Stocker TJ. JACC Cardiovasc Interv. 2021 Jan 11;14(1):29-38.
Tricuspid regurgitation (TR) has been correlated with elevated mortality in patients undergoing TTVR in the condition of pulmonary hypertension (PH). The mismatch among invasively and echocardiographically estimated PH – high invasive pressures however low echocardiographic pressure gradients has been correlated with unfavourable diagnosis because of developing tricuspid valve dysfunction. Hemodynamic markers incorporating non-invasive estimation of cardiac output have been recommended to provide as clinical endpoints following TTVR. But, There is limited data available about hemodynamic predictors analysed from right heart catheterization concerning adverse events following TTVR. Stocker TJ et al., conducted a study to describe precisely a comprehensive hemodynamic profile analysed by right heart catheterization (RHC) in patients undergoing TTVR, incorporating the analysis of hemodynamic changes following TTVR. Additionally, hemodynamic factors that forecast 1-year mortality following TTVR were recognised.
A total of 236 patients were enlisted in this international, multicentre study. Patients with severe symptomatic TR, in spite of being on optimal medical treatment, were analysed to undergo TTVR on a compassionate-use basis after being judged to be at high or prohibitive surgical risk with the local heart team. Data from clinical evaluation, echocardiography, intraprocedural RHC, and non-invasive cardiac output estimations were evaluated. A linear Cox regression analysis was used to recognise hemodynamic predictors for mortality and were it was used for stratification of patients with consecutive assessment of survival time. The median age of patients was 78 years (IQR: 74 to 82 years), and 53% of patients were women. The European System for Cardiac Operative Risk Evaluation II score predicted a median operative mortality of 5.1% (IQR: 3.3% to 9.9%). The risk score for analysis of mortality was estimated as 9% in patients undergoing isolated tricuspid surgery. At baseline, all patients showed extreme or higher TR with symptomatic heart failure (NYHA functional class III or IV in 89%, median N-terminal pro–B-type natriuretic peptide 2,952 ng/l). Left ventricular systolic function was maintained, and mitral regurgitation was mainly mild to moderate.
TTVR substantially decreased TR at discharge (grade $3þ in 16%; p < 0.001), with a corresponding 19% decrease of the right atrial v wave (21 mm Hg vs. 16 mm Hg; p < 0.001) and an enhancement in cardiac output (from 3.5 to 4.0 l/min; p < 0.01). (Figure 1) Invasive mean pulmonary artery pressure, transpulmonary gradient, pulmonary vascular resistance, and right ventricular stroke work were substantial predictors of 1-year mortality (p < 0.05 for all). Hemodynamic stratification predicted 1-year survival using mean pulmonary artery pressure and transpulmonary gradient best (p < 0.001). While patients with pre-capillary dominant PH exhibited an adverse prediction (1-year survival 38%), patients without or with post-capillary PH had beneficial result (1-year survival 92% or 78%, respectively). (Figure 2)
Thus, it was concluded that TTVR effectively modulates hemodynamic status in patients with right-sided heart failure, facilitating functional enhancement and symptomatic alleviation. Preprocedural analysis of the cardiopulmonary hemodynamic profile permitted the risk stratification of patients organised for TTVR and should be executed in the routine patient selection procedure. This study showed that patients without substantial PH and dominant post-capillary PH showed a good prediction following TTVR. The results of this study additionally showed the requirement for complementary medical or alternative therapy strategies in patients with severe TR and substantial pre-capillary PH.
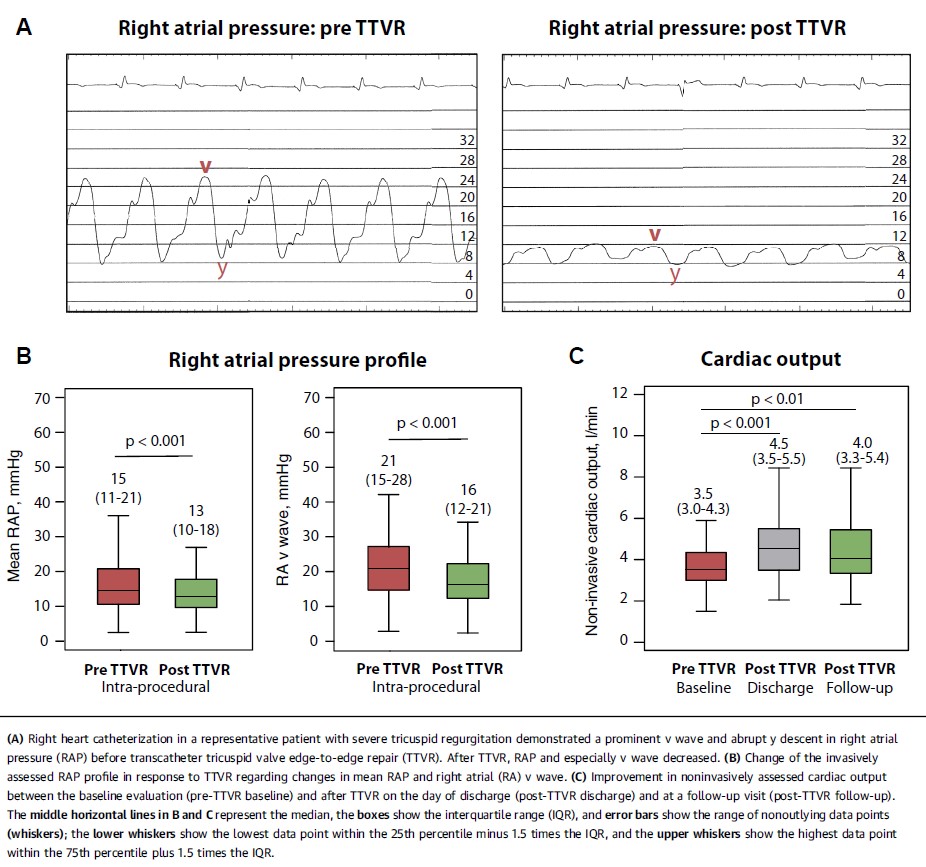
Figure 1: Hemodynamic changes after TTVR
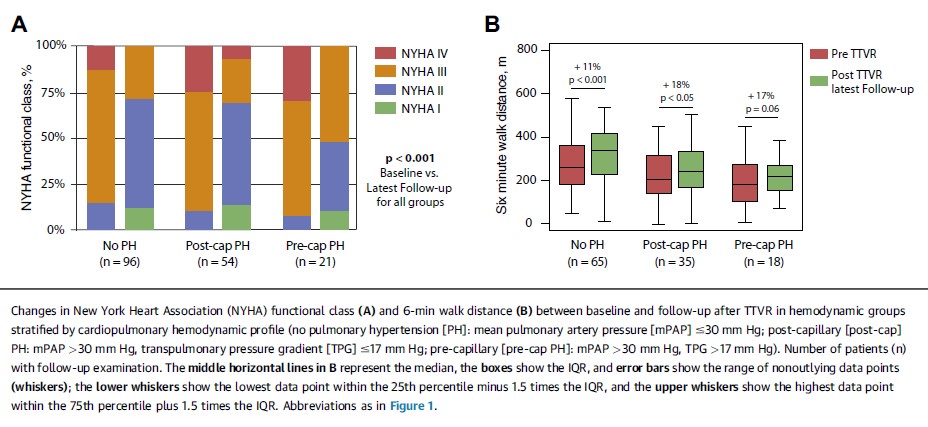
Figure 2: Clinical improvement after TTVR

