Artificial Intelligence: New Ways of Diagnosing Valvular Heart Disease
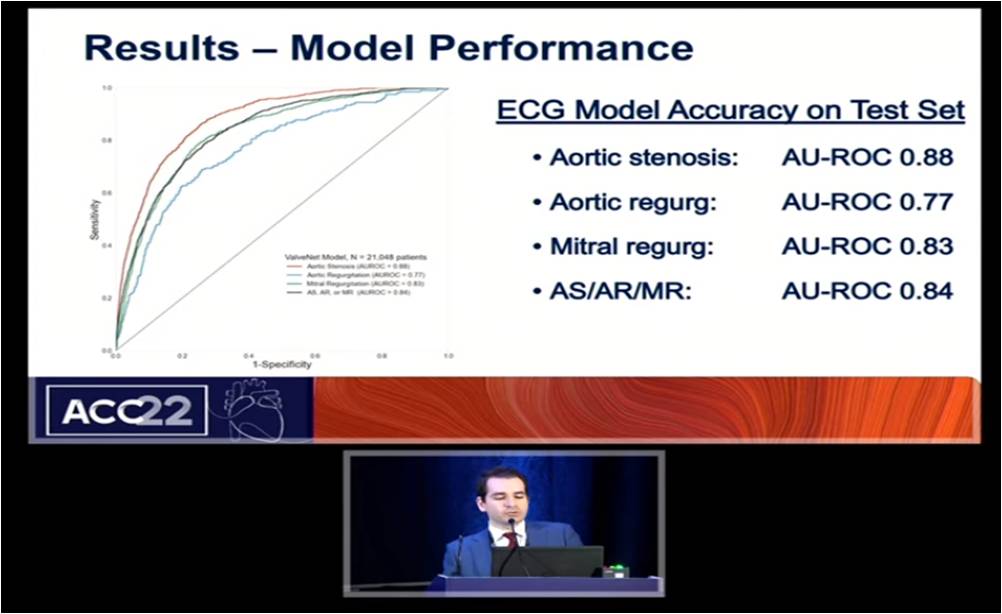
Elias P, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022. Artificial intelligence (AI) often seeks to match MD performance. Electrocardiograms (ECGs) are not diagnostics for aortic stenosis (AS). Cardiologists can’t detect AS from just an ECG. The ECGs were done on patients with echocardiograms and generate labels to diagnose what a human expert cannot. The objective of the study was to develop a deep learning model which analyses ECGs to detect patients with left-sided moderate or severe valvular heart disease (VHD) as determined by echocardiography. Total 617,564 ECGs were performed <1 year prior to echocardiography in 114,215 patients. After excluding 342,509 ECGs, 2,21,255 ECGs were conducted on 43,165 patients in multisite train and one ECG per patient was conducted in multisite validation, multisite train and holdout site test. The ECG model accuracy on test set was AU-ROC 0.88 for aortic stenosis, 0.77 for aortic regurgitation, 0.84 for AS/AR/MR. As per the screening program modeling, positive predictive value of AS,AR, or MR was inversely correlated to sensitivity of model. Saliency mapping determines what features the model uses to make predictions. Red line in the model pull towards positive results and blue line pull towards negative result. This is a true positive with aortic stenosis with the greatest activation in the QRS and T waves, less in the P waves.
Next step in the AI is taking steps to develop this technology further to detect early VHD with conduction of additional multicenter retrospective validation studies and actively enrolling a 200 patient prospective diagnostic trial in patients with no history of VHD. Also, it is developing single lead models for POC testing options. It built the first soup-to- nuts tutorial IntroECG to get deep learning with cardiac data and imaging.
Guidelines for Hypertension Management Around the Globe: The ESC/ESH Perspective
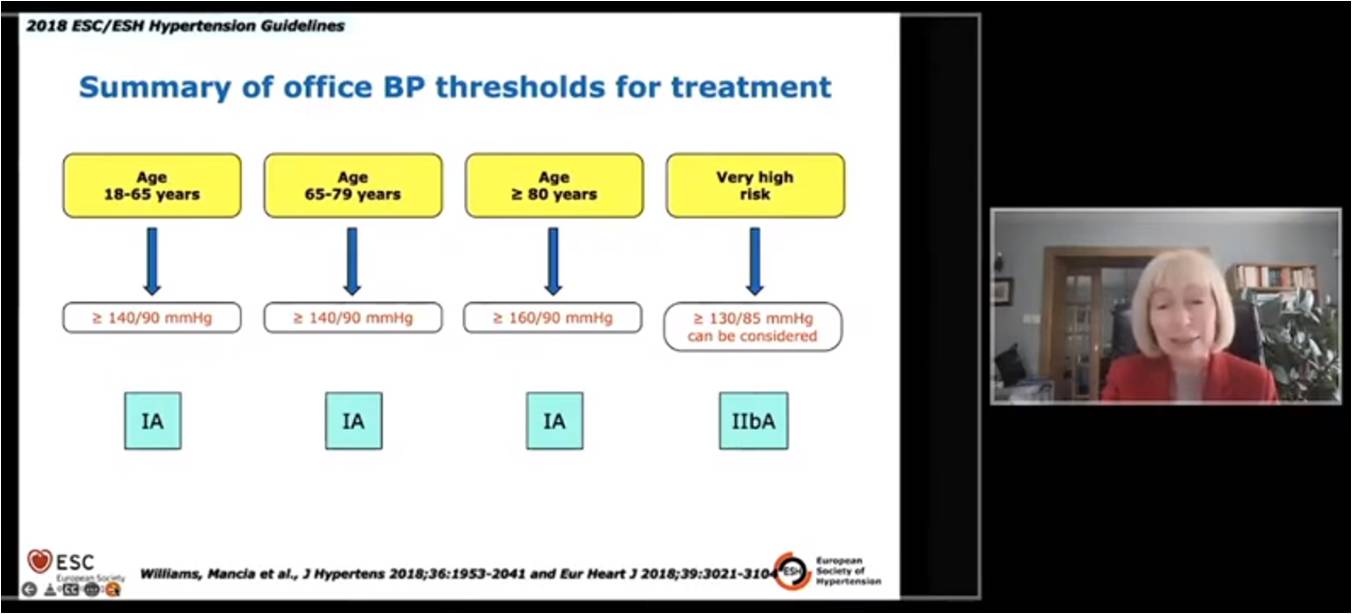
Dominicazak AF, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022. The objectives of the study were to discuss the diagnosis and role of out-office BP, organ damage, BP threshold and target for treatment, drugs and strategy of treatment. If the BP is 140/90 mmHg, repeat visits to office BP measurement or/and out-of office measurement (ABPM/HBPM) to confirm the diagnosis. Elevated ambulatory BP significantly increases the risk of CV events and mortality. Elevation in BP with organ damage significantly increases the high risk for patients to CVD. According to SCORE, SCORE ≥5% with superoxide dismutases (SOD) present substantially increase the probability of CV death as compared to SCORE ≥5% with no SOD p<0.001. In the younger age group of 18-65 years and age 65-79 years, the BP ≥140/90 mmHg is threshold to treatment. For ≥80 years group, BP ≥160/90 mmHg is considered to treatment and ≥130/ 85 mmHg is considered for very high risk group. According to RT-based meta analyses, lowering SBP to <130 or DBP to <80mmHg significantly reduces the risk of all CV events and CV-cause death. The office BP treatment target range for all age group should be first SBP <140 mmHg and aim for SBP 130 mmHg. Sometimes BP lowers too much while decreasing stroke, CHD and HF risk leads to predominately increase in treatment discontinuation to adverse drug reactions. Initial two-drug combination therapy showed better adherence to treatment, reduced therapeutic inertia, better long-term BP control and reduces CV events. 5 drug classes (ACEIs/ARBs/BBs/CCBs/Ds) have proven ability to reduce BP, CV events in placebo controlled studies. These guidelines recommend that the same 5 classes of drugs should form the basis of antihypertensive therapy.
The core drug-treatment strategy for uncomplicated hypertension is dual combination initial therapy of ACEi or ARB plus CCB or diuretic in 1 pill. Step 2 of therapy will be triple combination of ACEi or ARB plus CCB plus diuretic in single pill. If hypertension is still resistant with treatment, spironolactone or other diuretic, alpha-blocker or beta-blocker is added to the triple combination therapy with 2 pills.
Past, Present, and Future: Addressing the Global Burden of Hypertension and Cardiovascular Disease
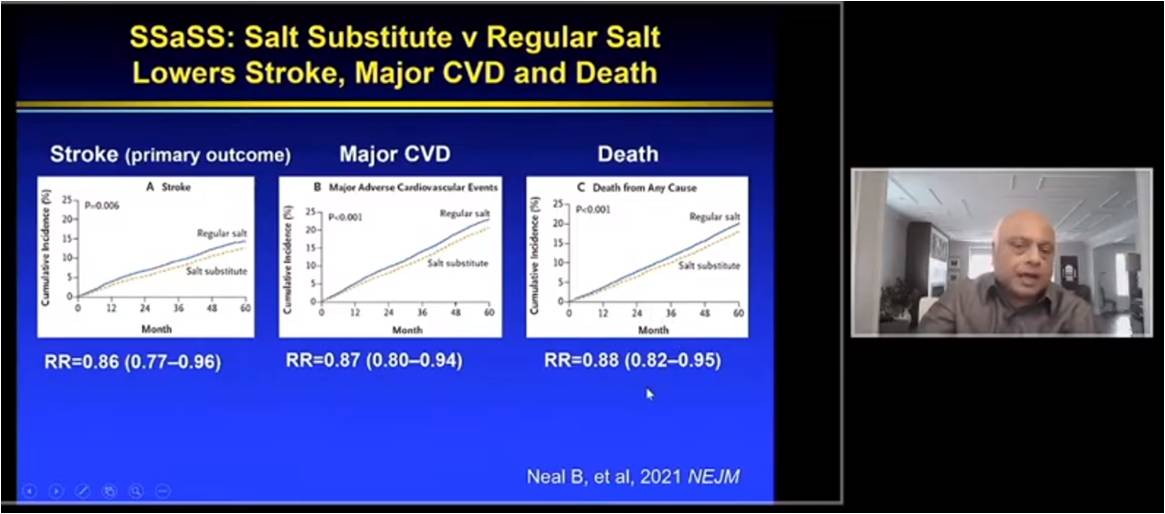
Yusuf S, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022. The prevalence of hypertension is about 40-50% in most of countries. 10 years back, PURE study showed that 17 countries showed very high prevalence of hypertension with 40-50% awareness and 40-45% treatment ratio whereas control rate was 10-20% only. Salt substitute and Stroke Study (SSaSS), a cluster, randomized, parallel, open-label trial with 20,995 patients randomized to salt-substitute or regular salt and followed for approx 5 years. Salt substitution group had higher SBP reduction with difference of 3.34 mmHg. Also, salt substitution showed mean 24 hr U Na excretion of 4.3g/d with diiference of 8% and mean 24 hr U K excretion of 1.4g/d with difference of 57%. Salt substitute lowers stroke, major CVD and death in patients as compared to regular salt. PREMIER trial showed that the established behavioral program further lowered SBP by 3.7 mmHg (p<0.01). Combined DASH diet with established behavioral program resulted in further SBP reduction by 0.6 mmHg. Bothe interventions significantly lowered body weight. FDC meta analysis of 18,162 patients overall from TIPS-3, HOPE-3 and PolyIran studies showed that FDC group significantly reduces LDL-C (mean diff- 22.6 mg/dL) and SBP (mean diff- 4.7 mmHg) as compared to control, group. The primary outcome i.e. CV death, MI, stroke, revascularization was significantly reduced by FDC group (p<0.0001). The addition of aspirin to FDC showed superior results in risk reduction of primary outcomes.
Hypertension is poorly detected, treated and controlled worldwide. Improving K intake reduces BP, CVD and mortality. Combination of BP lowering drugs plus statin plus aspirin safely reduces CVD by 50%. Such a low cost community wide strategy can avoid over 10 million CVD events each year globally and is applicable to all economic settings.
Gaps in Guideline-Based Lipid-Lowering Therapy for Secondary Prevention in the United States: A Nationwide Analysis of 227,824 Patients
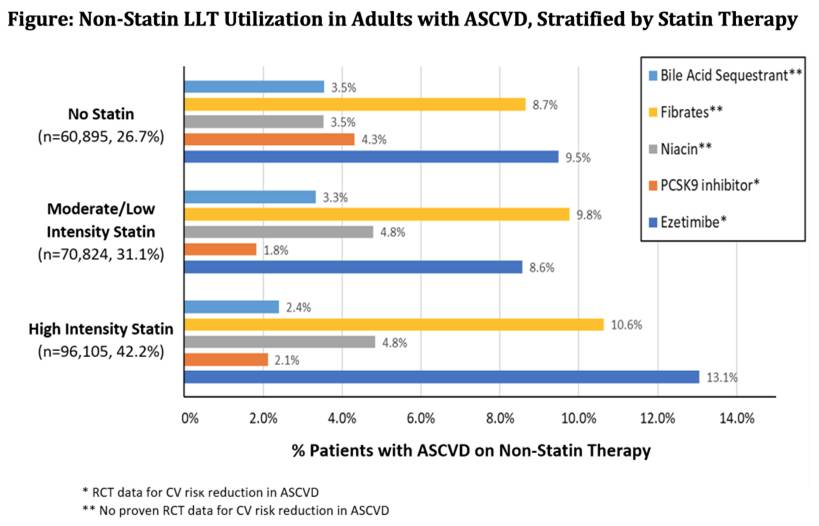
Kolkailah AA, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022.Statins are specified for the secondary prevention of atherosclerotic cardiovascular disease (ASCVD). But, the degree to which statins are used and dosed for secondary prevention in clinical practice is not clear.
Patients with ASCVD that acquired care during 2017-2018 were recognized over 90 health systems in the US using Cerner Real World Data, a de-recognized electronic health record (EHR) dataset. Medication data were analysed to categorize patients into 3 groups according to 2018 ACC/AHA guideline recommendations: not on a statin, on lower-than-recommended statin (low or moderate intensity), and appropriate dose (high intensity).
From 227,824 ASCVD patients incorporated (median age 65 years, 61.7% male, 80.1% white), 41.2% were on appropriate statin treatment, 31.1% were on lower-than-recommended treatment, and 26.7% were on no statin. Patients not on statins or on less-than-recommended statin intensity were more likely to be female and less likely to have private insurance as compared to patients on appropriate treatment (p<0.001). All groups had low usage of non-statin lipid lowering therapy (LLT).
Above half of patients with ASCVD are not on guideline-recommended appropriate statin treatment, few are using evidence-based non-statin LLT, and many are using non-evidence-based LLT. Additional work is urgently required to enhance usage of guideline-based LLT in clinical.
Long-Term Overexpression of BMP9 Prevents Pulmonary Hypertension

Genetic evidence implies bone morphogenetic protein 9 (BMP9) as a culprit gene for pulmonary arterial hypertension (PAH). But, removal or inhibition of BMP9 prevents or even alters PAH. To mark this contradictory, Wang SJ, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022 which developed a BMP9 transgenic rat model (Tg-BMP9) and evaluated the long-term impact of BMP9 on the pulmonary vascular.
Transgenic SD rat lines were developed with overexpression of human BMP9 especially in the liver. The phenotype characteristics of pulmonary artery were evaluated at baseline or exposed to of monocrotaline stimulation for 3 weeks.
The expression of BMP9 protein were frequently up-regulated in both liver and blood in Tg-BMP9 rats. These rats were phenotypically normal for up to 6 months of results. Surprisingly, the monocrotaline-induced pulmonary vascular remodeling were almost completely inhibited using BMP9 overexpressing. In Tg-BMP9 rats, the right ventricular wall thickness (RVAW) and internal diameter (RVID) were reduced by 33% and 45%, respectively. Tg-BMP9 rats showed reduction of mean pulmonary arterial pressure (mPAP) by 20 mmHg. Tg-BMP9 rats showed lesser wall thickness of small pulmonary arteries as compared to in wild-type littermates.
Long-term overexpression of BMP9 does not lead to spontaneous PAH. In comparison, it prevents pathological pulmonary remodeling. The long-term improvement of BMP9 could be a favorable preventive strategy for PAH.
A Comparison of Plant-Based, Mediterranean, Paleolithic and Dash Diets

Cardiovascular disease is the major cause of death in the US. Talreja S, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022 which analysed the effect of four diet programs: plant-based, Mediterranean, Paleolithic and DASH diets on CV risk factors.
Nondiabetic adults (ages 35-85) with one or more risk factors for CVD were enrolled in the study. Participants attended a comprehensive nutrition education program before a 60-day diet intervention in which they kept a daily food log and met weekly with a multi-disciplinary study team. An initial health screen analyzed weight, blood pressure, fasting glucose, A1C, lipids and lipoprotein particles, and was repeated following 60 days and at 6-months follow-up.
279 patients completed the 60-day dietary intervention (58 Vegan, 80 Mediterranean, 76 Paleo, 65 DASH), and 199 returned for 6-month follow-up. Mean age of patient was 56 years, mean BMI 33 kg/m2. Mean FPG, TG and HDL-C were within the normal range at baseline, but LDL-P and BP were increased. Patients lost an average of 9 lbs (4.7% body weight), which was correlated with enhancements in BP over all groups following 60 days on the respective diets. Patients lost the most weight (6.5%) on the Vegan and Paleo diets and exhibited the highest enhancements in lipid risk factors (11-14% reduction in LDL-P; 10-20% reduction in VLDL and TG).
All 4 diets aided weight loss and enhanced BP however showed changing impacts on lipid risk factors. Impacts were highest and sustained in those patients who underwent regular diet support group meetings.
Multisite, Randomized, Controlled Trial of a Supermarket and Web-based Intervention Targeting Nutrition for Cardiovascular Risk Reduction
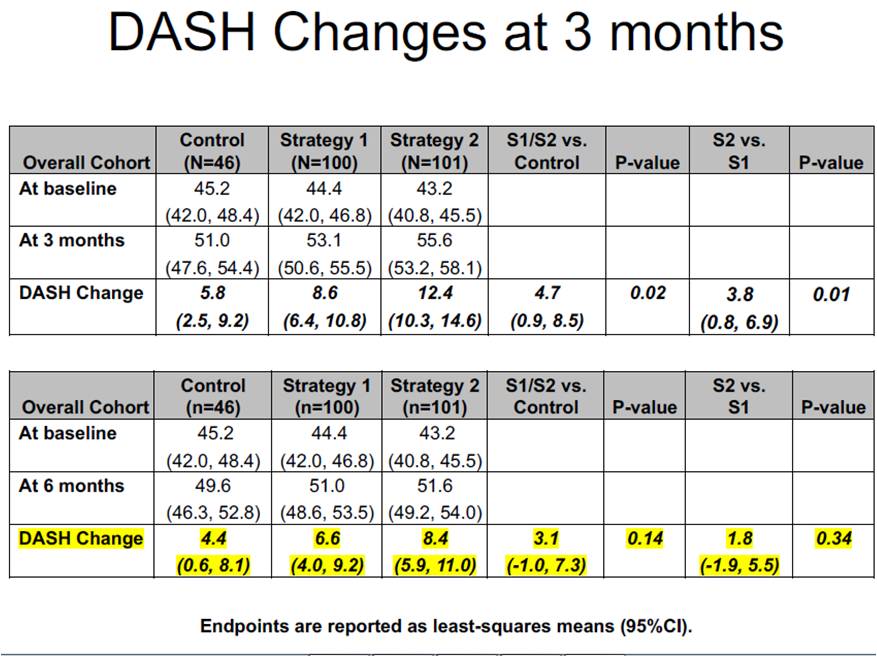
Steen DL, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022. Dietary interventions may foremost be delivered at grocery stores, which provide convenience, accessibility, full food inventories, and increasingly, in-store registered dietitians, online shopping and delivery services, electronic food purchasing data-guided support tools, and other healthcare services. The effectiveness of interventions controlling these opportunities has not been explored by well designed clinical trials. A multisite, randomized, controlled trial (N=247) was conducted enrolling from a primary care network via each participant’s home grocery store and retail clinic. Two individualized, in-person, dietitian-led, education interventions focused on the Dietary Approaches to Stop Hypertension (DASH) dietary pattern and guided by electronic food purchasing data were evaluated: 1) “Strategy 1” harnessed the in-store environment for education, demonstration and practice and 2) “Strategy 2” harnessed both the in-store and online environments. Participants were allocated 2:2:1 to Strategy 1, Strategy 2, or standard of care (SOC). Two hypotheses were analysed hierarchically to estimate change in DASH score from baseline to 3 months (post-intervention): 1) Strategies 1 and 2 together compared with SOC and 2) Strategy 2 compared with Strategy 1. The interventions elevated DASH score by 4.7 as compared to SOC (0.9, 8.5; p=0.02). Strategy 2 elevated DASH score by 3.8 (0.8, 6.9; p=0.01) as compared to Strategy 1. A pre-specified examination showed that prior to the COVID-19 pandemic, the interventions elevated DASH score by 8.3 (3.4, 13.3; p=0.001) as compared to SOC.
This trial exhibited the effectiveness of two comprehensive, retail based, dietary interventions as well as modern online shopping devices. These findings are timely given the rapid growth and consumer adoption of online shopping as well as retail-based care. This trial shows the chance for academia to cooperate with the rapidly expanding and evolving, retail-based healthcare industry to outline and rigorously analyse nationally scalable, community-based healthcare interventions.
Magnitude And Duration of Effects of A Short-interfering RNA Targeting Lipoprotein(a): A Placebo-controlled Double-blind Dose-ranging Trial (APOLLO Trial)
Nissen S, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022. A genetically determined, independent risk factor for atherosclerotic cardiovascular disease (ASCVD) and aortic stenosis (AS) is elevated Lipoprotein(a) [Lp(a)]. As per mendelian randomization studies, elevated Lp(a) levels show positive association with ASCVD and AS.
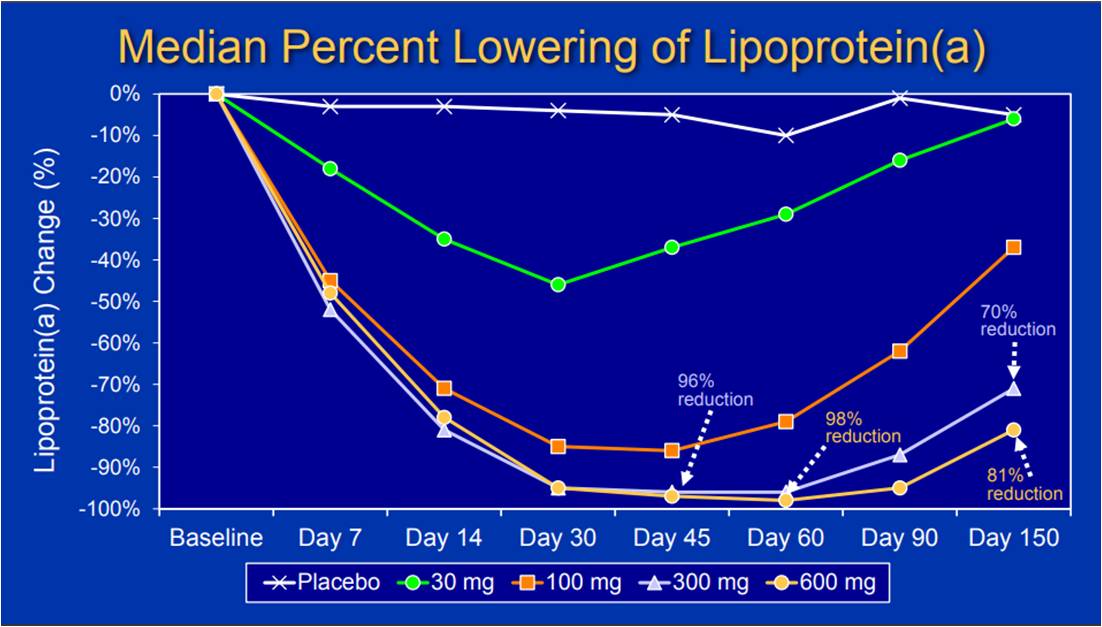
SLN360 is a 19-mer double-stranded small interfering RNA (siRNA) targeting LPA messenger RNA. Apolipoprotein(a) is encoded in LPA which is a dominant and rate limiting component in the hepatic synthesis of Lp(a). SLN360, an siRNA contains a covalently linked N-acetyl-galactosamine (GalNac) ligand attaches to a receptor expressed on liver cells facilitating concentration of SLN360 in the liver. The APOLLO trial was conducted that included men and women, between the 18-70 years of age, without evidence of ASCVD or AS and an Lp(a) level ≥150 nmol/L (equivalent to approximately 60 mg/dL). The mean age of the participants enrolled was 49.6±13.5 years, 53.1% were female, and median Lp(a) levels were 224 nmol/L (IQR 188-278). Two cohorts were developed with 8 participants in each ((6 active: 2 placebo), were randomized to ascending doses of SLN360 or placebo at 30, 100, 300, or 600 mg subcutaneously. Measurement of plasma concentrations of the drug and Lp(a) were used to determine the pharmacokinetic and pharmacodynamic effects of SLN360 and effects were assessed at multiple time points for the first 24 hours and during follow up for 150 days. Single dose of SLN360 significantly reduces median Lp(a) levels at day 30. SLN360 showed significant reduction in Lp(A) by 98% after 60 days. SLN360 300 mg and 600 mg dose showed significant reduction in LDL-C by 21% and 26% resp. and in ApoB by 21% and 24% resp.
Subcutaneous injection of an siRNA (SLN360) targeting mRNA for the LPA gene lowered lipoprotein(a) upto 98%. >70% and >80% reductions in Lp(a) persisted for 150 days after the 300 mg and 600 mg doses. The highest doses reduced LDL-C and Apo-B by 20-30%. The findings support further development of the therapy.
Patiromer for the Management of Hyperkalemia in Subjects Receiving Renin-angiotensin-aldosterone System Inhibitor Medications for Heart Failure with Reduced Ejection Fraction: Results from the DIAMOND Trial
Butler J, presented a study in a session at American College of Cardiology on 3rd April, 2022. For the treatment of patients with heart failure with reduced ejection fraction (HFrEF), Renin-angiotensin-aldosterone system inhibitors (RAASi) follow a class I indication. However, RAASi therapy is often down titrated or discontinued in patients with history of or current hyperkalemia. The following study hypothesized that treatment with patiromer, a novel potassium binder, can result in lower serum potassium (sK+) levels, thus facilitating guideline directed medical therapy.
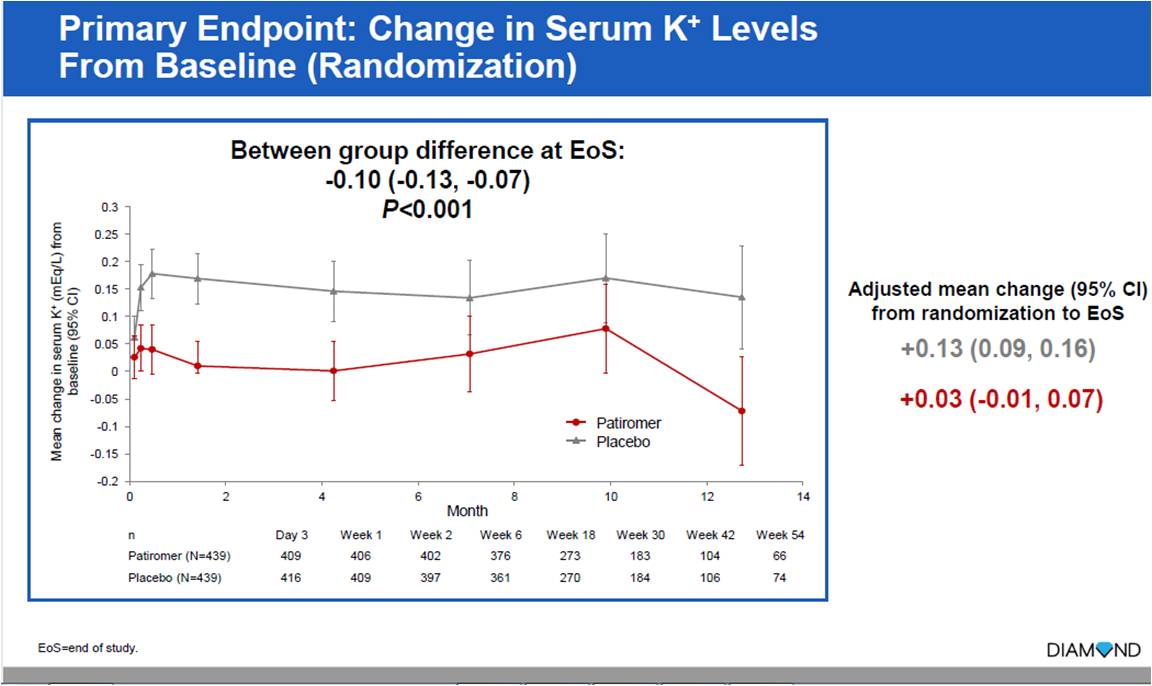
The DIAMOND trial was conducted which included 1640 patients with HFrEF with current or history of hyperkalemia where participants were optimized on RAASi therapy including mineralocorticoid receptor antagonist (MRA), and patiromer. Following this, patients were randomized to double-blind in a 1:1 ratio to either continued patiromer treatment or plabo (patiromer withdrawal). The primary endpoint assessed was mean difference in serum potassium from baseline between the two arms for the duration of the trial.
A total of 1194 patients entered the run-in phase, out of which 878 were randomized. Average duration of follow up was 266.6 days. Patiromer showed significantly lesser increase in serum K+ levels as compared to placebo (+0.03 vs +0.13) (p<0.001). Patiromer had lesser no. of hyperkalemia events than placebo (61 vs 85) (p=0.006). Lesser no. of patients with patiromer had reduction of MRA dose below target (61 vs 83) (p=0.006).
Most patients (84.6%) with HFrEF and RAAS related hyperkalemia could achieve optimal doses of RAASi including MRA when treated with patiromer. Patiromer maintained lower serum K+ levels. Patiromer was associated with lower incidence of hyperkalemia events and greater proportion of patients being maintained on MRA at target doses. Patiromer lead to 35% relative risk reduction in total number of hyperkalemia events.
A Cluster-Randomized PRagmatic Trial Aimed At ImprOving Use of Guideline Directed Medical Therapy in OutPatienTs with Heart Failure: PROMPT-HF
Ghazi L, presented a study in a session at American College of Cardiology (ACC) on 3rd April, 2022. The use of GDMT improves outcomes in patients with HFrEF but uptake remains challenging. The PROMPT-HF trial, pragmatic multicenter EHR-based randomized controlled trial was developed an hypothesis that targeted and tailored EHR alerts recommending GDMT in HFrEF patient can improve guidance adherence.
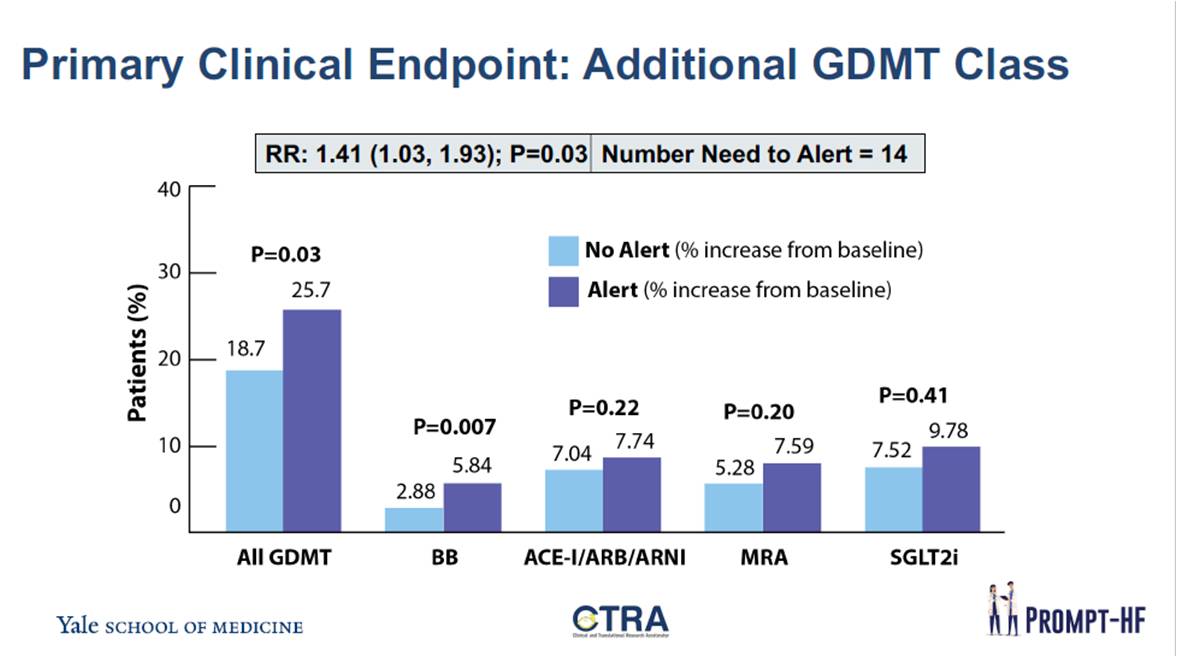
This trial included 100 clinicians seeing the most HFrEF patients were randomized to the alert vs usual care. The alert notified providers to GDMT recommendations as per their HFrEF patients who were not receiving any of 4 recommended medication classes. The primary outcome assessed was an increase in number of GDMT classes prescribed at 30 days post-randomization.
In the PROMPT-HF trial, a total of 1310 ambulatory HFrEF patients were enrolled over 7 months. At baseline, 84% were receiving BB, 71% ACE-I/ARB/ARNI, 28% MRA and 11% SGLT2i. In the alert arm, proportion of patients in whom GDMT components were added was higher; 117/625 in the usual care arm (18.7%) and 176/685 patients in the alert arm (25.7%) [RR: 1.38 (1.01, 1.87); p=0.04].
Significant higher rates of GDMT for a patient centred EHR-based alert for HFrEF outpatients as compared to usual care. The study indicates that this low cost-intervention can be rapidly integrated into clinical workflow, accelerate adherence to guidelines, and improve clinical outcomes, including mortality.

