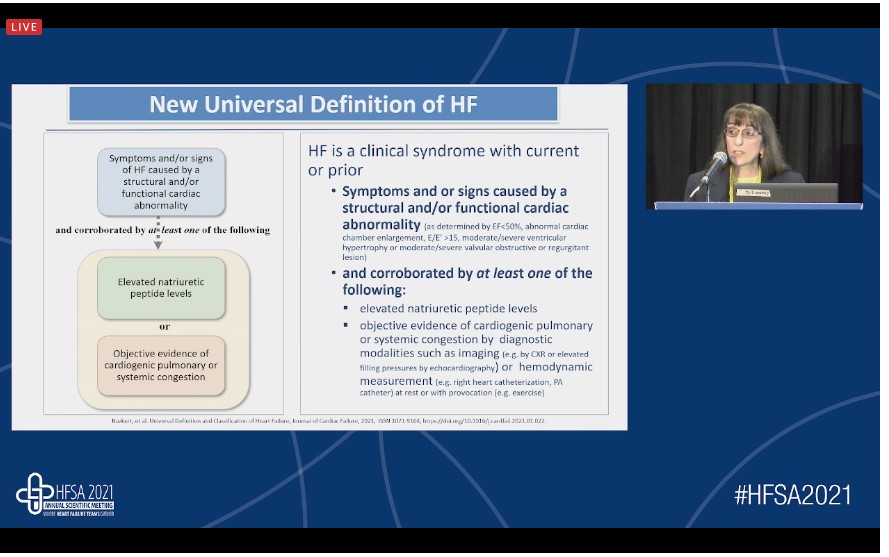
Text book definition “Heart failure”: A clinical syndrome caused by the inability of the heart to meet tissue metabolic requirements. Few patients with heart failure (HF) only meet the historical HF definition. The new universal definition of HF is defined as “Heart failure is a clinical syndrome with current or prior symptoms and or signs caused by a structural and/or functional cardiac abnormality and corroborated by at least one of the following: elevated natriuretic peptide levels, objective evidence of cardiogenic pulmonary or systemic congestion by diagnostic modalities such as imaging or hemodynamic measurements. Standardization of HF syndrome definiton may help to enhance appropriate diagnosis and opimisation of Guideline-directed medical therapy and achieve uniformity of care. The new revised classification of heart failure includes patients at risk for heart failure, pre-HF, HF and advanced HF.
The ejection fraction (EF) classification of HF in universal definition classifies HF:
- HF with reduced EF (HFrEF) [HF with left ventricular ejection fraction (LVEF) ≤ 40%];
- HF with mildly reduced EF (HFmrEF) [HF with LVEF 41-49%];
- HF with preserved EF (HFpEF) [HF with LVEF ≥ 50%];
- HF with improved EF (HFimprEF) [HF with a baseline LVEF ≤ 40, a ≥ 10 point increase from baseline LVEF, and a second measurement of LVEF >40%].
There has been failure of HF treatment in the last two decades. Current standard of care for HFrEF involves beta-blockers, ACEi/ARBs/ARNI, MRA, and SGLT2-inhibitors.
HF syndrome definition has been standardised. New revised classification of HF is easy to understand by patients as well as clinicians. The clinical trajectories terminology has changed from stable HF to persistent HF and recovered HF to HF in remission.
SGLT2 inhibitors: Reviewing their Role in Type 2 Diabetes, Heart Failure and Chronic Kidney Disease
Richard Pratley from Advent Heath Diabetes Institute, Ontario, presented an illuminating talk on the topic” SGLT2 inhibitors: reviewing their role in type 2 diabetes, heart failure, and chronic kidney disease” at the HFSA Annual Scientific Meeting 2021. His talk was focused on identifying the patients with type 2 diabetes (T2D), heart failure (HF), or chronic kidney disease (CKD) who would benefit from a sodium-glucose cotransporter-2 (SGLT2) inhibitor. He talked about the guidelines and specific evidence for the management of cardiovascular (CV) and or renal risk in patients with T2DM. He explained the mechanism of action of SGLT2 inhibitors in T2DM, HF, and CKD. He also mentioned clinical trial data on the use of SGLT2 inhibitors for managing CV and/or renal risk in patients with T2DM.
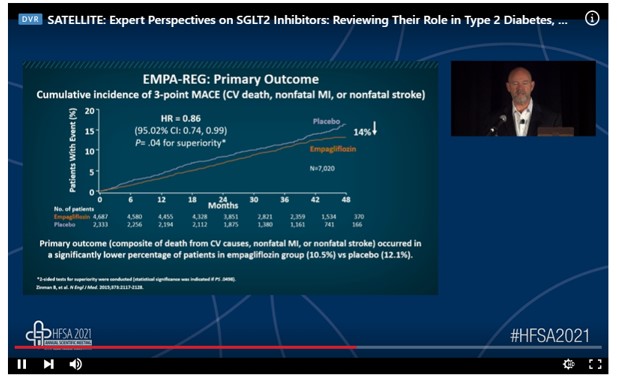
HF is one of the first manifestations of T2D-related CV disease (CVD). DM is associated with an increased incidence of heart failure and mortality. Intensive glucose control does not reduce the incidence of HF. On the other hand, diabetes is the leading cause of the end-stage renal disease (ESRD). Mortality is increased in patients with T2 D and kidney disease. SGLT2 inhibition reduces renal glucose reabsorption, plasma glucose, body weight, blood pressure, plasma uric acid, albumin excretion and improves renal and CV outcomes. SGLT2 inhibitors improve glomerular loading conditions. Canagliflozin, empagliflozin, dapagliflozin, and ertugliflozin food and drug administration (FDA)-approved SGLT2 inhibitors. Various CV outcome trials (CVOTs) have demonstrated the positive effects of SGLT2 inhibitors. EMPA-REG trial showed that the cumulative incidence of 3-point major cardiovascular events (MACE) was significantly reduced with empagliflozin as compared to placebo. The other CVOTs have also demonstrated positive effects of SGLT2 inhibitors. Guidelines are now transitioning from a gluco-centric focus to one emphasizing patient-relevant outcomes, including CVD, HF, and CKD, and hence supports the use of SGLT2 inhibitors in T2D patients at high risk of CVD, HF, and CKD.
SLGLT 2 inhibitors have proven benefits to reduce the risk for CVD, HF, and CKD progression and should be considered in high-risk patients regardless of glycemic control.
Restore EF Trial- Impact of Hemodynamic-Supported Revascularization on LVEF
Jason Wollmuth, Director, Complex Coronary Interventions, Providence Heart Institute, Portland, Oregon, presented a captivating talk on the topic, “Restore EF trial- Impact of hemodynamic-supported revascularization on LVEF” at the HFSA Annual Scientific Meeting 2021.
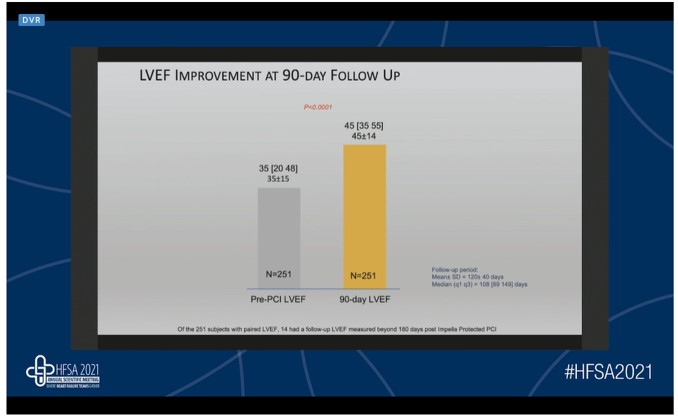
The extent of coronary artery disease (CAD) is associated with prognosis in heart failure. Coronary artery bypass graft (CABG) is associated with sustained reductions in death as well as cardiovascular (CV) hospitalizations in ischemic cardiomyopathy (ICM). CABG has proven to be effective in patients with severe left ventricular dysfunction. In a meta-analysis of observational studies of CABG in patients with left ventricular ejection fraction (LVEF) 35%. A total of 26 studies comprising 4911 patients were included. The operative mortality and 5-year mortality were noted to be 5.3% and 26.4%, respectively. A significant improvement in LVEF was noted with CABG revascularization. The population of complex and high-risk percutaneous coronary intervention (PCI) is growing at a faster rate. PCI after surgical consult grew six times faster than total PCI. The evidence for PCI in ICM is limited. Impella heart pumps mitigate the inherent risks of surgical ineligibility. The PROTECT II and cVAD registry trial including 331 patients reported no difference in the mortality and major adverse cardiac and cerebrovascular events in CABG eligible and ineligible unprotected left main PCI patients. In high-risk Impella-supported PCI patients, a considerable improvement in LVEF has been noted. The “Restore EF” study was a multicenter, single-arm, prospective clinical study conducted in post-Impella supported high-risk PCI patients to validate the best practices. The primary endpoint of the study was LVEF at a 90-day follow-up. A significant improvement in LVEF at 90-day LVEF was noted as compared to pre-PCI LVEF. Follow-up LVEF improvement from baseline was significantly higher in subjects who underwent complete revascularization. The primary endpoint stratified by quartile baseline also showed significant follow-up LVEF improvement for patients with depressed pre-PCI LVEF. There was a 76% and 97% reduction in heart failure and angina symptoms.
Revascularization in patients with low LVEF is challenging with limited randomized trial data. Surgical revascularization has been shown to improve outcomes including death and CV hospitalization with probable improvement in LVEF. Increasingly, surgical turndown patients are being referred for complex PCI and hemodynamic support is often used during revascularization. Early data suggest hemodynamic supported revascularization in patients with low LVEF leads to improvement in LVEF and this was also demonstrated in real-world consecutive patients in the RESTORE-EF trial. Further trials will help to determine the value of percutaneous revascularization and optimal approach in surgical turndown patients.
Multidisciplinary Perspectives on Recognizing, Diagnosing and Managing Polyneuropathy Caused by hATTR Amyloidosis (NO CEUs)
John Eatman from North Kansas City Hospital and Summet Mitter from Mount Sinai Hospital discussed their clinical experience in recognizing, diagnosing, and managing adult patients with polyneuropathy caused by hereditary transthyretin-mediated (hATTR) amyloidosis. They highlighted the signs and symptoms that may help identify patients with polyneuropathy of hATTR amyloidosis through case-based discussion.
An amyloidosis is a heterogeneous group of disorders characterized by the deposition of insoluble protein aggregates in tissues. It can be inherited, systemic, or localized. The two types of ATTR amyloidosis are wild-type ATTR amyloidosis and hATTR amyloidosis. More than 120 different TTR gene variants have been identified some of which are more common in certain populations. The red flag symptoms in such patients could be peripheral sensory-motor axonal polyneuropathy, bilateral carpal tunnel syndrome, and lumbar spinal stenosis. hATTR amyloidosis can be misdiagnosed with different polyneuropathy as well as cardiac conditions. Accurate diagnosis is critical for early intervention. Diagnosing hATTR amyloidosis is a multistep process; raise clinical suspicion (red flags/family history of hATTR amyloidosis), identify the signs through diagnostic tools (sensory-motor, autonomic and cardiac), and establishing the diagnosis. A multidisciplinary team approach impacts overall patient management.
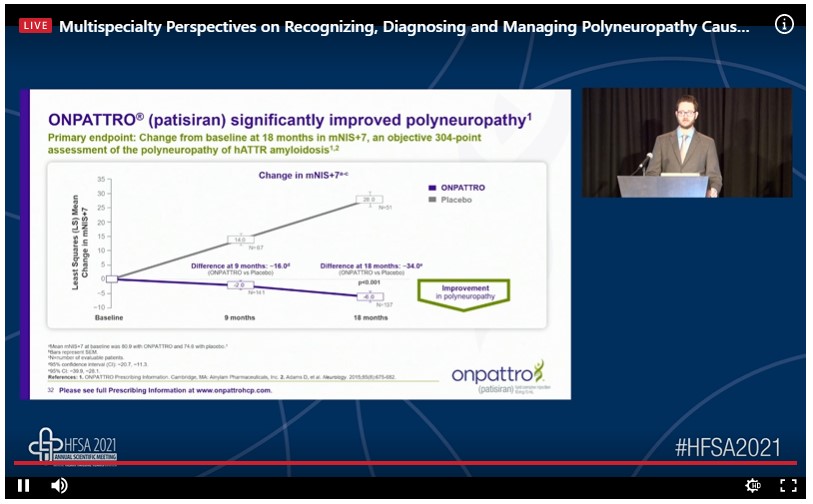
ONPATTRO® (patisiran) has been found effective for the treatment of polyneuropathy in patients with hATTR amyloidosis. ONPATTRO® (patisiran) reduces the TTR production in the liver. APOLLO-the largest controlled study in hATTR amyloidosis patients found that ONPATTRO® (patisiran) significantly improved polyneuropathy symptoms. 50% of patients treated with ONPATTRO® (patisiran) experienced a reversal in neuropathy impairment from the baseline. ONPATTRO® (patisiran) significantly improved quality of life. Early treatment led to sustained and durable improvements in quality of life for up to 2 years. ONPATTRO® (patisiran) improved autonomic neuropathy symptoms. In addition, ONPATTRO® (patisiran) improved orthostatic intolerance, gastrointestinal symptoms, and nutritional status.
ONPATTRO® (patisiran) is a useful option for treating polyneuropathy in patients with hATTR amyloidosis as it has been shown to markedly reduce the neuropathic impairment and improves the overall quality of life (patient mobility, self-care, usual activities, pain discomfort).
A Computed Tomography Reconstruction Software to Model Ventricular Assist Device Implantation Position
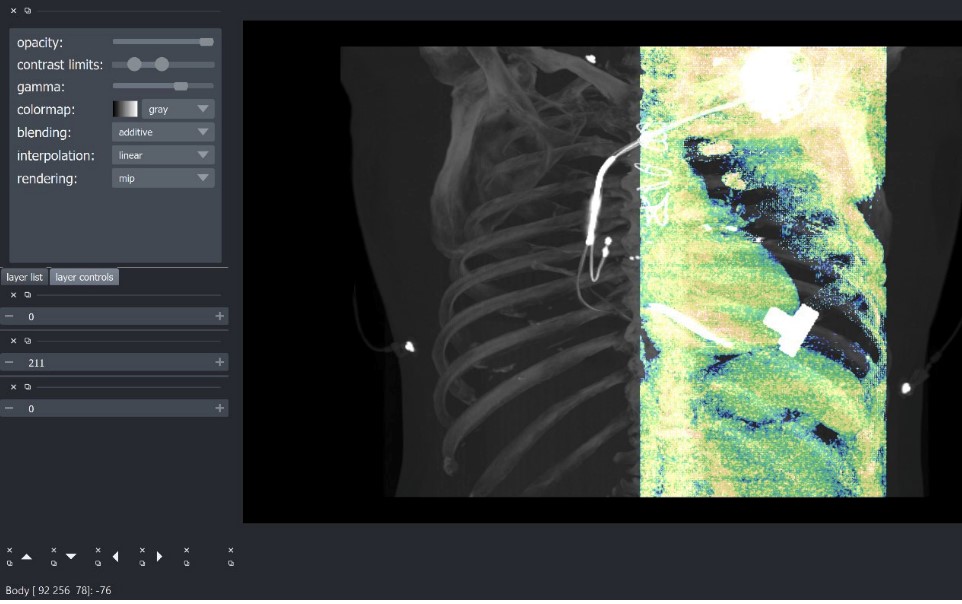
Andrew S, et al, presented a poster session on the topic “A computed tomography reconstruction software to model ventricular assist device implantation position” at the HFSA Annual Scientific Meeting 2021.
This study aims to develop a program that virtually models a VAD into the 3-dimensional rendering of the myocardium and chest using computed tomography images. A python code process was created with a 4D retrospective cardiac CT dataset and then integrated with high-definition 3D VAD model. Rather than creating a full-fledged viewer and analytics tool, which would be too costly and time-intensive a tool, was created that can be used to complement the capabilities of professional imaging processing software such as 3 dimension or visage. The user can adjust the viewer to better isolates the heart prior to simulated VAD implant placement. The DICOM directories produced by this program can be opened directly in the software already used in daily clinical imaging to allow for more in-depth analysis of desired implant placement and cannula positioning which can aid in pre-operative and intra-operative planning.
The next steps of the project will be to enable VAD implant model to be propagated across the 3D scan time series increase computational efficiency and view clarity as well as output the resulting DICOM directory so that it can be opened in visage or a similar tool. In a future version of the project, an automatic placement feature and fluid dynamic analysis to validate the proposed implant location.
Analysis of Clinical, Biochemical and Echocardiography Criteria for Heart Failure with Preserved Ejection Fraction
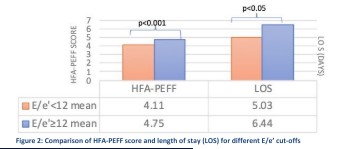
Stringer B presented a poster session on the topic “Analysis of Clinical, Biochemical and Echocardiography Criteria for Heart Failure with Preserved Ejection Fraction” at the HFSA Annual Scientific Meeting 2021. He aimed to compare the sensitivities of various clinical, biochemical and echocardiographic criteria used to diagnosis HFpEF on a cohort of admitted HFpEF patients.
It was carried out as a retrospective review of inpatients with a primary diagnosis of HFpEF over a 2- years. Review of patient demographics, medical comorbidities and lab results was carried out. Echocardiograms were analyzed, including parameters of diastology to determine H2FPEF, HFA-PEFF scores and American Society of Echocardiography diastolic dysfunction (ASE-DD).
The sensitivity of 94% was found for Brain natriuretic peptide (BNP) greater than 100 pg/mland ASE-DD criteria for diastolic dysfunction had a sensitivity of 58%. H2FPEF risk percentage of ≥90% had sensitivity of 63%. Septal E/e’ of ≥15 had a sensitivity of 57% which increased to 90% when cut-off was lowered to ≥10.
In patients who had E/e’ ≥12 had significantly higher H2FPEF score, HFA-PEFF score and length of stay (p<0.05).
The study shows that current diagnostic criteria for HFpEF have relatively low sensitivity. Diagnostic sensitivity can be improved by lower E/e’ cut-off. The correlation of E/e’ and BNP suggests a relationship between the functional and biochemical entities of HFpEF.
The Effect of COVID-19 Infection on Tacrolimus Metabolism in Heart Transplant
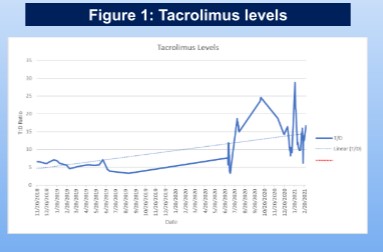
Gopalan R presented a poster session on the topic “The Effect of COVID-19 Infection On Tacrolimus Metabolism in Heart Transplant” at the HFSA Annual Scientific Meeting 2021. This study aimed to understand how COVID-19 and its treatment affect tacrolimus metabolism in solid organ transplant.
The cornerstone management strategy to balance the immune response with the potential for rejection of the graft has remained reliable on tacrolimus levels. We present a case of a heart transplant recipient with highly elevated tacrolimus levels following COVID-19 infection despite little to no tacrolimus administration and no other known drug-drug interactions. This case presents a 58-year-old male with history of ischemic cardiomyopathy; status post orthotopic heart transplantation. After 2 years, he presented to the ED with complaints of jaw pain, symptoms of urinary retention and 3 days of diarrhoea. The patient had been maintained on tacrolimus 0.5mg BID for 8 months with associated trough levels between the goal range of 4-8ng/mL. T: D ratio remained stable on tacrolimus 0.5mg BID before COVID-19 infection. The ratio rose following infection and remained elevated 8 months later despite reducing the dose to 0.5mg QAD.
A relationship is suggested between SARS-COV-2 viremia with tacrolimus metabolism.
The Persistent Heart Failure and Mortality Burden Following Anterior STEMI Treated with PCI; The Role of SSO2 Therapy

Gopalan R gave an enlightening presentation at the HFSA, 2021 on the topic “The Persistent Heart Failure and Mortality Burden Following Anterior STEMI Treated With PCI; The Role Of SSO2 Therapy”. The study hypothesised that Supersaturated oxygen (SSO2) can improve the outcomes in patients treated with primary PCI. It is an FDA approved therapy to deliver to the left anterior descending coronary artery immediately for STEMI. Comparison of 2005-2008 and 2016-2018 Medicare Data rates of mortality and REHOSP for HF was done using descriptive and regression analysis. 100 IC-HOT participants were matched to a Medicare beneficiary to form a comparison group with similar characteristics also treated with primary PCI.
The eligible Medicare group for comparison with IC-HOT included 10,634 cases. The IC-HOT treatment group was observed to have reduced mortality in comparison with the matched Medicare group at 1 year (0 vs 4.6%, p <0.02). In the Medicare group at 1 year, rehospitalisation for HF in IC-HOT was lower (1.1 vs 9.2%, p <0.05) despite a significant decrease in the 1-year REHOSP for HF from the early to later Medicare cohort. The risk adjusted 1-year and 2-year mortality rates increased from the early to later Medicare cohort with anterior STEMI treated with PCI alone.
There is no improvement observed for mortality and REHOSP for HF for MEDICARE patients. Infarct size reduction with h SSO2 therapy has the potential to favorably impact this growing clinical burden in an aging population.
SGLT2 Inhibitors: Cardiovascular Outcomes from DAPA-HF, Emperor-Reduced and SOLOIST-WHF
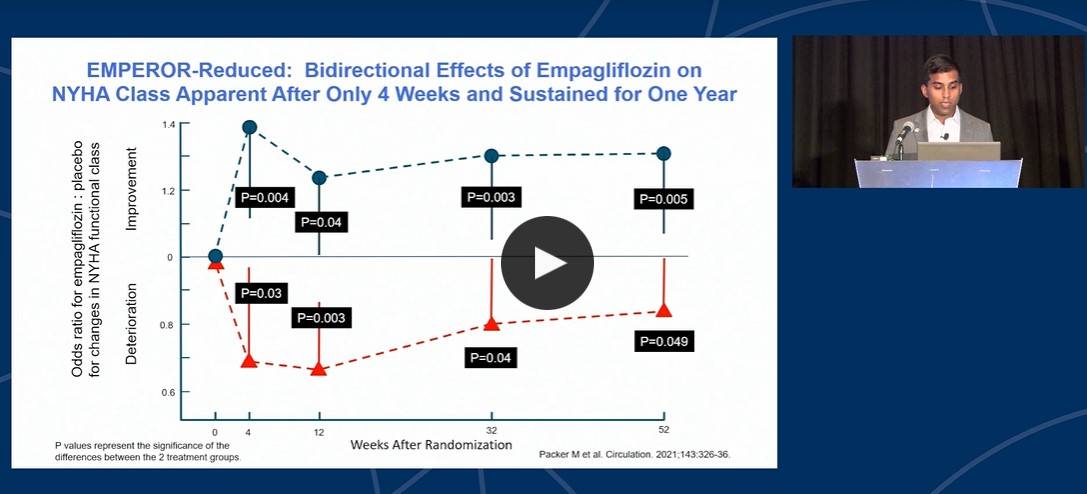
Vaduganathan M gave an enlightening presentation on the topic “SGLT2 Inhibitors: Cardiovascular Outcomes from DAPA-HF, Emperor-Reduced and SOLOIST-WHF” under the session “SGLT2 Inhibition and Heart Failure: Translating the Evidence to Clinical Practice (CEUs)” at the HFSA Annual Scientific Meeting 2021. SGLT2 Inhibitors undergoes rapid oral absorption, has long half-lives and no clinically relevant drug-drug interactions.
SGLT2 Inhibitors lose glucose lowering properties in advanced CKD and has limited risk of hypoglycaemia. All FDA approved SGLT2 Inhibitors are highly selective. A meta-analysis of the EMPEROR-reduced and DAPA-HF trials show that SGLT2 inhibitors results in 13% reduced risk of death, 26% reduction in CV death or HF hospitalization, and 38% reduction in kidney outcomes. Only modest decrease in background diuretic doses with SGLT2 inhibitors in HF trials and no anticipatory changes were observed. Bidirectional effects of Emplagliflozin on NYHA class apparent after only one week and the effects were sustained for one year. It takes around 28-56 weeks until the GDMT is fully implemented with various medications in place. An ideal HFrEF therapy consists of:
- One pill, one per day, with no titration
- Improves survival and prevents hospitalization
- Improves quality and functional status
- Benefits appear rapidly within days to few weeks of initialization
- Well-tolerated and safe
- No adverse renal effects observed
As per 2021 ESC HF guidelines, dapagliflozin or Emplagliflozin is recommended for patients with HFrEF to reduce the risk of hospitalization and death and SGLT2 inhibitors can be considered as a first line treatment for ASCVD, CKD or HFrEF.
SGLT2i represents cornerstone management for treatment of patients with HF and reduced HF and can be initiated during or soon after hospitalization of HF.
SGLT2 Inhibitors: Renal Outcomes
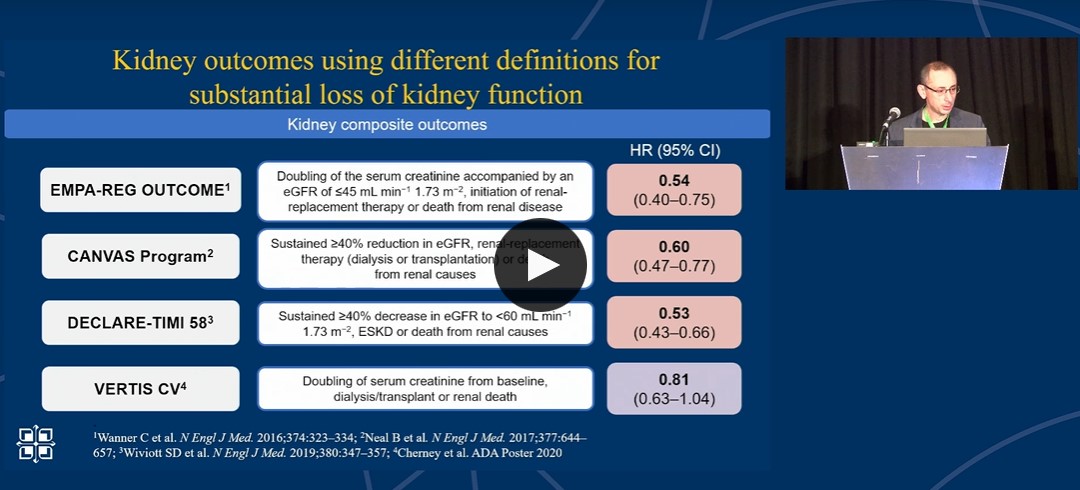
Kosiborod M gave an exciting presentation on the topic “SGLT2 Inhibitors: Renal Outcomes” under the session “SGLT2 Inhibition and Heart Failure: Translating the Evidence to Clinical Practice (CEUs)” at the HFSA Annual Scientific Meeting 2021. SGLT2 Inhibitors block SGLT-2 and reduce glucose and NA absorption.
In EMPA-REG outcome trial, eGFR decreased over time and cumulative probability of kidney endpoints were significantly lower with Emplagliflozin as compared to placebo. In EMPEROR-Reduced trial, significant eGFR slope decline was found for Emplagliflozin vs placebo. In DAPA-CKD trial, primary composite outcomes such as sustained ≥ 50% eGFR decline, ESKD, renal or CV death is significantly less with DAPA 10 mg as compared to the placebo. There is 39% reduced RRR with DAPA 10 mg as compared to placebo. Coming to the mortality, Dapagliflozin were reported to have 101 all-cause mortality events as compared to 146 events with placebo. In DAPA-HF trial, doubling of serum creatinine was observed in 43 patients of Dapagliflozin as compared to 77 patients of placebo. Cumulative incidence of composite kidney endpoints was 7.7% with Dapagliflozin as compared to 10.4% with placebo. SGLT2 inhibitors reduce progression of kidney disease, including eGFR decline and hard endpoints in T2D, HF, and CKD.
SGLT2i reduces acute kidney injury in patients with HF, CKD and in acute illness and reduce death from any cause in CKD.

