Kim YH. BMC Cardiovasc Disord. 2021 Aug 9;21(1):386.
Moderate-dose statin therapy is more frequently administered because of decreased bodyweights in actual practice of Asian population. Prediabetes is not an unfrequent population to interventional cardiologists. Recent studies outlined that people with prediabetes showed worse outcomes than normoglycemia and comparable to diabetes mellitus (DM) patients. To reflect contemporary practice in Asian patients and to analyse the different impacts of statin-intensity among prediabetes and type 2 DM (T2DM), in patients with AMI, Kim YH, et al. conducted a study which analysed a two-year clinical outcome in these two groups, specifically in Korean acute myocardial infarction (AMI) patients who underwent successful percutaneous coronary intervention (PCI) by newer-generation DES.
A total of 23,391 AMI patients aged ≥ 30 years at diabetes onset, who underwent successful DES implantation from November 2005 to June 2015, were analysed from the Korea AMI Registry (KAMIR). A total of 11,612 AMI patients were categorised as statin users (n = 9893) and non-users (n = 1719). Afterwards, statin users were further divided into high-intensity (n = 2984) or low-moderate-intensity statin (n = 6909) therapy groups. Finally, patients in these two groups (A and B, respectively) were further categorised as patients with normoglycemia (group A1 [n = 806, 27.0%] and B1 [n = 1815, 26.3%]), prediabetes (group A2 [n = 935, 31.3%] and B2 [n = 2145, 31.0%]), and T2DM (group A3 [n = 1243, 41.7%] and B3 [n = 2949, 42.7%]) (Figure 1). The major outcomes were the incident of major adverse cardiac events (MACE), described as all-cause death, recurrent myocardial infarction (Re-MI), or any repeat coronary revascularization.
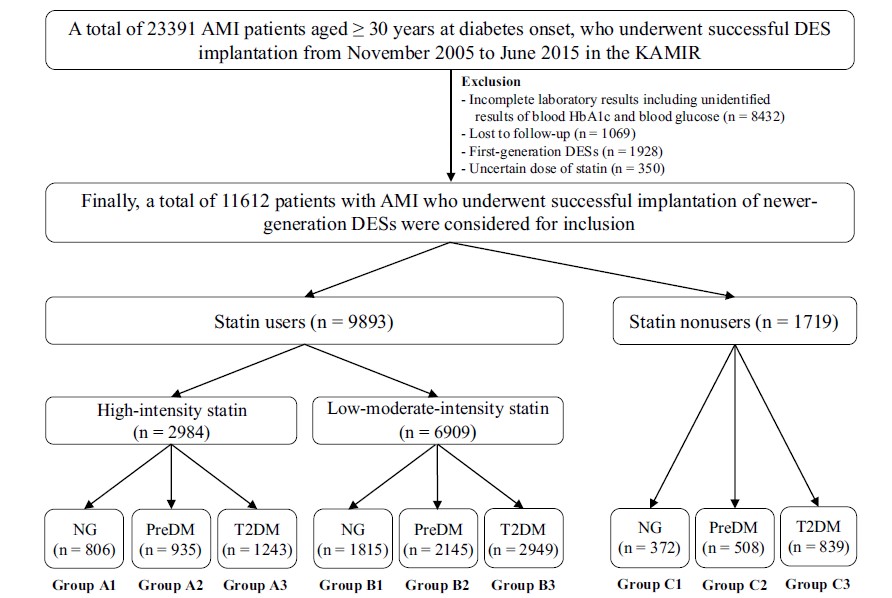
Figure 1: Flowchart showing the patient selection process for the study.
AMI: Acute myocardial infarction; DES: Drug-eluting stents; KAMIR: Korea AMI Registry; NG: Normoglycemia; PreDM: Prediabetes; T2DM: Type 2 diabetes mellitus.
In high-intensity statin users, group A2 (prediabetes) showed higher cumulative incidences of MACE (adjusted hazard ratio [aHR]: 2.187; 95% confidence interval [CI]: 1.341–3.569; p = 0.002) and any repeat revascularization (aHR 3.009; 95% CI 1.342–6.745; p = 0.006) as compared to group A1 (normoglycemia). Similarly, group A3 (T2DM) showed the substantially higher cumulative incidences of MACE (aHR 2.368; 95% CI 1.480–3.788; p = 0.001) and any repeat revascularization (aHR 3.619; 95% CI 1.659–7.898; p = 0.001) as compared to group A1 (Table 2) (Figure 2).
Table 2: Clinical outcomes in high-intensity or low-moderate-intensity statin users at 2 years
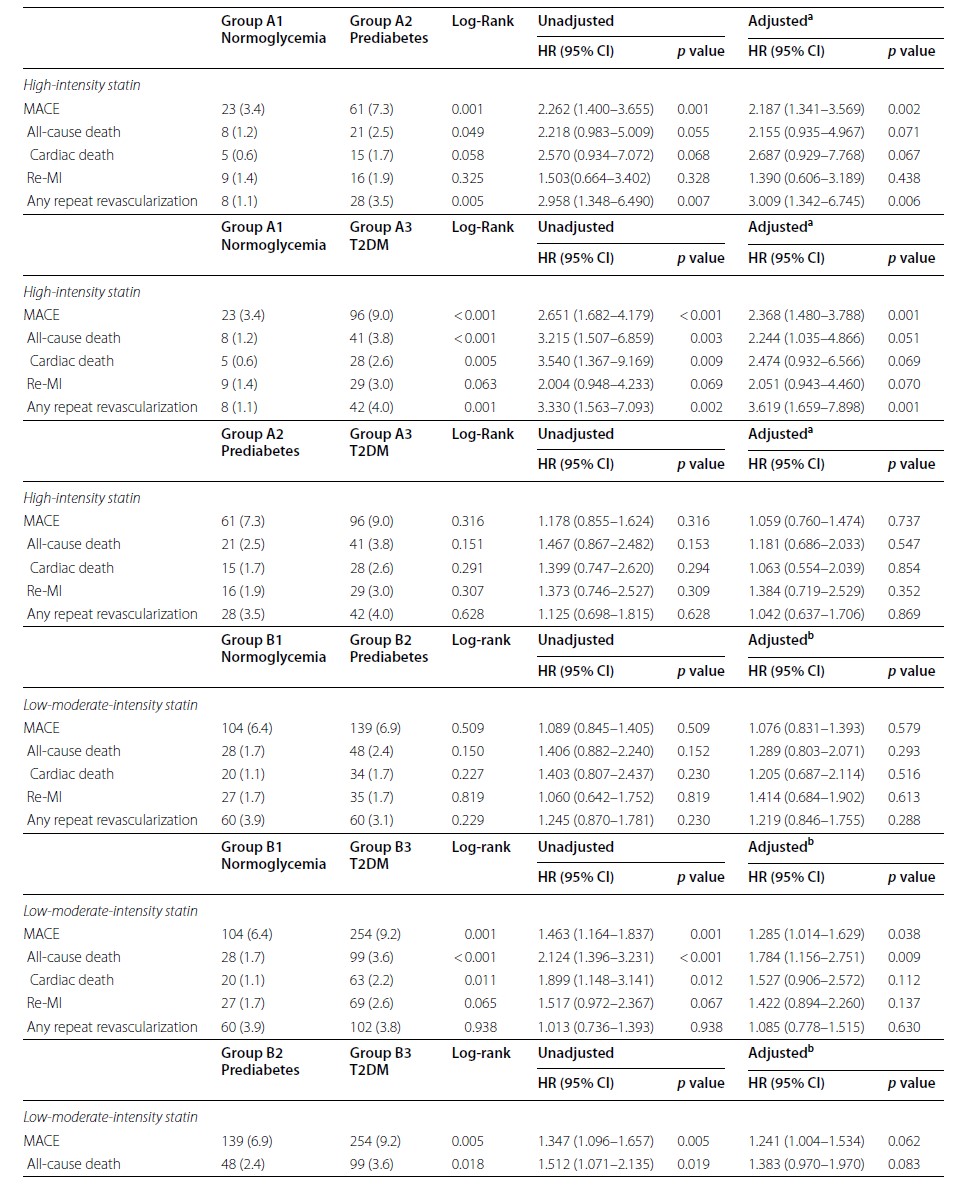
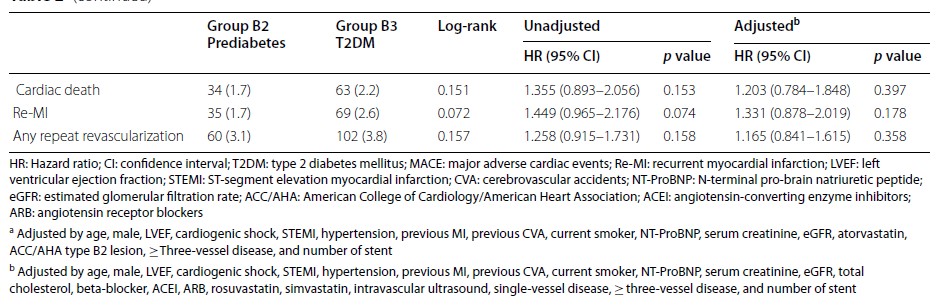
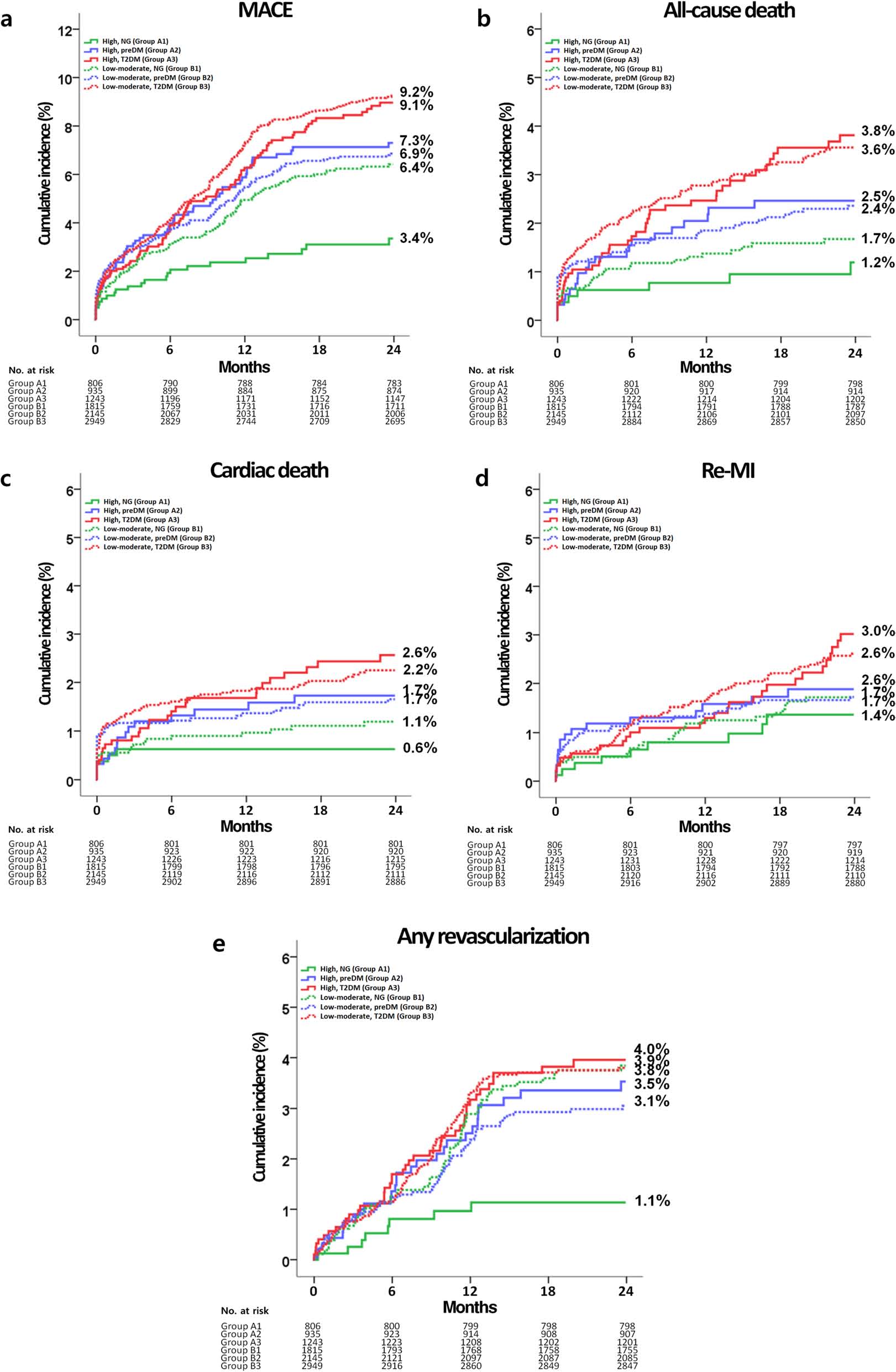
Figure 2: Kaplan–Meier analyses for the MACE (a), all-cause death (b), cardiac death (c), Re-MI (d), any repeat revascularization (e) in statin users.
MACE: Major adverse cardiac events; Re-MI: Recurrent myocardial infarction, High: High-intensity statin; Low-moderate: Low-moderate-intensity statin; NG: Normoglycemia; preDM: Prediabetes; T2DM: Type 2 diabetes mellitus
In the total study population, both high-intensity and low-moderate intensity statin therapies exhibited comparable findings. But, in the patients who enlisted following October 2012, high-intensity statin users showed substantially lower cumulative incidences of MACE (aHR 1.533; 95% CI 1.144–2.053; p = 0.004) and any repeat revascularization (aHR, 1.587; 95% CI 1.026–2.456; p = 0.038) as compared to low-moderate intensity statin users. The advantageous impacts of high-intensity than low-moderate-intensity statin treatment were more evident in the normoglycemia group as compared to hyperglycemia group, as it decreased the cumulative incidences of MACE (aHR 1.903; 95% CI 1.203–3.010; p = 0.006) and any repeat revascularization (aHR 3.248; 95% CI 1.539–6.854; p = 0.002).
Prediabetes and T2DM groups exhibited comparable clinical effects, following both high-intensity and low-moderate-intensity statin therapies in this retrospective registry study. Additionally, the normoglycemia group had more evident advantageous impacts of high intensity than low-moderate-intensity statin treatment as compared to the prediabetes and T2DM groups. But, these findings are likely to be clearly proved by further studies, specifically in patients with AMI who are being managed in contemporary practice.

