Yugar-Toledo JC. Curr Hypertens Rep. 2018 Mar 27;20(3):26.
Uncontrolled resistant hypertension (UC-RHTN) is defined as a blood pressure (BP) that remains above the desired level (140/90 mmHg) in spite of the concurrent use of three or more antihypertensive agents of different classes. Controlled resistant hypertension (C-RHTN) is defined as a blood pressure (BP) is controlled using four or more antihypertensive medications.
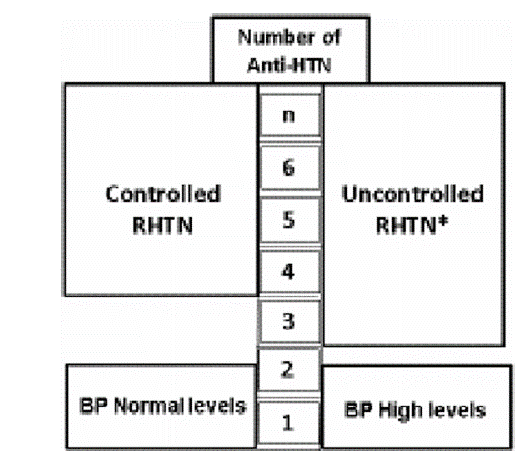
Figure 1: Definition of controlled (C-RHTN) and uncontrolled resistant hypertension (UC-RHTN)
Clinical evidence:
Yugar-Toledo JC et al., conducted a study which reviewed the issue dividing resistant hypertension as controlled (C-RHTN) and uncontrolled (UC-RHTN) resistant hypertension with refractory hypertension (RfHTN), an extreme phenotype of uncontrolled hypertension (taking 5 or more antihypertensive drugs) being included in the latter subgroup (UC-RHTN). Some characteristics of isolated RfHTN are highlighted below.
Pathophysiological Issues
C-RHTN occurrs to be more dependent on the volemic status than uncontrolled UC-RHTN due to the important involvement of persistent fluid retention, increased sodium sensitivity, excessive salt intake, hyperaldosteronism, and a certain degree of renal dysfunction.
- UC-RHTN seems to have additional pathophysiological mechanisms in contrast to C-RHTN, and may not be exclusively volume-dependent
- UC-RHTN patients regularly have sympathetic nervous system hyperactivity as evidenced by measurement of 24-h urinary metanephrines, increased resting heart rate (HR); increased HR variability during 24-h EKG monitoring (spectral analysis); increased arterial stiffness inferred by pulse wave velocity (PWV); increased arterial resistance
- RHTN patients had higher levels of TNF-α compared to normotensive individuals
- Higher PWV values indicated an increased arterial stiffness and elevated cytokine levels including TNF-α may bring about the vascular damage in RHTN
- UC-RHTN individuals showed more pronounced aforementioned mechanisms than in C-RHTN patients
Clinical Differences
- 133 consecutive patients were included in a study for RHTN treatment
- All the individuals had a complete case report and underwent a physical examination, electrocardiography, and laboratory tests to eliminate secondary forms of hypertension
- 90 individuals were classified as RHTN patients after a 6-month period (five to six visits)
- They were divided into two subgroups were uncontrolled (UC-RHTN; n = 47) and controlled (CRHTN; n = 43) RHTN patients and plasma aldosterone concentration (PAC)
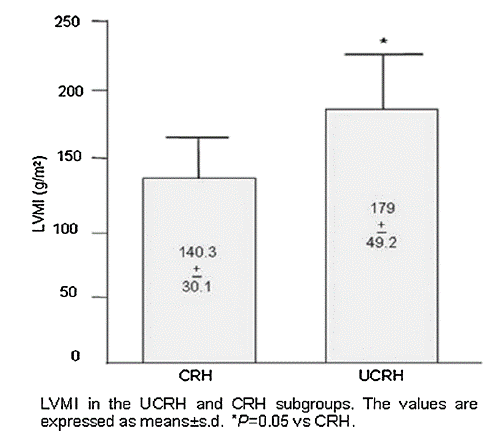
Figure 2: LVMI in the UCRH and CRH subgroups
- UC-RHTN patients showed higher body mass index (BMI), vascular stiffness, plasma aldosterone levels, and left ventricle hypertrophy (LVH) as compared to C-RHTN (Fig. 2)
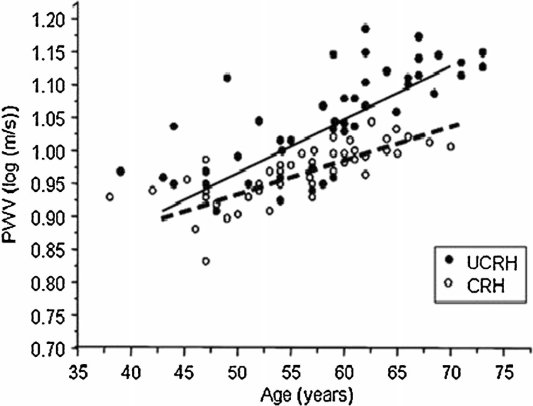
Figure 3: Multivariate linear regression for PWV with respect to age
- PWV was appeared to be dependent on age in both UC-RHTN and C-RHTN patients in multivariate analysis, although the influence of aging was more important in the UC-RHTN (Fig. 3)
- UC-RHTN patients had higher carotid intima-media thickness (IMT) and PWV, reflecting thicker and stiffer arteries after one year
- PWV was significantly dependent on age in RHTN patients in multivariate linear regression (β = 0.005; s.e. = 0.001; p < 0.05). UCRHTN patients had stiffer arteries and higher left ventricular mass index in all age strata.
Cardiovascular Outcomes
- The occurrence of fatal and nonfatal cardiovascular events was estimated in 340 patients with controlled hypertension and 130 RHTN subjects
- The event rates per 100 patient-years were 0.87 and 4.1, resp. during the follow-up period.
- Patients with UC-RHTN had a higher risk of coronary artery disease, stroke, peripheral arteriopathy, heart failure, renal disease, and all-cause mortality as compared to C-RHTN patients
Risk of Refractoriness
- 116 RHTN patients from a specialized clinic subdivided as RHTN (n = 80) and RfHTN (n = 36). All patients were submitted to echocardiography, 24-h ambulatory BP monitoring, and biochemical analyses.
- No differences were found between the groups regarding age, gender, body mass index, biochemical parameters, and comorbidities.
- Logistic regression analysis exhibited that the white-coat effect (p = 0.03), Black race (p < 0.001), and left ventricular mass index (p = 0.04) were independent predictors of refractoriness
Thus, it was concluded that UC-RHTN and C-RHTN are not in the same bag. Both C-RHTN and UC-RHTN are extreme phenotypes of hard-to-control BP but some mechanisms of the disease and clinical expressions are distinct.

