Pujol C, et al. International Journal of Cardiology. 2020 Feb;300:127-131.
Arrhythmias are a leading cause of hospitalization in adults with congenital heart disease (ACHD), and increase the risk of thromboembolic events and the risk of death by 50%. The incidence of ischemic strokes in ACHD under 55 years of age is 9-12 times higher compared to the general population, and 2 to 4 times higher in the age group between 55 and 64 years. More than 20% of ACHD needs some form of oral anticoagulation (OAC) during their lifetime. However, the risk of haemorrhagic stroke in ACHD is 8 times higher than in the general population. According to the international expert consensus on recognition and management of arrhythmias in ACHD, all patients with a moderate or complex CHD, and all those with simple defects but a CHA2DS2-VASc score > 2 require anticoagulation. Most commonly used OAC are vitamin-K antagonists like warfarin or phenprocoumon. Direct oral anticoagulants (DOACs) are an established alternative to vitamin-K antagonists for patients with acquired cardiovascular disease requiring anticoagulation with the exemption of those with mechanical heart valve prosthesis.
Pujol C, et al. conducted a study to analyse the effectiveness and safety of DOACs in ACHD patients at mid-term follow-up. A total of 215 ACHD patients (111 females, 48.4 ± 15.5 years) were included into the study. All ACHD under DOACs were retrospectively identified. Bleeding and thromboembolic events was noted. CHADS2, CHA2DS2-VASc and HASBLED scores were calculated and risk factors for bleeding and thromboembolic events were identified.
In the retrospective study it was observed that CHD was severe in 44.2%, moderate in 23.7%, and simple in 32.1%. Indications for anticoagulation were: atrial arrhythmias (66.8%), cerebrovascular accidents (32.7%), pulmonary thromboembolism (3.7%), deep vein thrombosis (11.2%), atrial thrombi (6.5%), and Fontan circulation/TCPC (5.6%). Mean follow-up was 15.8 ± 15.8 months. Nine patients suffered a major, eight a minor bleeding and thromboembolic events occurred in two patients. The annual risk for bleeding was 3.1%/patient/year and for thromboembolic events 0.7%/patient/year. In the univariate analysis, a CHADS2-Score >2 (HR 1.46, CI [1.03e2.05], p < 0.05), a HASBLED score > 3 (HR 1.83, CI [1.30e2.59], p < 0.001), and renal disease (HR 16.58, CI [4.09e67.22], p < 0.001) were identified as risk factors for bleeding (minor and major bleeding) under DOAC. In the multivariate analysis, renal disease remained as an independent predictor for bleeding (HR 6.13, CI [1.04e36.27], p < 0.05). It was also the only risk factor for major bleedings (HR 13.75, CI [2.60e72.54], p = 0.002). Risk factors for thromboembolic events were not identified (Figure 1).
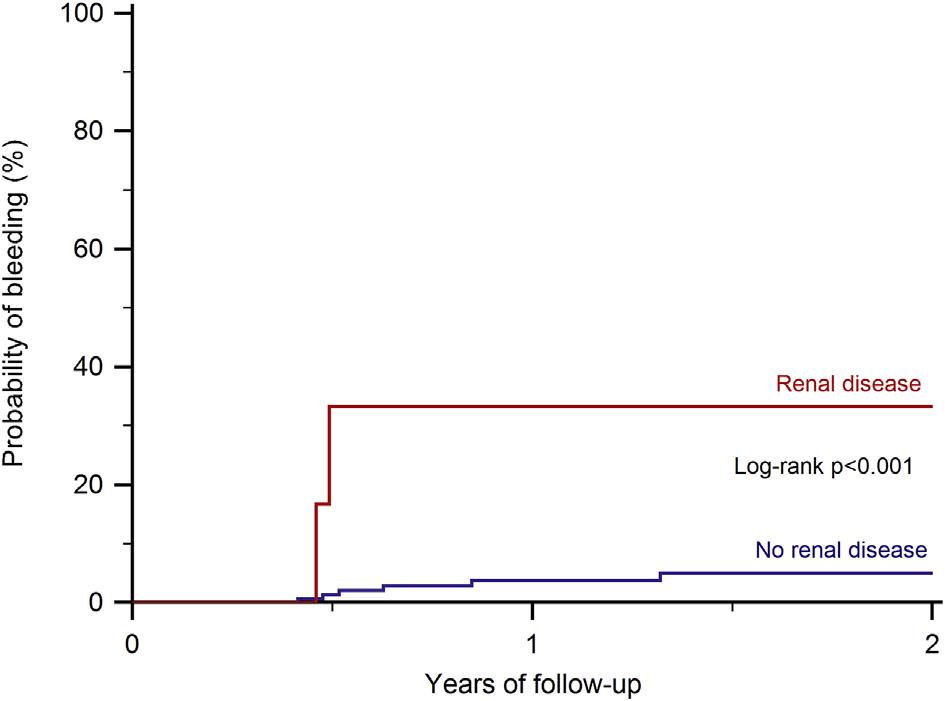
Figure 1: Kaplan-Meier curves for bleeding events in ACHD patients under DOAC therapy stratifying patients by presence of renal disease
Thus, DOACs have been proven to be safe and effective in patients with acquired heart disease. A low rate of thromboembolic events was observed in ACHD patients under DOAC therapy. Bleeding complications were not negligible. Special attention has to be paid to those patients with advanced renal failure.

