Dyad Gender and Relationship Quality Are Related to Heart Failure Self-care Maintenance

Self-care, a health maintenance procedure, monitoring and symptom treatment, enhances morbidity and mortality in HF adults. Caregivers are significant in promoting patient self-care however little is known about the impact of relationship quality (RQ) on HF patient self-care, particularly in same and mixed gender dyads.
Stawnychy MA, presented a session at American Heart Association Scientific Sessions 2020: A Virtual Experience which ascertained the contribution of dyadic gender and RQ on HF patient self-care maintenance. Secondary analysis of baseline data was done from a study of Italian adults with HF and their caregivers (n=503). Dyads were enlisted to estimate efficacy of motivational interviewing on HF self-care maintenance computed with the Self-Care of Heart Failure Index v.6.2, confirmed in an Italian community. The Mutuality Scale was used to estimate RQ, validated for HF patients and caregivers. Dyadic gender was classified as Male-Male (M-M), Female-Male (Fpt-Mcg), Female-Female (F-F), and Male-Female (Mpt-Fcg; reference group). Determinants of HF patient self-care maintenance was recognized with univariate linear regression with backward ejection (p<.05). The sample was 48% Mpt-Fcg, 27% F-F, 15% Fpt-Mcg, 10% M-M. 86% Mpt-Fcg dyad patients were married; with older (59±15 years), less educated (46% secondary or lower) spousal caregivers (66%). More F-F vs M-M patients lived alone (32% vs 4%). Determinants of better patient self-care were: living alone, receiving aid for HF, better mental quality of life, patient and caregiver employment, caregiver married status, greater caregiver perceived social support, and more months caring for the patient. 23% of variance was shown in patient self-care maintenance with dyad gender, RQ, and these covariates. Dyad gender independently provided to self-care, however only for same gender dyads. Being in a M-M dyad was correlated with greater patient self-care (ß=.52, p<.026). Better caregiver perception of RQ in both M-M and F-F dyads was correlated with lower patient self-care (M-M: ß=-.97, p<.001; F-F: ß=-.55, p<.026). There were no substantial interactions for patient RQ or mixed gender dyads.
Dyadic relationship quality seems to be significant for self-care, especially in M-M dyads and should to be contemplated when working with HF patients and their caregivers.
Transient Cell Cycle Induction in Cardiomyocytes is a Promising Approach to Treat Ischemia Induced Heart Failure
The heart’s regenerative ability to repair itself following myocardial infarction (MI) is reduced. Previous research has shown that ectopic introduction of the complexes Cdk1/CyclinB1 and Cdk4/CyclinD1 (4F) promotes in vitro and in vivo proliferation of cardiomyocytes and enhances cardiac function following MI. But, its clinical application is limited because of the concerns for tumorigenic prospective in other organs.
Abouleisa R, presented a session at American Heart Association Scientific Sessions 2020: A Virtual Experience which recognised on a single cell transcriptomic basis the essential reprogramming steps that cardiomyocytes require to undertake to development via proliferation procedure after 4F overexpression, and then, in small and large animals, to evaluate the pre-clinical effectiveness of transient and cardiomyocyte specific expression of 4F in enhancing cardiac function following MI. Temporal bulk and single cell RNAseq of mature hiPS-CMs managed with 4F or LacZ control for 24, 48, or 72 h showed full cell cycle reprogramming in 15% of the cardiomyocyte population which was correlated with sarcomere disassembly and metabolic reprogramming. Non-integrating lentivirus (NIL) showed transient overexpression of 4F particularly in cardiomyocytes driven by TNNT2 (TNNT2-4F-NIL). TNNT2-4F-NIL or control virus was injected intramyocardially, one week after induction of ischemia-reperfusion injury in rats or pigs. Rats or pigs managed with TNNT2-4F-NIL exhibited a 20-30% substantial enhancement in ejection fraction and scar size four weeks after treatment as compared with controls, as estimated using echocardiography and histological evaluation. Estimation of cardiomyocyte proliferation in pigs by a novel cytokinesis reporter exhibited ~10% of the cardiomyocytes within the injection site were labelled as daughter cells after injection with TNNT2-4F-NIL as compared to ~0.5% background labelling in control groups.
The first understanding of the process of forced cardiomyocyte proliferation was provided and advanced clinical applicability of this approach via minimization of oncogenic prospective of the cell cycle factors by a novel transient and cardiomyocyte-specific viral construct was also provided.
Cardio-ankle Vascular Index Predicts New Onset Stroke in Patients with Heart Failure
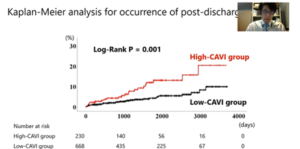
Hotsuki Y, presented a session at American Heart Association Scientific Sessions 2020: A Virtual Experience which assessed the implication of cardio-ankle vascular index (CAVI) to forecast new onset stroke in patients with heart failure (HF).
A total of 898 patients hospitalized for HF were recruited with clinical data in a prospective observational study. The precise cut-off value of CAVI in forecasting post-discharge stroke was 9.6 as per the survival classification and regression tree analysis. Patients were divided into two groups: the high CAVI group (CAVI > 9.6, n = 230, 25.6%) and the low CAVI group (CAVI ≤ 9.6, n = 668, 74.4%). The patients’ characteristics and event of new onset stroke were compared. The high CAVI group was older (73.5 vs. 66.0 years old, p < 0.001) and had a greater prevalence of male sex (74.3% vs. 62.0%, p = 0.001) and prior stroke (23.5% vs. 17.5%, p = 0.047). The high CAVI group exhibited greater levels of B-type natriuretic peptide (246.0 vs. 165.1 pg/mL, p < 0.001) and lower levels of assessed glomerular filtration rate (51.6 vs. 61.8 mL/kg/1.73 m2, p < 0.001). In contrast, left ventricular ejection fraction, and prevalence of other co-morbidities such as hypertension, diabetes mellitus, dyslipidemia, chronic obstructive pulmonary disease was comparable among the two groups. The Kaplan-Meier evaluation showed that rate of new onset stroke was greater in the high CAVI group as compared to the low CAVI group (Figure, log-rank p = 0.001). High CAVI was an independent forecaster of new onset stroke following adjusting for potential confounding factors (hazard ratio 2.359, 95% confidence interval 1.223-4.513, p = 0.010).
CAVI independently forecasts new onset stroke in HF patients.
Molecular Signatures of Sex Differences in Heart Failure with Preserved Ejection Fraction
Heart failure with preserved ejection fraction (HFpEF) is a complex syndrome entailing diastolic dysfunction and metabolic diseases. Women are twice as likely to develop HFpEF than men and present with a higher rate of symptoms. But, the sex-specific biology of HFpEF is not known. Cao Y, presented a session at American Heart Association Scientific Sessions 2020: A Virtual Experience which analysed sex-specific molecular signatures of diastolic dysfunction in HFpEF. In C57BL/6J male and female mice, a ‘two-hit’ HFpEF model were developed with HFD and l-NAME (Nω-nitrol-arginine methyl ester). RNA-seq for heart tissue from mice under HFpEF versus Chow condition was executed and results were incorporated with multi-omics datasets comprising hybrid mouse diversity panel (HMDP, a panel of more than 100 inbred strains of mice) and human heart failure group to analyse novel gene-by-sex interactions in the heart. HFD and l-NAME activated diastolic heart failure phenotypes in both male and female mice. Greater E/A (1.68 ± 0.09 vs. 1.40 ± 0.04, p < 0.05 under chow diet), E/E’ (35.82 ± 2.05 vs. 26.13±1.11, p < 0.05 under chow diet; 53.78 ± 3.94 vs. 43.92±2.08, p < 0.05 after HFpEF) and lung weight (wet/dry ratio, 4.51 ± 0.09 vs. 4.15 ± 0.09, p < 0.05 after HFpEF) was observed in females compared with males. Pathway evaluation showed that female mice showed a higher reduction in fatty acid metabolism, insulin signaling, heart development and an improved increase in cell cycle, inflammation, cholesterol efflux and serine synthesis upon HFpEF as compared to male mice. HFpEF mice showed that female hearts with reduced mtDNA copy number relative to males, together with high fat/high sucrose diet-induced metabolic disorder HMDP group and isoproterenol-induced heart failure HMDP group (3102.56 ± 85.70 vs. 3770.43 ± 77.44, p = 4.51E-08). Cardiac mtDNA was inversely associated with diastolic dysfunction (bicor = -0.307, p = 0.005) and was managed with gonadal hormones.
Systems genetics approach was used that incorporates multi-omics datasets and analyse novel gene-by-sex interactions in the heart. Females showed more acute metabolic diseases and mitochondrial dysfunction which are responsible for higher diastolic dysfunction of HFpEF, as compared to males.
10-Year Risk Prediction Equations for Heart Failure in Chronic Kidney Disease: The Chronic Renal Insufficiency Cohort Study
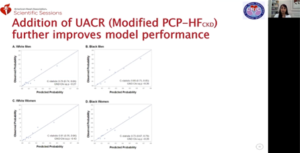
Heart failure (HF) is a main contributor of cardiovascular morbidity and mortality in the chronic kidney disease (CKD) population. While risk equations such as the pooled cohort equations to inhibit HF (PCP-HF) have been validated in the general population, in CKD-specific groups, no such tools have been analysed. Strategies are required for recognition of individuals with CKD at greater risk of HF. Mehta R, presented a session at American Heart Association Scientific Sessions 2020: A Virtual Experience which explored risk equations for 10 years for heart failure in chronic kidney disease. Individuals among the ages of 30-79 without baseline cardiovascular disease were included in the CRIC Study between black and white patients with CKD stages 2-4. Model performance of the PCP-HF was analysed to forecast incident HF and recalibrated the PCP-HF in the CKD population (PCP-HFCKD). Given that indices of kidney function are correlated with HF, the contribution of assessed glomerular filtration rate (eGFR) and urinary albumin-to-creatinine ratio (UACR) to PCP-HFCKD was analysed with change in C-statistic, net reclassification index (NRI) and integrated discrimination index (IDI). Between 2328 participants, mean (SD) baseline eGFR was 46 (15) ml/min/1.73m2 and median (IQR) UACR was 37 (7, 381) mg/g. 336 incident HF events arised across 9.5 years of follow-up. The PCP-HF equations systematically under-forecasted HF risk in participants with CKD (C-statistic <0.71 for all sex-race groups). The recalibrated PCP-HFCKD showed good discrimination and calibration (C-statistic 0.75-0.78), except in black women (0.61). Inclusion of UACR, however not eGFR, to the PCP-HFCKD enhanced model calibration (Figure) and execution in all race-sex groups (delta C-statistic 0.03-0.11, NRI and IDI values p<0.001).
Routinely accessible clinical data can accurately forecast incident HF in patients with CKD. Further study is required to analyse whether execution of the altered PCP-HFCKD risk prediction equation into clinical practice can enhance HF prevention and patient effects.
Cardiac Remodeling in Adults Following Percutaneous Patent Ductus Arteriosus Closure: A Meta-analysis
Blissett S, presented findings from the Session “Adult Congenital Heart Disease (ACHD) Risks and Outcomes” at American Heart Association Scientific Sessions 2020: A Virtual Experience. This meta-analysis was conducted to characterize the extent of cardiac remodeling following percutaneous Patent Ductus Arteriosus (PDA) closure in adults. In adults undergoing percutaneous PDA closure, MEDLINE and EMBASE were systematically searched for original studies that recorded echocardiographic variables at baseline, immediately post-procedure (within 24 hours) and follow-up (>1 month). In addition, echocardiographic data from a cohort of patients > 18 years of age who were subjected to percutaneous PDA closure at the center between 01/2015 and 12/2019 was included. Weighted averages have been determined for parameters with appropriate data for pooling, and pooled differences have been presented as weighted mean differences. Heterogeneity has been tested using the I2 Statistics. 5 studies were found after the screening of 278 abstracts. The meta-analysis encompassed 244 patients when paired with the cohort of 13 patients. The weighted mean age of all patients was 33 years, with all studies consisting primarily of female patients, and the median follow-up was 12 months (studies ranged from 1 month to 5 years). Left ventricular ejection fraction (LVEF) decreased significantly immediately after the procedure relative to the baseline, and all parameters decreased significantly at follow-up (Table 1).
Reverse remodelling was found in adults who experienced percutaneous PDA closure, as seen by the decreases in left ventricular and left atrial sizes. Withdrawal of chronic volume overload or increased afterload could represent the significantly lower LVEF immediately after the procedure. The clinical significance of a statistically significant lower LVEF for follow-up testing is uncertain and further evaluation is needed.
Characteristics and Outcomes of Patients with Heart Failure with Reduced Ejection Fraction and a Worsening Heart Failure Event
Carnicelli AP, presented findings from the Session “Acute and Advanced Heart Failure” at American Heart Association Scientific Sessions 2020: A Virtual Experience. The aim of the study was to identify the characteristics and outcomes of patients in a broad tertiary medical center with Heart Failure with Reduced Ejection Fraction (HFrEF) and a Worsening Heart Failure (WHF) case. It was reported that patients 18-85 years of age with chronic symptomatic HFrEF (EF ≤ 35 percent and ≥ 2 HF experiences in the previous 18 months) treated via the Duke Echo Lab Database at Duke University between Jan 2009-Dec 2018. A WHF event was described as either a hospitalization or Heart Failure (HF) emergency department (ED) visit in the previous 12 months. Patients with WHF event were treated with a collection of exclusion criteria [e.g. renal failure, left ventricular assist device (LVAD), heart transplant] in order to produce a patient cohort comparable to those participating in contemporary HF studies. As these differ over time, the cohort based on blood pressure (BP) or brain natriuretic peptide (BNP) levels was not limited. Baseline characteristics and outcomes were measured, including death and hospitalization. In the year prior to the index echo, 3668 (76%) of 4846 separate HFrEF patients had a WHF case. Patients with GFR <20 mL/min/1.73 m2 sequentially, (n=458), LVAD (n=291), or heart transplant (n=95) were excluded; in the WHF sample population, 2824/4846 (58%) remained. HFrEF patients with WHF were usually male (68%) with a median age of 65 years (IQR 54, 73) and a low EF (57% EF <25%). Coronary artery disease (71%), diabetes (44%) and high N-terminal pro b-type natriuretic peptide (NT-proBNP) (median 2405 pg/mL [698, 6841]) were normal. Beta-blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACEi/ARB), and Magnetic Resonance Angiography (MRA) use were 88%, 79%, and 44%, respectively. HFrEF patients with WHF had a high cumulative rate of all-cause mortality and HF hospitalization after indexing of 30 days, 1 year and 5 years (FIGURE).
Almost 76% had a WHF case in the past year in patients with chronic HFrEF at Duke University, and 58% met several of the main eligibility requirements of contemporary HF studies. There was a heavy burden of co-morbidities and very high incident rates in patients with recent WHF.
Heart Failure with Preserved Ejection Fraction Patients Do Not Augment Longitudinal Pumping During Exercise
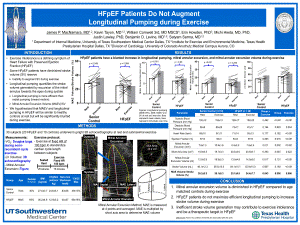
Macnamara JP, presented findings from the Session “Across the Spectrum of Stage A to Stage D Heart failure” at American Heart Association Scientific Sessions 2020: A Virtual Experience. This study aimed to estimate the contribution of longitudinal pumping to HFpEF when exercise induced stroke volume (SV) reserve is optimum relative to safe age-matched controls at rest and submaximal exercise. Simultaneous 3D echocardiography cardiopulmonary exercise research was conducted in 30 subjects (Heart Failure with Preserved Ejection Fraction [HFpEF] n = 20, age 69±5 years, Senior Control [CON]: n = 10, age 70±4 years) at rest and during exercise at a targeted heart rate of 100 bpm (HFpEF 66±18% VO2Max, CON: of 49±13% VO2Max, p=0.014). Using multi-beat 3D acquisition at rest and during sub-maximal exercise, left ventricular (LV) volumes and mitral annular excursion (MAE), a new metric of systolic activity, were measured. MAE volume (MAEV) was determined by multiplying MAE at the base of the ventricle by the short axis field. The quotient of MAEV and SV (percent) was measured as relative longitudinal pumping. At rest, mitral annular excursion (MAE) was lower in HFpEF. Compared to controls (CON Δ 3.3mm vs HFpEF Δ 1.1mm, group p = 0.002, group x exercise p = 0.011) and increased substantially less during sub-maximal exercise (figure). Compared to controls at rest, MAEV was equivalent in HFpEF but did not increase in HFpEF compared to controls (CON Δ 7.1 ml vs HFpEF Δ 1.9 ml, group x exercise p = 0.002). With exercise in CON, relative longitudinal pumping increased dramatically but remained unchanged in HFpEF (CON Δ 7.9% vs. HFpEF Δ-0.7%, group x exercise p = 0.043).
Despite exercising at a higher relative metabolic demand than their stable peers, longitudinal pumping does not rise in HFpEF patients. This lack of longitudinal pumping reserves may lead to the detection of cardiac limitations typically seen in HFpEF patients during exercise.
Identifying the Most Important ECG Predictors of Reduced Ejection Fraction in Patients with Suspected Acute Coronary Syndrome
Ahmad A, presented findings from the Session “A Potpourri of Physiologic and Psychosocial Factors Predicting Cardiovascular disease (CVD) Cardiovascular disease (CVD) Outcomes” at American Heart Association Scientific Sessions 2020: A Virtual Experience. The goal was to classify electrocardiogram (ECG) characteristics that are most predictive in the acute care environment for real-time screening of reduced left ventricular ejection fraction (LVEF). A secondary review of a longitudinal, observational cohort sample of patients tested for potential acute coronary syndrome was conducted. The parent research recruited consecutive patients assessed at three tertiary care hospitals associated with University of Pittsburgh Medical Center (UPMC) in the emergency department. Consecutive patients were included in whom an echocardiogram was performed during indexed encounter. Baseline ECGs have been pre-processed using algorithms unique to the manufacturer. In multivariate linear regression for predicting LVEF, 554 automated, 12-lead ECG characteristics were evaluated. Also regression trees were used to classify the most important predictive ECG. 297 patients (aged 63 ± 15.45 percent females) were included in the final survey. 57 percent ± 13 (IQR 50 percent -65 percent) was the mean LVEF. Depolarization dispersion in the horizontal plane; global repolarization dispersion; and irregular temporal indices in inferolateral leads were all-independent predictors of LVEF in multivariate analysis (R2 = 0.452, p < 0.001, F = 6.679). The most important determinants of decreased LVEF were horizontal QRS axis variance and prolonged ventricular activation (VAT) period at the left ventricular apex (Figure), while global QRS length was of less significance.
Poor R wave progression in precordial leads with dominant QS pattern in V3 is the most predictive characteristic of lowered LVEF in suspected Acute Coronary Syndrome (ACS). To help clinicians distinguish those with impaired cardiac function, this feature constitutes a clear visual marker.
Pro-inflammatory Diet Independently Predicts Shorter Event-free Survival in Patients with Heart Failure
Kang J, presented findings from the Session “A Potpourri of Physiologic and Psychosocial Factors Predicting CVD Outcomes” at American Heart Association Scientific Sessions 2020: A Virtual Experience. In patients with HF, the inflammatory capacity of individual diets, calculated by the dietary inflammatory index (DII), is correlated with event-free survival. Dietary Inflammatory Index (DII) scores were determined for 213 patients with HF (age 61 ± 12 years, 35 % female,
43 % New York Heart Association [NYHA III/IV]) from 4-day food diaries reported at baseline. In order to assess the time for all cause-hospitalization or death, patients were accompanied by monthly phone calls, medical record examination, and death reports for a median of 365 days. For the Cox regression model, the DII scores were dichotomized using the median value. The hierarchical multivariate Cox proportional hazards model was used to assess whether DII scores predicted event-free survival after age, gender, body mass index, prescribed angiotensin-converting-enzyme inhibitor, beta-blocker, cholesterol-lowering agent, anti-inflammatory agent, N-terminal pro B-type natriuretic peptide, comorbidity, depressive symptoms, and functional class of NYHA. Within the model constant, the DII scores independently predicted event-free survival (p = of 0.012). Compared to lower DII scores higher DII scores were correlated with more than double the likelihood of an incident (HR: 2.28, 95 percent Confidence Interval = 1.21-4.36).
Higher food consumption to encourage inflammation was associated with shorter event-free survival in HF patients. These findings provide further proof of diet contribution to the effects of HF.
Pulmonary Artery Pressure Guided Heart Failure Management Reduces Hospitalizations across All Stages of Chronic Kidney Disease
Raval NY, presented findings from the Session “Across the Spectrum of Stage A to Stage D Heart failure” at American Heart Association Scientific Sessions 2020: A Virtual Experience. This study was carried out to determine whether the value of Pulmonary Artery Pressure (PAP)-guided Heart Failure (HF) therapy continues to increase the severity of CKD. This retrospective cohort research was performed in the CardioMEMS Post Approval Study of NYHA Class III HF recipients of the PAP sensor. Patients were divided into quartiles estimated by the MDRD equation of glomerular filtration rate (eGFR). Heart Failure Hospitalizations (HFH) rates 1 year before versus 1 year after implantation of the PAP sensor were compared through quartiles of eGFR using the Andersen-Gill Cox proportional hazards model, while competing death risk, advanced HF therapy and progression to end-stage kidney disease were compared. To classify independent predictors of CKD (baseline eGFR < 90 mL/min/1.73 m2), multivariate analysis was performed. 1119 of 1200 PAP sensor recipients had concomitant CKD with stage 3 and 4 CKD occurring in 754 (67.4 percent) patients. In CKD patients, 40.6 %, 42.1 %, and 17.3 % respectively, showed worse, unchanged, or better CKD stage. Compared to 12 pre-implant months, HFH rates fell across all eGFR quartiles in 12 months after implantation (Table). PA systolic, diastolic, and mean pressures decreased in all GFR quartiles from baseline to 24 months. As a continuous variable, the baseline PAP predicted CKD progression independently (OR: 1.027, p= 0.0006).
In a broad HF population receiving the CardioMEMS sensor after Food and Drug Administration approval, reduction of HFH by PAP-guided therapy occurred through CKD phases. Thus, also in patients with advanced CKD, PAP control allows stable HF therapy optimization. Since CKD worsening is independently predicted by the higher baseline mean PAP, HF patients with this unfavorable hemodynamic value Frequires intensified monitoring.

