Cardiovascular 2022 Heart Failure Guidelines… What is Needed in 2023 and Beyond to Ensure Equitable Care for All Patients?
Yancy CW, presented a session at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans, that evaluated 2022 HF guidelines in comparison to recent 2023 guidelines. There are four pillars are present for the treatment of HFrEF are:
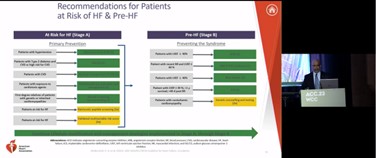
- At risk of HF (Stage A)
- Pre-HF (Stage B)
- Treatment of HFrEF Stage C
- Treatment of HFrEF Stage D
In Stage A, blood pressure should be controlled in accordance with GDMT for hypertension to prevent symptomatic HF in patients with hypertension. In patients with type 2 diabetes and either established CVD or at high cardiovascular risk, SGLT2i should be used to prevent hospitalizations for HF. In Stage B, in patients with LVEF ≤40%, ACEi should be used to prevent symptomatic HF and reduce mortality. In patients with a recent or remote history of MI or ACS, statins should be used to prevent symptomatic HF and adverse cardiovascular events. New treatment strategies in HF, including sodium-glucose cotransporter-2 inhibitors (SGLT2i) and angiotensin receptor-neprilysin inhibitors (ARNi) are added in stage C. In patients with advanced (stage D) HF refractory to GDMT and device therapy who are eligible for and awaiting MCS or cardiac transplantation, continuous intravenous inotropic support is reasonable as “bridge therapy”.
In patients with HFpEF, SGLT2i, MRAs, ARB, ARNi may be considered particularly among patients with LVEF. In patients with HFimpEF after treatment, GDMT should be continued to prevent relapse of HF and LV dysfunction, even in patients who may become asymptomatic.
The 4 pillars of medical ethics are:
- The pillar of beneficence
- The pillar of non-maleficence
- The pillar of autonomy
- The pillar of justice
The pillar of beneficence is about promoting the good for others. In medicines mean acting in a way that helps your patients. Non-maleficence refers to not causing harm to your patients. The pillar of autonomy refers to patient’s right to make their own healthcare decisions known as self-determination. The principle of justice refers to fairness with medicine and equal distribution of resources.
Four pillars of therapy plus the four pillars of ethics are the path to health equity in heart failure.
Determining Cost and Value in Heart Failure Therapy
Allen LA, presented a session at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans. Heart failure is typically chronic and associated with multimorbidity, where multiple new treatments in recent years have been shown to improve survival but also add significant burdens and cost for patients. Understanding the totality of patient (and family caregiver) costs is related to management is critical to delivering patient-centered, high value care that maximizes health outcomes and patient experience.
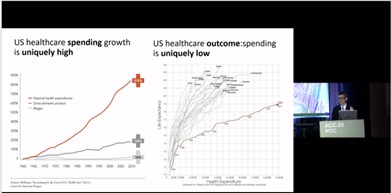
The most important word or concept in medicine is value. As per 2011 survey data, US healthcare spending growth is uniquely high with increasing national health expenditures by 81.8% while healthcare outcome i.e., life expectancy is uniquely low. This shows that US healthcare has low value.
Financial toxicity is defined as problems a patient has related to the cost of medical care. In medical expenditure panel survey 2014-2018, for those with HF, 33% patients reported financial hardship due to medical bills and 13% patients were not able to pay bills at all. In Markov model that stimulated monthly outcomes based on results from the EMPEROR-Preserved and DELIVER trials, adding SGLT2i to standard therapy is projected to cost $141200 per quality adjusted life year gained. An SGLT2i would not be cost effective if there is no mortality benefit.
OOP cost is tricky to get and convey and it depends on health insurance product of which there are thousands and pre-authorization. Also, other drug expenses that push patients into different copay categories during the year.
Efforts to communicate and address healthcare costs are emerging, including tailored, real-time, integrated estimates of out-of-pocket costs. Given the significant costs to patients associated with stacking of evidence-based therapies, improving equitable access to care will require improved data on the relative value of treatments as well as changes in healthcare policy and financing.
Rapid Simultaneous Initiation of HFrEF Quad Therapy is the Best Approach to Ensure Optimization of Medical Management
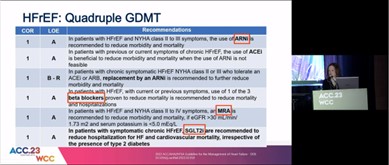
Vardeny O, presented a session at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans. Comprehensive guideline directed medical therapy (GDMT) extends lives and reduces hospitalizations as compared to conventional therapy. In 55-year-old patient, ARNI+βB+MRA+SGLT2i are estimated to extend event free survival by 8.3 years vs. ACEI+ βB alone. In patients with HFrEF, Quadruple GDMT i.e, ARNI, beta-blockers, MRA and SGLT2i are recommended. In patients with symptomatic HFrEF, SGLT2i are recommended to HHF and CV mortality, irrespective of presence of T2DM.
Benefits of certain GDMT accrue early and delaying initiation exposes patients to potentially avoidable risk. Packer et al., 2014 paper showed the early benefit of Sacubitril/Valsartan over Enalapril. In JAMA 2021 study, Dapagliflozin showed clinical benefit with significant reduction in risk of primary efficacy outcome of HHF and CV death or worsening HF by 4 weeks. In DELIVER trial, Dapagliflozin showed significantly lower primary endpoint as compared to placebo. Each therapy has a treatment effect independent prior initiation (or dose) of other therapies, and may enable use of other GDMT. In PARADIGM-HF study, Sacubitril/Valsartan showed similar benefit irrespective of beta-blocker use or dose. Also, Sacubitril/Valsartan showed lower CV death in patients treated with MRA. Sacubitril/Valsartan did not lead to discontinuation of GDMT and may facilitate sustained use of MRAs due to stabilization of kidney function and potassium compared with enalapril. Empagliflozin was associated with a 22% reduced risk of MRA discontinuation post randomization as compared to placebo. Severe hyperkalemia was less common in the Empagliflozin group.
GDMT and HFrEF consists of 4 medication classes, with evidence to support early clinical benefit after initiation. No biologic rationale is suggested for waiting to add therapies until full dose achieved of prior therapy. Earlier use of ARNI and SGLT2i may enable sustained use of MRA. More research is needed on optimal strategies for rapid simultaneous initiation of quadruple GDMT.
Step by Step Initiation of HFrEF Quad Therapy is the Best Approach to Ensure Optimization of Medical Management
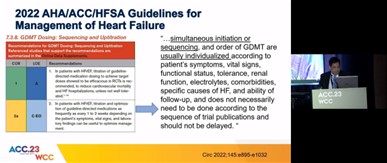
Aguilar D, presented a session at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans. As per Biegus, et al., 2022 study, in treatment of patients with HFrEF, today’s challenge is that too many people with HFrEF remain untreated and experience treatment delays with medications that extend survival and prevent worsening HF. There is clear need to improve initiation, titration and adherence of GDMT for all patients living with HF. 2022 AHA/ACC/HFSA guidelines for management of HF recommended that simultaneous initiation or sequencing and order of GDMT are usually individualized according to patient’s symptoms, vital signs, functional status and dose not necessarily need to be done according to the sequence of trial publications and should not be delayed.
HFrEF trials were performed sequentially and on background of optimal HF therapy predominantly in ambulatory patients. Acute HF trials added an individual therapy after hemodynamic stability and most patients on background therapy. HF guidelines leave open the question of how to initiate and sequence therapies. A personalized approach is suggested based on patient profiling/characteristics and potential adverse effects of the HF medication. Sequential therapy allows for personalization and shared decision making with the patient (right drug in right patient at the right time). Allen A, et al., 2022 study stated that GDMT should be initiated and intensified in a sequence that priorities meds with the greatest expected benefit and drawing on areas where the patient has ample reserves.
An evidence gap exists for how best to initiate and sequence HFrEF quad therapy. Sequential initiation allows for personalization based on patient characteristics, medication factors and allows for shared decision making. Nonetheless, underutilization and delayed treatment with lifesaving HFrEF pharmacotherapies must be improved. It is critical to identify improvement strategies i.e., GDMT titration clinics, HER interventions, telehealth, multidisciplinary HF management programs, electronically administered patient awareness tools.
Controversies at the Intersection of Structural Heart Disease and Cardiac Electrophysiology Management of Atrial Fibrillation After PFO Closure
Patent Foramen Ovale (PFO) is present in 25% of adults. Its prevalence is higher with cryptogenic CVA. If the stroke is due to a paradoxical embolism, it is likely to carry a significant risk of recurrence.
Baykaner T, presented a session held at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans that discussed the management of Atrial Fibrillation after PFO closure.
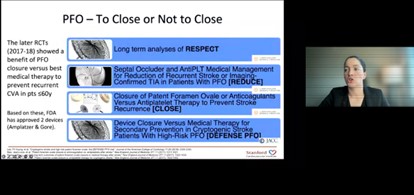
The early RCTs between 2012-13 failed to meet the primary efficacy point but the later RCTs in 2017-18 like RESPECT, REDUCE, CLOSE, DEFENSE-PFO trials showed a benefit of PFO closure versus best medical therapy to prevent recurrent CVA in patients ≤60 years.
The SCAI guidelines for the Management of Patent Foramen Ovale:
|
Conditional recommendations FOR PFO closure
|
Conditional recommendations AGAINST PFO closure
|
|
In patients >60 years with a prior PFO-associated stroke |
In patients with AF who have had an ischemic stroke |
|
In persons with platypnea-orthodeoxia syndrome (POS) and without a prior PFO-associated stroke |
In persons experiencing migraine without a prior PFO-associated stroke |
|
In persons with systemic embolism and without a prior PFO-associated stroke |
In persons with TIA and DVT without a prior PFO-associated stroke |
The onset of AF after the closure of PFO was noted in earlier studies. PFO closure in patients with CVA attributable to PFO and paradoxical emboli, to avoid the use of OACs. The concurrent presence of AF would render the transcatheter PFO closure redundant, as patients would have an ongoing indication for OAC. Monitoring extensively (i.e., ILR) for AF in patients with cryptogenic CVA and PFO can detect AF in >10% of the patients who otherwise would have undergone PFO closure.
There is a potential procedure-related higher incidence of AF after PFO closure mostly reported in the first 4-6 weeks, which may subside long-term, and may not necessitate life-long OAC.
New Onset LBBB with Normal EF After TAVR
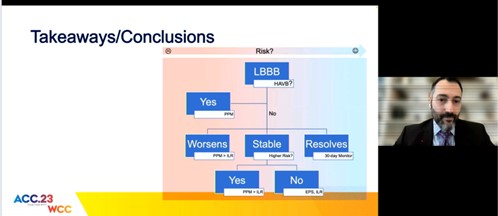
Left bundle branch block (LBBB) is a common complication contributing to approximately 20-25%. Majority will resolve after POD1.
Kiani S, presented a session held at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans, and discussed the associated risk of LBBB after TAVR and ancillary risk factors for HAVB/CHB.
Approximately 15%-31% are associated with HAVB/CHB, the majority are asymptomatic and are also associated with new PPM. The risk of Sudden Cardiac Death (SCD) is up to 3.2%. The risk factors for the persistence of LBBB are absolute QRS width and implant depth. The risk factors for HAVB were wider QRS and chronic kidney disease. Risk stratification was conducted. 708 patients having TAVR out of that 180 (25%) have LBBB after TAVR. The utility of EP study showed HV ≥ 70ms and 44% sensitivity. The QRS was >150 or PR was > 240. The ambulatory rhythm monitoring showed a rate of AVB in 10%-25% and a rate of SCD in 1%-1.3%. It is still unclear who is truly low risk.
Patients at highest risk show:
- QRS > 150
- Abnormal HV
- Low implant death
- Worsening condition on EKG
It is unclear who is at low risk. Local factors should be considered while evaluating.
Transvenous Leads Should Be Extracted Before Percutaneous Tricuspid Valve Replacement -Con Jailing is Safer Than Extraction
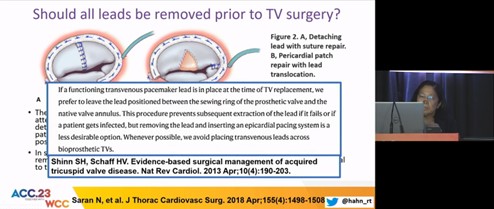
The most common mechanism leading to pacemaker-induced tricuspid regurgitation was restricted leaflet mobility, followed by adherent leaflet to the leads, leaflet perforation, scarring of leaflets, and chondral entrapment. The pacemaker-induced tricuspid regurgitation was found to be protective compared to pacemaker-associated TR with improved survival (hazard ratio [HR 0.76;95% confidence interval [CI], 0.68-0.98)
Hahn R, presented a session held at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans that discussed whether transvenous leads should be extracted before percutaneous tricuspid valve replacement -con and the benefits and risks of jailing over-extraction
The approach to removing leads prior to TV surgery varied with individual surgeons. The repair was attempted when the valve was not extensively damaged. The B. Pfannmueller et al. study suggested that patients with pre-existing PPL, who require TV surgery for significant TR without evidence of PPL-induced TR, can undergo TV repair without removal of the PPL. In tricuspid regurgitation following TLE a clinically significant increase in TR was noted in 5.6% patients (n=124), removal of ≥ 2 leads and powered sheath-assisted extraction were significantly associated with an increase in TR score. The Park SJ et al study reported a significant acute TRI in 11.5%. The European Lead Extracted Controlled (ELECTRa) study showed a higher risk of major complications or death in TR patients, with TLE. The Anderson TL et al study showed that TTVR in the setting of trans-TV pacemaker leads without lead extraction or re-replacement can be performed safely with a low risk for complications, offering an alternative to surgical TV replacement. The risk of CIED-related infection in jailing is estimated to be 4.7 per 1000 person-years.
The benefits of jailing were avoidance of TLE complications and extraction was noted as avoidance of complications of jailing. The complications associated with jailing were endocarditis, CIED dysfunction, and TTVR complication. The complications associated with extraction were venous injury, tricuspid valve injury, cardiac avulsion, and death.
A Randomized Trial of A Personalized Clinical Decision Support Intervention to Improve Statin Prescribing in Patients with Atherosclerotic Cardiovascular Disease (PCDS Statin)
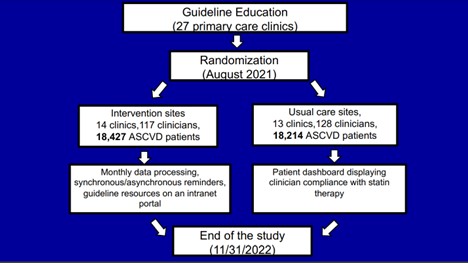
High-intensity statin (HIS) use remains low in patients with atherosclerotic cardiovascular disease (ASCVD) despite guideline recommendations. Reasons include therapeutic inertia (TI) and statin-associated side effects (SASE). Do personalized reminders targeting TI or SASE improve HIS use in ASCVD patients?
Virani S.S, presented a session held at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans evaluated whether personalized reminders improve HIST use.
In a randomized clinical trial in the Department of Veterans Affairs, an intervention was developed by constructing machine learning algorithms that use structured and unstructured data via natural language processing (NLP) to identify SASEs and by performing qualitative interviews to determine patient and clinician perspectives on SASEs and clinician information needs. The intervention included centrally processed reminders individualized to each patient and sent to primary care clinicians 2-7 days before the patient visit. Information included the date and type of ASCVD diagnosis, statin, and dose, date of last statin fill, date and type of any SASE, and guideline resources on HIS definition and SASE management. Usual care included access to the patient dashboard with statin guideline compliance assessments. After guideline education, 27 primary care clinics were randomized: 14 to the intervention (117 clinicians, 18,427 ASCVD patients) and 13 to usual care (128 clinicians, 18,215 ASCVD patients). Outcomes include a pre-post change in HIS (primary) and statin (secondary) use between intervention and usual-care sites.
Baseline HIS/statin use at intervention and usual-care sites was 52.6%/81% and 55.6%/82.2%, respectively. In the intervention arm, the algorithm identified SASEs in 23% of patients; individualized reminders on 5156 patients have been delivered to date. The trial began in August 2021 and will end in November 2022.
Centrally controlled reminders allowed rapid upscaling of the intervention to several sites. The study results informed how informatics-driven interventions can improve evidence-based care delivery in large healthcare system.
Building Electronic Tools to Enhance and Reinforce Cardiovascular Recommendations for Heart Failure (BETTER CARE-HF): A Pragmatic, Cluster-randomized Trial Comparing Two Ambulatory Clinical Decision Support Tools
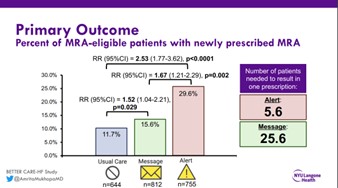
Approximately 68,000 preventable deaths occur every year due to shortfalls in prescribing of proven therapies for heart failure with reduced ejection fraction (HFrEF), particularly mineralocorticoid receptor antagonists (MRA). Electronic clinical decision support (CDS) is a low-cost, scalable approach with the potential to improve prescribing, but optimal CDS format and timing in the ambulatory cardiology setting are unknown. Using an established CDS framework, semi-structured interviews, and pilot testing two targeted CDS tools were developed that notify cardiologists of patients in their care who were eligible for MRA therapy: 1) a best practice alert (BPA) that notifies cardiologists during individual visits, and 2) a monthly in-basket message that allows for review of multiple patients between visits
Mukhopadhyay A, presented the BETTER CARE-HF Trial at the session held at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans that evaluated the effectiveness of an electronic alert vs. message vs. usual care to improve prescribing of HF therapy.
BETTER CARE-HF is a three-arm, pragmatic, cluster-randomized trial comparing the effectiveness of the alert vs. message vs. usual care on the primary outcome of MRA prescribing. Key secondary outcomes include time to prescription and provider engagement with CDS (e.g. actions taken). The adults included were with EF≤40%, outpatient cardiology visits, and no active MRA prescription. The patients with systolic blood pressure (SBP)5.1 mmol/L, any potassium ≥5.5 mmol/L, most recent glomerular filtration rate (GFR) ≤30 mL/min/1.73m2, or documented MRA intolerance were excluded. Patients were cluster randomized by cardiologists across a large health system (>50 practices, 180 cardiologists [60 per arm]).
Overall, 1,859 patients were randomized, of whom 70.8% were male, 68.7% White, 81.4% non-Hispanic, and 84.9% English speaking. The median age was 73. The average EF was 33%, with average potassium of 4.3 mmol/L, GFR 68 mL/min/1.73m2, and SBP 123 mmHg. Primary and secondary outcomes will be presented.
BETTER CARE-HF is the first study to directly compare the effectiveness of an alert vs. message to improve prescribing. Our findings can be rapidly disseminated with the potential to improve morbidity and mortality for patients with HFrEF, and can also inform the development of future CDS interventions for other diseases.
Atrial Pacing for Heart Failure with Preserved Ejection Fraction: A Randomized Clinical Trial
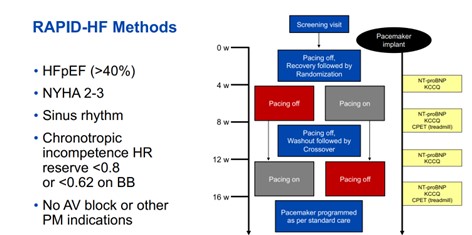
Reduced heart rate (HR) during exercise is common in patients with heart failure with preserved ejection fraction (HFpEF) and associated with reduced aerobic capacity, but it remains unknown if restoring exertional HR through pacing would be beneficial.
Barry A, presented a session held at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans and reported the implantation of a cardiac pacemaker to increase exercise HR is not effective to improve submaximal or peak exercise capacity or functional status in patients with HFpEF and chronotropic incompetence.
Single-Center, Double-Blinded, Randomized, Cross-Over Trial testing the effects of rate-adaptive atrial pacing on the primary endpoint of Oxygen Consumption (VO2) at anaerobic threshold (VO2,AT) and secondary endpoints of peak VO2, ventilatory efficiency (VE/VCO2 slope), patient-reported health status by the Kansas City Cardiomyopathy Overall Summary Score (KCCQ-OSS), and N-Terminal Pro-B-Type Natriuretic peptide levels in patients with HFpEF and chronotropic incompetence.
A total of 32 patients were recruited and 29 underwent pacemaker implantation and were randomized to atrial rate responsive pacing or no-pacing first for 4 weeks, followed by 4-week washout period, and then cross-over for an additional 4 weeks. In the absence of pacing, peak VO2 and VO2 at anaerobic threshold (VO2,AT) were both correlated with peak exercise HR (r=0.46-0.51, both p0.27 for all). Atrial pacing was associated with a decrease in O2 pulse (p=0.002), which may have mitigated any gains in exercise performance
The present study provides strong evidence that implantation of pacemakers to increase exercise heart rate is ineffective to improve functional status in patients with HFpEF and chronotropic incompetence. These results challenge our current understanding of chronotropic incompetence in HFpEF, and suggest that a lower-than-expected peak HR is a consequence of premature exercise cessation rather than a cause of exercise limitation.
Translating Polygenic Risk for Coronary Artery Disease into Clinically Actionable Information Using Causal A.I.
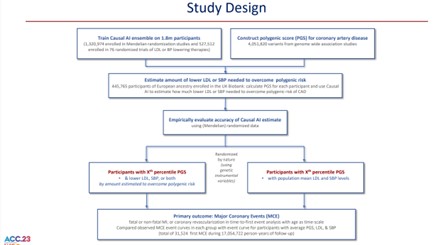
A polygenic score (PGS) measures a person’s inherited risk for coronary artery disease (CAD), but it is unclear how this information can be used to inform clinical care.
Ference BA, presented a session held at the American College of Cardiology (ACC) on 5th March 2023, at New Orleans that determined how much each person must lower their LDL, SBP, or both to overcome their inherited polygenic risk for CAD using Causal AI.
The PGS consisting of 4,051,820 variants was used to estimate the lifetime risk of major coronary events (MCE: fatal or non-fatal-MI; or coronary revascularization) among participants in each decile of the PGS. Then a causal AI algorithm was used that integrates information from Mendelian randomization studies and randomized trials to estimate the reduction in LDL or SBP needed to reduce risk among participants in each decile of PGS to the same level as participants with average PGS. These estimates were validated by comparing the observed event curves in each group.
Among 445,774 participants (54.1% women) followed to a median age of 70.9 years, 31,524 participants experienced a first MCE during 17,054,722 person-years of follow-up. For the vast majority of participants, the polygenic risk for CAD was overcome with small lifetime reductions in LDL and SBP (FIGURE). However, the amount of LDL or SBP lowering needed to overcome polygenic risk increases the later LDL or SBP lowering is initiated.
Causal AI can translate a PGS for CAD into clinically useful information by quantifying how much each person must lower their LDL or SBP to overcome their inherited polygenic risk for CAD.

