Hendren NS. Circulation. 2021 Jan 12;143(2):135-144.
Obesity impacts >4 in 10 adults and augments to diabetes, heart failure, and cardiovascular disease (CVD) morbidity and mortality. As the coronavirus disease 2019 (COVID-19) pandemic has developed, obesity may be a significant driver of hospitalization and may be death in patients with COVID-19. Simultaneously, younger age has been correlated with a much decreased risk of severe COVID-19 infection. But, it is not known whether the distinctly protective impact of younger age may continue to obese individuals. Even though preliminary observations recommend that young, obese individuals hospitalized with COVID-19 may be at greater risk for adverse effects, the possibility of an interplay among obesity and age has not been fully explained. Thus, Hendren NS, et al., conducted a study to analysis the association among BMI and in-hospital death, mechanical ventilation, adverse cardiovascular, renal, and venous thromboembolic effects in patients admitted with COVID-19 in the American Heart Association’s (AHA) COVID-19 CVD registry.
The patient data was acquired from 88 US hospitals in the first data release of the AHA COVID-19 CVD registry with data accumulation via July 22, 2020. People are briefed to abstract data from all consecutive patients hospitalized with active COVID-19 infection in participating hospitals, nevertheless of CVD condition, and data are listed into an electronic case record form. The medical record for the duration of the hospital stay was used to gather detailed demographic and clinical data, however no outpatient follow-up is executed. Adults (≥18 years old) with available BMI data and completed field entries for age, sex, admission date, discharge date, discharge disposition, and a medical history (selected as either none or as applicable conditions) were incorporated in the study group for present investigations. World Health Organization obesity class stratified the BMI, with normal weight predetermined as the reference group.
Obesity, and, in specific, class III obesity, was overexhibited in the registry as compared to the US population, with the largest variations between adults ≤50 years. (Figure 1) From 7606 patients, 2109 (27.7%) patients showed in-hospital death or mechanical ventilation, 1302 (17.1%) patients showed in-hospital death, and 1602 (21.1%) patients showed mechanical ventilation. Classes I to III obesity were correlated with greater risks of in-hospital death or mechanical ventilation (odds ratio, 1.28 [95% CI, 1.09–1.51], 1.57 [1.29–1.91], 1.80 [1.47–2.20], respectively), and class III obesity was correlated with a greater risk of in-hospital death (hazard ratio, 1.26 [95% CI, 1.00–1.58]) following multivariable adjustment. Overweight and class I to III obese individuals showed greater risk for mechanical ventilation (odds ratio, 1.28 [95% CI, 1.09–1.51], 1.54 [1.29–1.84], 1.88 [1.52–2.32], and 2.08 [1.68–2.58], respectively). (Figure 2A) In the unadjusted models, overweight and obese individuals showed decreased risk for MACE (p<0.01 for all); but, in the adjusted models there was no correlation among obesity classes and MACE (P>0.05 for all). (Figure 2B) All primary end points (p-interaction<0.05 for each) exhibited substantial BMI using age interactions, such that the correlation of BMI with death or mechanical ventilation was strongest in adults ≤50 years, intermediate in adults 51 to 70 years, and weakest in adults >70 years. Severe obesity (BMI ≥40 kg/m2) was correlated with an elevated risk of in-hospital death only in those ≤50 years (hazard ratio, 1.36 [1.01–1.84]). In adjusted analyses, greater BMI was correlated with dialysis initiation and with venous thromboembolism however not with major adverse cardiac events. (Figure 3)
Thus, it was concluded that obese patients are more prone to hospitalized with COVID-19, and are at greater risk of in-hospital death or mechanical ventilation, especially, if young (age ≤50 years). Obese patients are also at greater risk for venous thromboembolism and dialysis. In all obese individuals nevertheless of age, these remarks support clear public health messaging and precise adherence to COVID-19 prevention strategies.
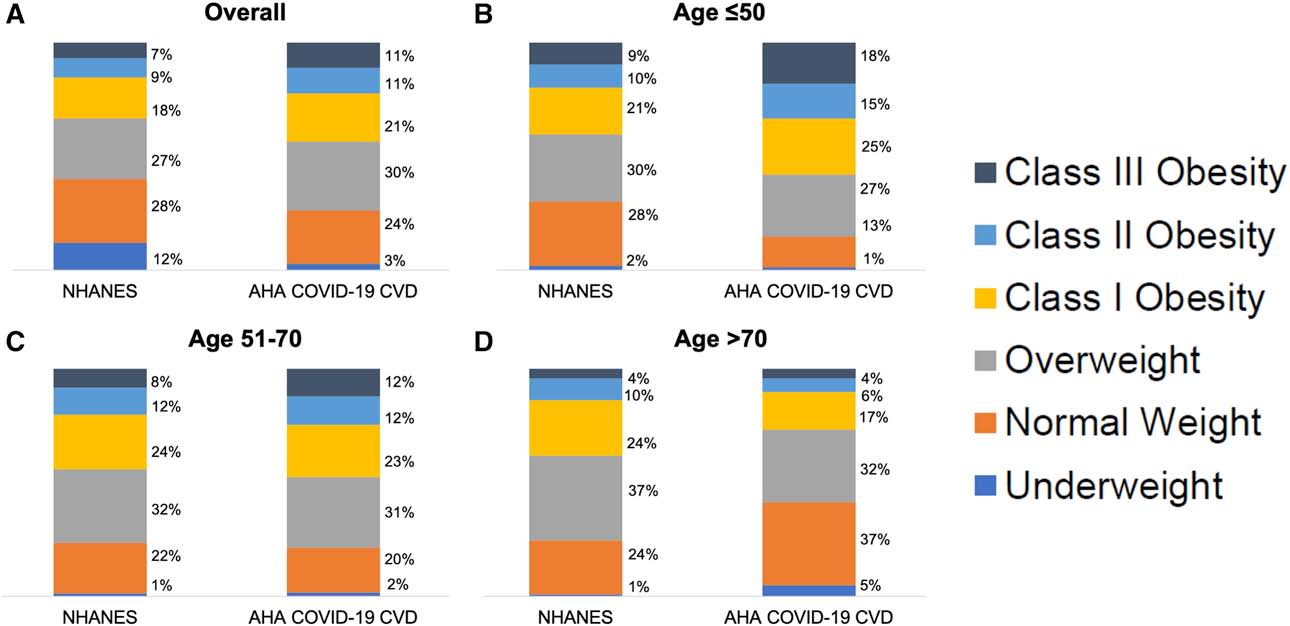
Figure 1: Proportion of individuals hospitalized by COVID-19 by BMI in comparison with NHANES
A, NHANES sample weighted proportion of US adults 2015 to 2016 and 2017 to 2018 (≥18 years old) by BMI in comparison with US adults in the AHA COVID-19 CVD Registry. B, Proportion of US adults 18 to 50 years old by BMI from NHANES and the AHA COVID-19 CVD Registry. C, Proportion of US adults 51 to 70 years old by BMI from NHANES and the AHA COVID-19 CVD Registry. D, Proportion of US adults >70 years old by BMI from NHANES and the AHA COVID-19 CVD Registry. World Health Organization BMI classes: underweight <18.5 kg/m2; normal weight 18.5 to 24.9 kg/m2; overweight 25.0 to 29.9 kg/m2; class I obesity 30.0 to 34.9 kg/m2; class II obesity 35.0 to 39.9 kg/m2; and class III obesity ≥40.0 kg/m2. AHA COVID-19 CVD indicates American Heart Association COVID-19 Cardiovascular Disease Registry; BMI, body mass index; COVID-19, coronavirus disease 2019; and NHANES, National Health and Nutrition Examination Survey
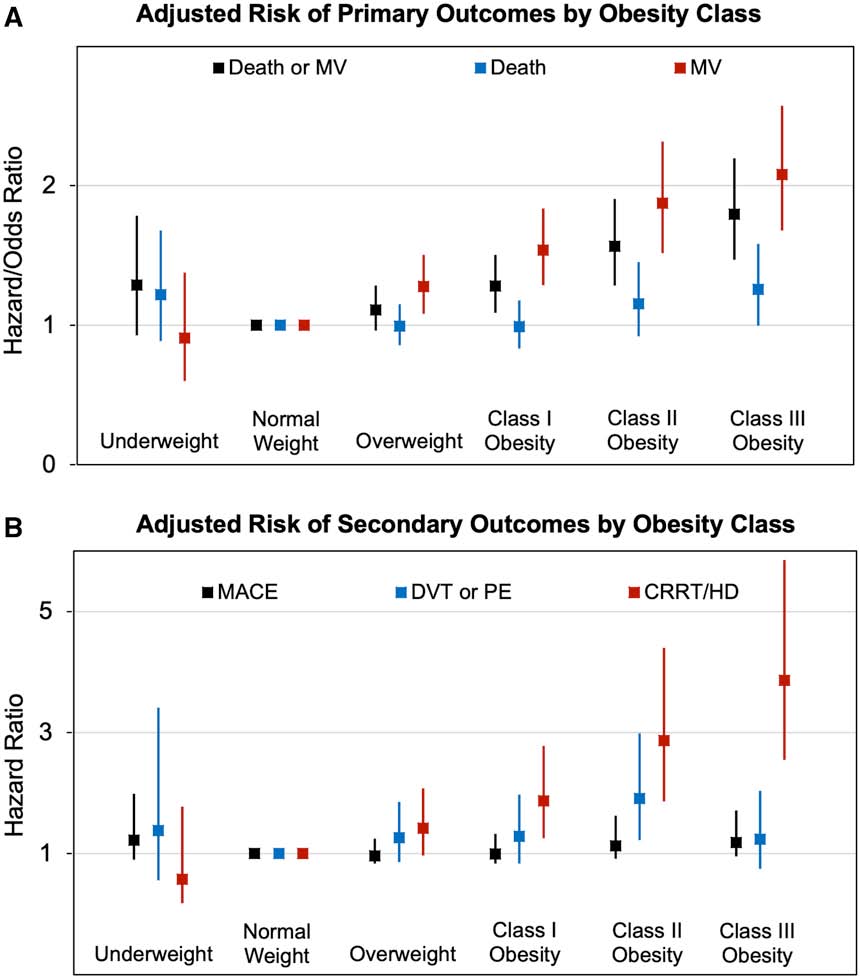
Figure 2: Primary and secondary outcomes by BMI class. A, Adjusted risk of primary and secondary outcomes by BMI classes with 95% CIs. B, Adjusted odds ratio for mechanical ventilation, and death or mechanical ventilation with remainder of outcomes represented as adjusted hazard ratios.
Outcomes were adjusted for age, sex, race, hypertension, diabetes, prior stroke, prior myocardial infarction, prior heart failure, chronic kidney disease, and current hemodialysis. Secondary outcomes considered the competing risk of death. BMI indicates body mass index; CRRT, continuous renal replacement therapy; DVT, deep vein thrombosis; HD, hemodialysis; MACE, composite of in-hospital myocardial infarction, stroke, all-cause death, and heart failure; MV, mechanical ventilation; and PE, pulmonary embolism.
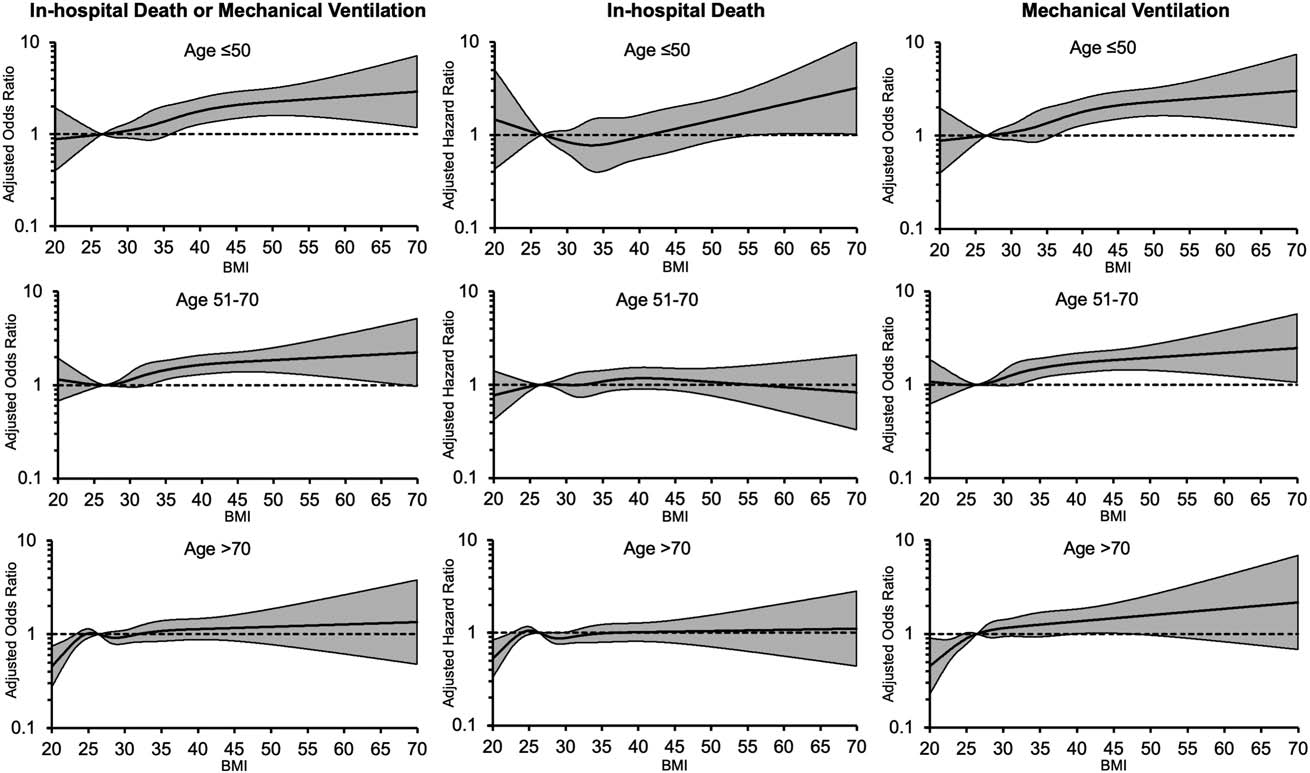
Figure 3. Risk of in-hospital death or mechanical ventilation by age and BMI.
Adjusted odds ratio for in-hospital death or mechanical ventilation (Left), adjusted hazard ratio for in-hospital death (Center), and adjusted odds ratio for mechanical ventilation (Right) by continuous BMI and ages ≤50, 51 to 70, and >70 years. BMI of 25.0 kg/m2 serves as the reference. Adjustment variables include age, sex, and race/ethnicity, history of cardiovascular disease (myocardial infarction, stroke, heart failure, or percutaneous coronary intervention), hypertension, diabetes, and chronic kidney disease. BMI indicates body mass index.

