Bempedoic Acid and Cardiovascular Outcomes in Statin Intolerant Patients at High Cardiovascular Risk
Nissen SE, presented the CLEAR Outcomes Trial at the session held at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans, that evaluated whether Bempedoic acid, an ATP citrate lyase inhibitor lower the risk of major adverse cardiovascular events in statin-intolerant patients.
The CLEAR OUTCOMES trial was a randomized, placebo-controlled, double-blind trial. It enrolled 13970 patients with LDL C ≥ 100 mg/dL. Patients and providers were required to document in writing that the patient was unable to tolerate two or more statins or alternatively, a single statin if unwilling or advised not to take a second statin. The patient and provider were required to provide written confirmation that the patient was aware of the benefits of statins to reduce the risk of CV events, including death. Bempedoic acid, 180 mg daily, or matching placebo was administered to patients. The primary endpoint was a composite of CV death, nonfatal myocardial infarction (MI), nonfatal stroke, or coronary revascularization with 1620 events and ≥2 years follow-up required for completion. The first key secondary endpoint was time to the first occurrence of the composite of cardiovascular death, nonfatal stroke, or nonfatal MI with 810 events required.
The incidence of a primary end-point event was significantly lower with Bempedoic acid than with placebo (819 patients [11.7%] vs. 927 [13.3%]; hazard ratio, 0.87; 95% confidence interval [CI], 0.79 to 0.96; p = 0.004), as were the incidences of a composite of death from cardiovascular causes, nonfatal stroke, or nonfatal myocardial infarction (575 [8.2%] vs. 663 [9.5%]; hazard ratio, 0.85; 95% CI, 0.76 to 0.96; p = 0.006); fatal or nonfatal myocardial infarction (261 [3.7%] vs. 334 [4.8%]; hazard ratio, 0.77; 95% CI, 0.66 to 0.91; p = 0.002); and coronary revascularization (435 [6.2%] vs. 529 [7.6%]; hazard ratio, 0.81; 95% CI, 0.72 to 0.92; p = 0.001). Bempedoic acid had no significant effects on fatal or nonfatal stroke, death from cardiovascular causes, and death from any cause.
Bempedoic acid was well tolerated in a mixed population of primary and secondary prevention patients unable to take statins. It lowered LDL C by 21.7% and hsCRP by 22.2% with small increases in the incidence of gout and cholelithiasis. The primary end point, 4 component MACE was reduced 13%, 3 component MACE 15%, myocardial infarction 23% and coronary revascularization 19%.
The CLEAR Outcomes trial provides a sound rationale for use of Bempedoic acid to reduce major adverse cardiovascular outcomes in patients intolerant to statins.
TRILUMINATE Pivotal: A Landmark Randomized Clinical Trial of Transcatheter Tricuspid Valve Edge-to-Edge Repair for Tricuspid Regurgitation
Severe tricuspid regurgitation is a debilitating condition that is associated with substantial morbidity and often with poor quality of life. Decreasing tricuspid regurgitation may reduce symptoms and improve clinical outcomes in patients with this disease.
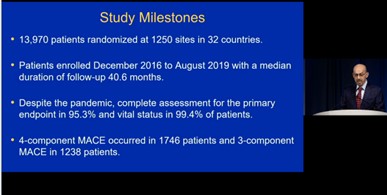
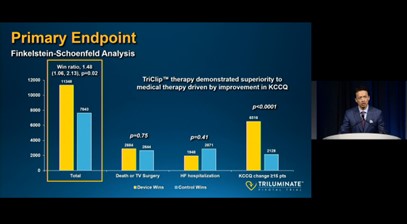
Sorajja P, presented the TRILUMINATE Pivotal study results at the session held at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans that evaluated the safety and effectiveness transcatheter tricuspid repair with the TriClip device in the symptomatic patients with severe tricuspid regurgitation who are intermediate or greater estimated risk for mortality with tricuspid valve surgery.
The Prospective, randomized, controlled, multi-center trial was the first trial to test the superiority of TriClip™ therapy in addition to medical therapy (Device group) over medical therapy alone. 450+ subjects were enrolled. The primary endpoint was a composite of mortality or tricuspid valve surgery, heart failure hospitalizations, and quality of life improvement ≥15 points assessed using the Kansas City Cardiomyopathy Questionnaire (KCCQ), evaluated at 12 months in a hierarchical fashion using the Finkelstein-Schoenfeld methodology. The secondary endpoint was assessed hierarchically in the following order: 1) Freedom from major adverse events (MAE) after procedure attempt (femoral vein puncture) at 30 days (Device group only) 2) Change in KCCQ at 12 months (superiority of Device vs. Control) 3) TR Reduction to moderate or less at 30-day post-procedure (superiority of Device vs. Control) 4) Change in 6MWD at 12 months (superiority of Device vs. Control).
TR was reduced by TriClip therapy to moderate or less in 87%, vs. only 4.8% for the control group, and reduction was sustained to 1- year follow-up. The primary endpoint was met (p=0.02) demonstrating device superiority, driven mainly by significant improvement in QOL. The degree of TR reduction was related to the degree of improvement in QOL. The 30-day MAE rate was only 1.7%, and death and pacemaker implant each occurred in 0.6%. Survival free of mortality and TV surgery was high at 1 year in both groups (~90%).
The TriClip device was highly effective in reducing TR and led to significant improvements in quality of life in one year. With the excellent benefit-to-risk profile of the TriClip system, a historically untreated population will have a treatment option to improve their quality of life.
Statins To Prevent the Cardiotoxicity from Anthracyclines: The STOP-CA Trial
Anthracyclines are a key component of several cancer regimens. The administration of anthracyclines is associated with a reduction in left ventricular ejection fraction (LVEF) leading to clinical heart failure. The retrospective data support the hypothesis that statins may reduce the cardiotoxicity of anthracyclines.
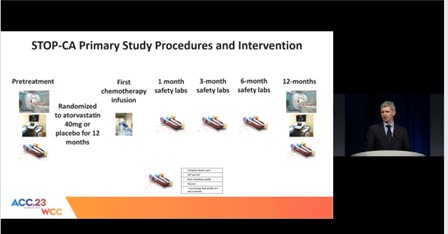
Neilan TG, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans, that discussed the results of STOP-CA study which evaluated the effect of Atorvastatin, compared to placebo, on the occurrence of cardiac dysfunction among patients with lymphoma being treated with anthracyclines.
The STOP-CA study is a multicenter, randomized, double-blind, placebo-controlled trial. 300 patients with either lymphoma (Hodgkin’s or Non-Hodgkin’s) was scheduled to receive anthracycline-based chemotherapy. Patients were randomly assigned in a 1:1 ratio to receive Atorvastatin (40 mg) or placebo starting prior to anthracyclines and continued for 1 year. The primary endpoint was the proportion of patients in each group with a ≥10% reduction in the LVEF to less than 55% within the first year of therapy. A secondary endpoint was the absolute LVEF in each group at follow-up, adjusted for the baseline LVEF.
At baseline, among the entire cohort, the LVEF was 63±4.6%. In total, 286 participants (95%) completed the trial. At 12 months, among the entire cohort, the LVEF was 59±5.9%. At 12 months, among the entire cohort, 46 participants (15%) had a decline in the LVEF of ≥ 10% from prior to chemotherapy to a final value of < 55%. Adherence with study drug was documented in > 90%. The incidence of the primary endpoint at 12 months was 9% in the atorvastatin group and 22% in the placebo group (p=0.002). The incidence of this secondary endpoint was 13% in the atorvastatin group and 29% in the placebo group (p=0.001).
For the participants with lymphoma who were treated with anthracyclines, the prophylactic use of Atorvastatin over 12 months was associated with a lower rate of cardiac systolic dysfunction.
Impact of Heart Failure Management Using Thoracic Fluid Monitoring from A Novel Wearable Sensor: Results of The Benefits of Microcor (μCor™) in Ambulatory Decompensated Heart Failure (BMAD) Trial
Despite advances in medical and device therapy, heart failure (HF) remains a disease characterized by frequent hospitalization.
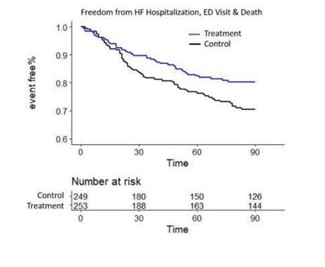
Boehmer J, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans, that discussed the efficacy analysis with the use of thoracic fluid index (TFI) monitoring using a novel radiofrequency-based sensor in the BMAD trial.
The BMAD trial enrolled subjects from clinical sites in the US and Europe over 45 months. All subjects were asked to wear the μCor system for 90 days and were assigned by site into a control group with investigators were blinded to TFI and a treatment group using TFI to guide HF therapy. The endpoints of the study were investigator engagement of μCor system data in the context of HF management in the treatment subjects with an objective to evaluate HF emergency visits (ER) and hospitalizations or death, reported here by Kaplan-Meier analysis as time to first event.
A total of 522 subjects were enrolled with 502 receiving the device and included in this intent to treat analysis. Subjects are characterized as 55% HFpEF, 42% female, age 68 ± 13 years, 53% non-ischemic. There were 42 treatment subjects with a HF event compared to 63 control subjects representing a 36% reduction in HF events (HR = 0.64; p=0.02).
HF management using TFI results in a 36% reduction in HF ER visits and hospitalizations or death.
My Way or the Highway: Surgical and Cath Controversies in Congenital Heart Disease
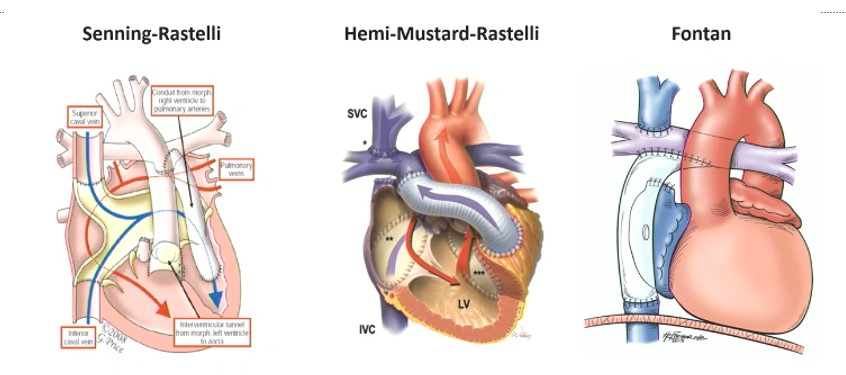
Muniz J and Gearhart A, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans that discussed two cases. Fontan physiology can have long-term effects such as fontan pathway disruption, collateral shuts, arrhythmias, pleural effusion, hepatic fibrosis or malignancy, renal insufficiency, stroke, thrombophilia, thyroid disease, etc and the factors impacting biventricular repair are dextocardia/mesocaria, coronary artery anomalies, atrioventricular valve hyperplasia and/or significant straddle, etc.
Although a biventricular approach may seem preferable, it is an inappropriate candidate which is associated with significant mortality as well as pulmonary hypertension, valvar dysfunction, and LV systolic and diastolic dysfunction and the treatment options are limited for these co-morbidities. History of endocardial fibroelastosis and smaller LV stroke volume/BSA are independent factors associated with adverse outcomes among patients with borderline hypoplastic left heart undergoing biventricular conversion.
Borderline heart is a heterogeneous mix of unbalanced AVC, coarctation and VSD, complex transposition of great arteries, upstairs downstairs ventricles, and double inlet ventricle. The modified paradigm of borderline heart consists of single ventricle palliation and primary biventricular repair. Single ventricle palliation can either move towards or Fontan or staged ventricular recruitment.
Surgical approach is the mainstay therapy for sinus venous ASD and bicaval canulation and cardiac arrest can be managed by pump repair. In the Warden procedure, pulmonary veins enter high in SVC and SVC entry into RA baffled across sinus venous defect and SVC reimplanted into RA appendage. The best management strategy for sinus venous ASD should be applicable to entire cohort, widely available, easily executed, low morbidity/mortality with minimally invasive approach and excellent long-term profile. Sinus venous defects can be closed by catheter by planning, assessing morphology, selection of appropriate stents and balloons, and technique details to deliver these in correct positions.
In conclusion, one bad decision can impact transplant eligibility and can result in end-organ dysfunction and increased potential for sensitization. An individualised approach is most prudent.
Effect of Remogliflozin on Biomarkers Compared to Empagliflozin Inpatients of Type 2 Diabetes Mellitus with Chronic Heart Failure
SGLT2 inhibitors reduce heart failure hospitalisation and N-terminal pro-brain natriuretic peptide (NTproBNP) levels in HF.
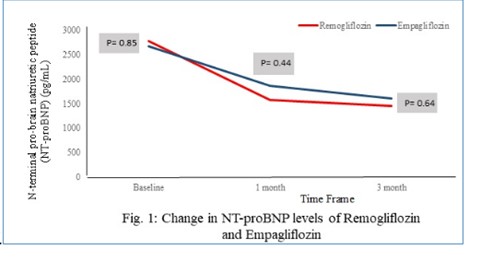
Sengupta S, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans, that evaluated the effect of Remogliflozin in patients of T2DM with CHF as compared to Empagliflozin using NT-proBNP as index of therapeutic effects.
In this multicentric, prospective study, 71 patients of DM with CHF (EF<40%) with NTproBNP>600pg/ml were included. 38 patients were in Remogliflozin (R) group and 33 in Empagliflozin (E) group. Baseline demographic, glycaemic, cardiac and renal parameters were comparable between 2 groups (p>0.05).
Mean NT-proBNP level improved from baseline to 3 months in both groups (R group: 2781±2695 to 1451±1183 pg/ml, p=0.0007); (E group: 2672±2181 to1602±1436 pg/ml, p=0.004) respectively, but no significant difference was seen between two groups (p= 0.64, Figure 1). Mean HbA1c was 7.87±1 at baseline and improved to 7.58±1.3 at 3 months in R-group; 7.78±0.1 at baseline and improved to 7.44±1.2 at 3 months in E-group. The mean eGFR was 75.6±27.4 at baseline and 81.7±28.4 at 3 months in R-group; 78.1±21.3 at baseline and 71.7±22.9 at 3 months in E-group. Systolic BP reduced from 127±21 mmHg at baseline to 123±14 mmHg at 3 months in R group (p<0.05). No adverse events occur in either group.
Remogliflozin improved glycaemic parameters and NTproBNP as an index of therapeutic effects in T2DM patients with CHF. Remogliflozin was well tolerated and non-inferior to Empagliflozin in T2DM patients with CHF.
Navigating the Post Pandemic Staffing Crisis: The Way Forward for Cath Labs
Welt F, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans. Health care employment fell by 17,500 jobs in September, with losses in hospitals (-8100 jobs) and nursing residential care settings (-37,000 jobs) outweighing gains in ambulatory care settings (-28,200 jobs). Revisions through July were modest, adjusting total health care jobs up by 7,000. Compare to the Feb 2020 pre-pandemic peak, employment in ambulatory care settings has almost completely returned, at about 5000 fewer jobs (-0.1%), while hospitals employ 93,000 fewer jobs (-1.8%). Overall healthcare employment in 5,24,000 jobs (3.2%) below the February 2020 pre-pandemic peak. Total employment remains about 5 million jobs, or 3.3%, below pre-pandemic levels. The unemployment rate fell to 4.8%.
The possible reasons for the crisis are:
- Enduring attempts to control the public health crisis
- Fiscal visibility of small and large healthcare systems that can be related to temporary closure of outpatient clinics, limitation of elective cases. There were large downstream effects on new staffing hires, budgets and retention
- Personal decisions of individuals leaving the healthcare sectors with early retirement or job/career transitions. The factors of health or family or childcare were also considered
The layered strategies can be applied for the society, state and federal layer, administrative layer and individual clinician layer such as improve awareness and advocacy initiatives to address the crisis, commit to re-evaluate rewards philosophy, implementing innovative training pathways to provide more health care workers i.e., RN, RT, echo techs etc. make workforce health and well-being a priority, resiliency, emotional support and recovery. The staff should be leveraged. Flexibility/care model redesigns should be introduced. The academic partnerships should be strengthened to build the pipelines and re-instill hope and focus on path forward.
Clinical Trial Recruitment: Challenges and Solutions in the COVID Era
Davidson LJ, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans that discussed the challenges to clinical enrolment and their solutions in COVID times. The challenges we faced to clinical trial enrollment on a good day are:
- Identifying objects
- Inclusion of diverse patient populations
- Follow up
- Meeting pre-specified recruitment numbers
- Interpreting data and drawing conclusions
These leads to inadequate power, inability to reach primary endpoints, cofounding variables, biased samples and inability to generalize results and need for protocol modifications. In fact recent survey shows that 47% of valve disease patients DO NOT get information on clinical trials that may might be eligible for. 63.7% of patients stated that they received their information about clinical trials form somewhere other than a doctor, surgeon or their hospital. It can be say that we may missing the opportunities to recruit the patients into trials. COVOD-19 exacerbated already existing inequalities in clinical trial participation.
The lesson learned from the pandemic with clinical trial recruitment are
- Virtual visits are feasible and patients are willing to adopt to this
- Research protocol should have prospective contingency planning
- Consider opt-out strategies
The important considerations for clinical trial enrollment should be implemented are referral base and relationships should be build. Leverage your website to recruit patients directly, highlight the educational programmes and social media, direct referral Apps for physicians can be given to use.
Clinical trial recruitment presents many challenges, which are only exacerbated during a pandemic. Novel methods of interacting with patients i.e., virtual visits, addressing unique concerns of patients during pandemic, follow up and data analysis are imperative. The key to method is maintaining a strong referral basis and diversifying the methods by which you are accessible for referrals.
Time to Get Green – Managing Cath Lab Utilization and Waste
Ahmed B, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans which explore the Cath lab and waste management. Why we need a greener Cath lab practice is
- To reduce wasteful practices and optimize utilization
- For the cost savings
- To make better climate change
- Its stronger impact on healthcare system
Climate change is considered to be the biggest threat to human civilization in the 21st century and environmental pollution is a cardiac risk factor to people. Global healthcare system is the 5th largest contributor to global GHG emissions. US healthcare system is leading the charge-US healthcare output is greater than the output of all sectors in the UK. US healthcare system is responsible for 10% of US GHG emissions. The Cath lab sustainability team should be establish with nurses, Techs, Cath Lab manager, students, trainees, Physicians. The Cath lab sustainability plan can be outlined by assessing the existing process and identifying ways to limit landfill waste. Systemic changes should be made across the spectrum of utilization. The ways to reduce, reuse and recycle products should be identified and periodic re-assessment of output is necessary.
Life cycle assessments and other industrial ecology procedures and tools, such as circular economy, can be used to furthermore evaluate healthcare services at multiple levels, incorporating: global supply chain, national healthcare systems, whole hospital/health systems, clinical pathways and procedures, in- dividual drugs, medical devices, and basic materials. A healthcare-specific industrial ecology framework that merges top-down (macro scale) and bottom-up (micro scale) approaches is required, to review clinical activities, and to enhance the general use of research that pursue to guide execution attempts and track health- care environmental performance development.
From Heresy to Necessity: Same Day Discharge for TAVR – How We Do It
Cohen MG, presented a session at the American College of Cardiology (ACC) on 4th March 2023, at New Orleans. The key points to be considered for the same day discharge (SDD) of patients are:
- Patient and environmental factors
- Procedural factors
- Complications
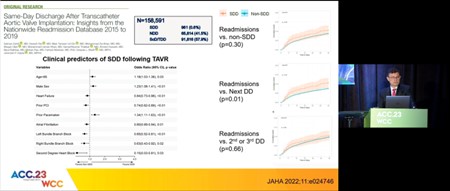
JAHA 2022 paper stated the insights from the nationwide readmission database of SDD patients after transcatheter aortic valve replacement (TAVR) from 2015 to 2019. Total 158, 591 patients were included in the study in which only 9.6% patients had SDD and 41.5% patients were non-SDD while 57.9% patients were ScD/TDD (second‐ or third‐day discharge). The SDD patients showed higher rate of readmissions as compared to non-SDD patients (p=0.30). The next day discharge (NDD) and ScD/TDD patients also had high rate of readmissions than non-SDD patients (p=0.01, p=0.66 resp.)
In wood D, et al. JACC 2019 paper, the Vancouver 3M clinical pathway is implemented for NDD patients in which 1400 patients were screened, 411 patients were enrolled at 13 centers. 80% of patients were discharge on next day. 5.7% patients had PPM implantation and 0.24% patients required late heart block PPM. The 3M-TAVR Economic study showed similar clinical outcomes between 3M TAVR and S3i Registry. Also, 3M-TAVR approach showed lower 30-day costs as compared to S3i. Programme implementation involves the steps of a QI process i.e., pathway development, evaluation and modification. SDD decisions are based on individualized team discussions at patient bedside.
SDD patients are highly selected because of lower risk, uncomplicated TF procedures, high THV implantation technique and without conduction abnormalities. Majority of patients in published series treated with SE THV. Economic considerations will reduce hospital costs and improve hospital margins. However, it may lead to lower payment by Medicare.

