Uric acid: A biomarker or risk factor for disease – The answer is here Why is uric acid a potential target for complications?
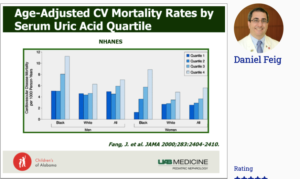
Feig D, presented a session at the 56th EASD Annual Meeting conducted virtually, to understand uric acid as biomarker or risk factor for diseases. The relevance of uric acid dates back to 1896, when Alexander Haig in a 572 page treatise, described that elevated serum uric acid was detectable in many patients with chronic, non-infectious disease. In a study conducted in black and white males and females, it was observed that the highest quartile of uric acid were substantially associated with increased risk of CV mortality. As per a study conducted by Watandbe et al., in rats, it was observed that mild hyperuricemia in rats acutely increases blood pressure (BP) by a renin-dependent mechanism which is majorly manifested under low-salt dietary conditions. Chronic hyperuricemia also causes salt sensitivity, in part by inducing preglomerular vascular disease. Uric acid causes reversible vasoconstriction via increase in renin and decrease in nitric oxide (NO) and arteriolar wall thickening via vascular smooth muscle proliferation mediated by PDGF and MCP-1. Reduction of uric acid lowers BP, has been confirmed in a crossover study of adolescents with newly diagnosed hypertension, where treatment with allopurinol resulted in reduction of BP. Uric acid lowering therapy also lowers BP in young adults who are non-smokers and have normal renal function. In contrast to animal experiments and observational studies, trial conducted by Forman et al., found that uric acid lowering had no effect on kidney-specific or systemic RAAS activity after 8 weeks or on mean systolic BP. These data do not support the hypothesis that higher levels of uric acid are a reversible risk factor for increased BP. As per a study, conducted by Hovind et al., uric acid level soon after onset of type 1 diabetes is independently associated with risk for later development of diabetic nephropathy.
Conclusion: Uric acid lowering therapy, regardless of mechanism, lowers BP in adolescents with elevated BP. Uric acid lowering therapy has little or no BP impact on older adults and patients with advanced CKD. In CKD trials uric acid lowering has little effect in older patients than those with more advanced CKD. Younger patients and those with less severe CKD appear to have improvement in GFR with uric acid lowering therapy consistently with model of 2 step vasculopathy.
ESC vs EASD/ADA-guidelines on diabetes and cardiovascular disease: Same evidence but different interpretations – Who’s right? The diabetologists
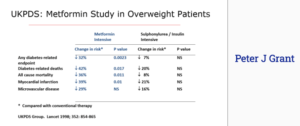
Grant PJ, presented a session at the 56th EASD Annual Meeting conducted virtually, to understand the evidence on ESC vs. EASD/ADA guidelines on diabetes and cardiovascular disease from the perspective of diabetologists. Since the results of UKPDS trial till date, Metformin has been recommended as monotherapy by all International guidelines for newly diagnosed T2DM. Several studies have investigated the association between glycemic control and prevention of CVD. DCCT trial in type 1 diabetes showed decrease in CVD at 12-20 years, Da Qing study in pre-diabetes showed decrease in CVD at 23 years and the UKPDS, VADT studies showed decrease in CVD after 8-15 years. Among the drugs used for diabetes treatment, SGLT-2 inhibitors have undoubtedly shown excellent results in CV outcomes and renal outcomes. The 2019 ESC guidelines on diabetes, pre-diabetes, and CVD developed in collaboration with the EASD recommends use of SGLT-2i or GLP-1 RA monotherapy in patients with ASCVD or high and or very high CV risk. Diabetes targets both the large and smaller blood vessels causing macrovascular and microvascular complications respectively. In a cross sectional study, 68% of people with type 2 diabetes suffered from at least one complication. Diabetes complications have known to contribute to poor quality of life and poor well-being. Insulin resistance in diabetes causes an inflammatory atherothrombotic syndrome causing hyperglycaemia, hyperinsulinaemia, hypertension, elevated levels of triglyceride and cholesterol. From the perspective of a diabetologist, heart failure may be improved partly due to renal function, partly through lowering of BP and partly through improvement of interstitial fluid. The coronary composition in atherectomy specimens from patients with diabetes mellitus reveal presence of greater area of lipid-rich atheroma, macrophage infiltration and excessive thrombus. Around 62% of diabetes patients show presence of thrombus vs. 42% of non-diabetic patients. Metformin has shown beneficial results on cardiovascular outcomes in several trials. Metformin has shown an advantage over sulphonylurea and insulin therapy in reducing diabetes related endpoints, diabetes related deaths, all-cause mortality, myocardial infarction and microvascular disease.
Conclusion: Several advantages have been observed with metformin while making indirect comparison with SGLT-2i. Metformin is inexpensive as compared to SGLT-2i; the legacy of metformin efficacy has been documented in several trials; the mechanism of action and side effects of metformin is known; several patients have been using metformin since years, a feat SGLT-2i is yet to achieve; the interaction of metformin with other anti-diabetic drugs is widely understood; metformin improves microvascular outcomes, CV outcomes and quality of life. On the contrary, SGLT-2i have no known effects on microvascular outcomes and quality of life.
EASD/AASD Symposium: Implementation science in diabetes AASD/IDF-WPR Diabetic Foot Guidelines: Implementation in Asia and WPR
Kono S, presented a session at the 56th EASD Annual Meeting conducted virtually, which reviewed the AASD/IDF-WPR Diabetic Foot Guidelines. The session revolved around revisiting the history of organisation of network of “Diabetic foot”, outlining the characteristics of diabetic foot problems in Western Pacific Region (WPR), regional recommendations for management of diabetic foot problems from AASD and implementation of regional recommendation in Asia and WPR. Kono highlighted the common foot problems in WPR like the scarcity of foot care specialists as well as foot wear specialists, lack of trained nurses, unhealthy lifestyle in WPR and obstacles in application of international guidelines to people in WPR. The action plan involved recognising the core hospital of diabetic foot care as IDF-WPR recognised foot center (IDF-WPR DFC), organising the network system of IDF-WPR DFC to support inter and intra-national, evaluating regional characteristics of diabetic foot in WPR, developing regional clinical recommendations and guidelines directly applicable to the regional lifestyle and conduct health promotion with WHO and SPC (The Pacific community). The AASD and the IDF-WPR group conducted prospective observational study of diabetic foot in WPR at recognised diabetic foot centers and tertiary care hospitals. 30 patients were treated at each hospital. The results observed were the presence of aerobic and anaerobic bacteria in 38.7% and only aerobic bacteria were seen in 61.8% cases. Staphyloccus supp. (48.6%), MRSA (8.8%), Streptococcus spp. (13.3%), Enterococcus spp. (11%), Proteus spp. (11%), were the predominant pathogens obtained from the diabetic foot culture specimens. Amputation was performed in 27% of the cases. The recommendations to improve management of diabetic foot disease in WPR included:
- Education about preventive foot care
- Raising HCP skill at screening for neuropathy and PAD at earlier stage to help prevent progression to sensory-loss and critical limb-threatening ischemia
- Raise HCP skills in assessing pre-ulcerative lesions and ulcers, including precipitating and predisposing factors
- Raising HCP skills in managing diabetic foot infection (DFI), isolation of pathogens, sensitivity testing to antibiotics essential in treating most DFI
- Raising skiils in DFU wound management, debridement, pressure-offloading and in surgical revascularisation and orthopaedic treatments
- Organise networks/systems for timely and progressive referral and for hospitalisation for DFU
- Ensuring periodic, appropriate follow-up management for DFU patients to ensure DFU resolution and to prevent recurrence

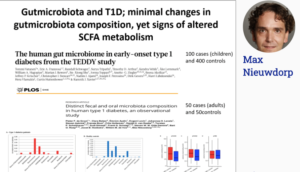
Targeting the gut to treat diabetes: How can the gut help us to treat diabetes
Nieuwdorp M, presented a session at the 56th EASD Annual Meeting conducted virtually which discussed effect of intestinal microbiota in type 1 diabetes (T1D) and type 2 diabetes (T2D) patients. In T1D, the small intestine is exposed to bacteria and pathogens; in T2D, fermentation takes place in the large intestine. In T2D, the pathogens are more, but less diverse. There is limited information about microbiota in T1D. In TEDDY study, distinct microbial changes were observed in T1D with altered short-chain fatty acids (SCFA) metabolism. Currently around 300 trials are ongoing with FMT (Fecal Microbiota Transplantation). 10 trials were on FMT in obesity and 3 trials on FMT in NAFLD/NASH. For T1D and T2D, the microbiota disease modifier can slow down the disease process by altering autoimmune profile. Allogenic FMT using METS-D decreases insulin sensitivity in metabolic syndrome recipients when compared with using post- Roux-en-Y gastric bypass donors (RYGB-D). The efficacy of FMT varies with studies but shows similar effects of oral diabetes medications on insulin sensitivity. 80% of T2D patients have NAFLD and modulation of gut microbiota drives NAFLD-NASH progression as observed in animal models. A randomized controlled trial on new onset T1D studied the effect of FMT on residual beta cell preservation showed residual beta cell function stabilises upon autologous and to a lesser extent with allogenic donor FMT. No effect of oral butyrate was shown on residual beta cell function as compared to placebo in T1D. Oral butyrate negatively affects gutbrain by reducing serotonin and dopamin receptor binding (in hypothalamus and striatum), whereas donor FMT improves this. Replenishing missing intestinal microbiota or supplementation with (immunomodulatory) bacterial strains stabilizes residual beta-cell function in and insulin sensitivity in T2D.
Conclusion: Intestinal microbiota are related with T1D and T2D. FMT is an infection modifiers and changes the cause for the disease yet never invert the disease in T1D and T2D from group to singular (responders-non responders). Oral butyrate supplementation doesn’t improve autoimmunity in T1D nor insulin affectability and gutbrain axis in T2D. Nonetheless, treatment with missing intestinal bacterial strains may show advantageous impacts on T1D and T2D in specific subgroups. The subsequent stage can be to consolidate numerous strains distinctive for each kind of diabetes and attempt to essentially involve gainful impact in the patients.
Semaglutide for the treatment of obesity (STEP-programme) From proof of concept: Semaglutide
Davies MJ, presented a session at the 56th EASD Annual Meeting conducted virtually, which explored the data on Semaglutide. Semaglutide showed improved albumin binding, DPP-4 stability, brain access and is less lipophilic as compared to Liraglutide. On comparing different trials of GLP-RAs in T2D, SUSTAIN trial demonstrated critical weight reduction with semaglutide than other trials. A trial of Semaglutide in patients with obesity in which different doses ranging from 0.05 mg to 0.4 mg of Semaglutide and 3 mg of Liraglutide were given to different groups of patients. Compared to placebo group, semaglutide demonstrated dose-dependent noteworthy reduction (13.8%) in body weight. The on treatment adverse events were similar as that of other GLP-RAs. Translating Phase 2 trial into phase 3 trial in which changing daily administration to weekly administration of Semaglutide showed similar results in phase 3 with dose escalation upto 2.4 mg/week as in phase 2 with dose escalation of 0.4 mg/day. There are 2 estimands in STEP programme i.e. primary and secondary. Primary estimand was the effect of getting the drug prescribed ‘intended to treat’ and for those who make decisions about group of patients e.g. regulators. Secondary estimand was the effect of taking drug as intended (average effect of exposure), for those who make decisions about individual patients e.g. physicians. The baseline characteristics are extensively comparable in in STEP1 to STEP4 apart from STEP2 which is a study of T2D patients in which gender balance is 50%. In STEP2 trial patients with diabetes had HbA1c of 8.1%. In STEP1, Semaglutide showed significant reduction in body weight in both treatment policy estimand and trial product estimand by 14.9% and 16.9% respectively. In STEP2, Semaglutide showed substantial decrease in body weight in both treatment policy estimand and trial product estimand, however lesser results were shown in patients with diabetes compared to patients without diabetes. In STEP3 likewise, significant reduction in body weight was seen. In STEP4, significant reduction was seen with Semaglutide while weight gain was seen with placebo administration.
Conclusion: Topline results from the STEP Programme demonstrate that in overweight and obese adults, Semaglutide 2.4 mg QW versus placebo shows a clinically significant decrease in body weight.

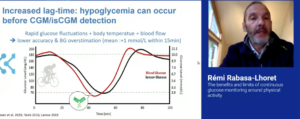
Diabetes on the run: insulin therapy in type 1 diabetes and exercise: The benefits and limits of continuous glucose monitoring around physical activity
Rabasa-Lhoret R, presented a session at the 56th EASD Annual Meeting conducted virtually, which investigated the benefits and limits of continuous glucose monitoring during physical activity. Before initiating continuous glucose monitoring (CGM), the exercise experience and hypoglycaemia risk should be assessed. CGM should be used to adjust insulin and/or CHO intake before exercise. The 3 groups i.e. Ex2 with low hypoglycaemia risk, Ex1 with moderate hypoglycaemia risk and Ex0 with high hypoglycaemia risk were enrolled in the T1D pre-exercise sensor glucose group. The criterion for blood glucose range was not above >270 mg/dL. It is possible that hypoglycaemia can occur before CGM detection with rapid fluctuation in glucose, body temperature and blood flow with increase lag time. Other limitations in exercise include adhesion, sensor location, lost signal missed data, hypoglycaemia over correction, alarm setting and fatigue. The sensor augmented pump therapies are predictive of low glucose suspend and hybrid closed loop systems. Predictive low glucose suspend therapy is not suitable to deal with exercise induced rapid glucose drop and is efficient for post exercise hypoglycaemic risk. Hybrid closed loop systems reduces hypoglycaemic risk. There are some specific sports such as swimming in which waterproof bag is needed or liquid gel or tablets can be used. In high altitude sports CGM is reliable upto 3.600m and can show impact of temperature on glucose sensor and insulin.
Conclusion: Physical activity is a key component of life and T1D management. Physical activity can induce glucose fluctuations. CGM facilitates key decisions such as insulin adjustments and CHO intake and also facilitates hypoglycaemia prevention and diagnosis.
Effects of intensive risk factor management on cardiovascular autonomic neuropathy in type 2 diabetes: Findings from the ACCORD clinical trial
Pop-Busui R, presented a study report at the 56th EASD Annual Meeting conducted virtually, to examine the effect of intensively targeting traditional risk factors for Cardiovascular autonomic neuropathy (CAN), including hyperglycemia, hypertension, and dyslipidemia, in persons with T2D and high CV risk participating in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. CAN is a common complication that independently predicts cardiovascular (CV) morbidity and mortality in persons with type 2 diabetes (T2D). The effects of preventive interventions on CAN remain unclear. CAN was defined as heart rate variability indices below the 5th percentile of the normal distribution (standard deviation of all normal-to-normal R-R intervals [SDNN] <8.2 ms and root mean square of successive differences between normal-to-normal R-R intervals [rMSSD] <8.0 ms). Of the 10,250 ACCORD participants, 71% (n=7,275) had valid CAN evaluations at study entry and at least once after randomization. The effects of intensive interventions on CAN were tested among these subjects by means of generalized linear mixed models. The results observed were: when compared to standard treatment, the intensive glycemia intervention significantly reduced CAN risk during the entire duration of the study (OR=0.84, 95% CI 0.75 – 0.94, p=0.003). This effect was present among individuals with no cardiovascular disease (CVD) history (OR= 0.73, 95%CI 0.63 – 0.85, p<0.0001) but not among those with a positive CVD history (OR=1.10, 95% CI 0.91 – 1.34, p=0.34) (p for interaction=0.001). Intensive BP therapy also decreased the odds of CAN (OR=0.75, 95% CI 0.63 – 0.89, p=0.001), with no evidence of heterogeneity based on CVD history or other clinical characteristics. Fenofibrate did not have a significant impact on CAN outcome (OR=0.91, 95%CI 0.78 – 1.07, p=0.26). No significant interactions were observed between treatment strategies.
Conclusion: The beneficial effect of intensive glycemic therapy was confirmed in this study and for the first time, a similar benefit of intensive BP control was demonstrated on CAN in T2D. They also suggest that a negative CVD history could be used as a criterion to select those T2D patients who would most benefit from intensive glycemic control for control for CAN prevention, whereas BP control is effective regardless of CVD history.
Effects of 5 weeks of treatment with dapagliflozin, a SGLT2 inhibitor, on energy metabolism in patients with type 2 diabetes
Op den Kamp Y, presented a study report at the 56th EASD Annual Meeting conducted virtually to explore the effects of dapagliflozin (DAPA) on insulin sensitivity, 24h energy metabolism and skeletal muscle mitochondrial function in patients with type 2 diabetes (T2D). Twenty-six T2D patients with HbA1c between 42 and 75 mmol/mol, were randomized to a double blind, cross-over study. Examinations were done at the end of the 5-week treatment periods, separatedby 6-8-week wash-out. 24h energy- and substrate metabolism was measured in respiration chambers, and blood was sampled at 7 time points. A two-step euglycemic hyperinsulinemic clamp (10 and 40 mU/m /min) with infusionof [6.6-2H2] glucose to determine glucose rate of disposal (Rd), endogenous glucose production (EGP) and indirect calorimetry was performed. Intramyocellular (IMCL), intrahepatic lipid (IHL) content and resting and post-exercise (70% Wmax) muscle acetylcarnitine were analysed by H-Magnetic Resonance Spectroscopy (MRS). Phosphocreatine recovery upon exercise was measured by P-MRS and body composition by DEXA. Ex vivo mitochondrial respiration was measured in a muscle biopsy taken after overnight fast. The results observed were: DAPA decreased total body weight (-1.12 (-1.66, -0.58) kg, p<0.01). Rd was unaffected by DAPA, while fasting EGP increased (+2.27 (1.39, 3.14) μmol/kg/min, p<0.01), EGP upon insulin infusion was unchanged. A trend towards a larger increase in carbohydrate oxidation (+0.77 (-0.37, 1.91) μmol/kg/min, p=0.11) and a larger decrease in fatty acid oxidation (-0.28(-0.65, 0.09) μmol/kg/min, p=0.13) upon insulin infusion was observed. 24h energy expenditure (-0.11 (-0.24, 0.03)MJ/day), sleeping metabolic rate or diet-induced thermogenesis were unaffected by DAPA. DAPA reduced RER during day- (-0.024 (-0.034, -0.014), p<0.01) and night-time (-0.033 (-0.046, -0.020), p<0.01). Day-time glucose was lower (p<0.01), while free fatty acids (p<0.01) and β-hydroxybutyrate (p<0.05) levels were higher upon DAPA. On placebo, urinary glucose loss was neglectable, whereas DAPA induced a 24h glucose loss of about 90g; rate of glucose loss was 50% lower during the night compared to daytime. IMCL increased upon DAPA (+0.06 (0.01, 0.11)%, p<0.05), whereas IHL decreased (-0.29 (-2.53, 1.94) %, p<0.05). DAPA had no effect on ex vivo mitochondrial respiration, phosphocreatine recovery rate or acetylcarnitine metabolism.
Conclusion: Five weeks dapagliflozin treatment in T2D patients had no effect on insulin sensitivity or energy expenditure, while 24h fatty acid oxidation was increased. A trend towards improved metabolic flexibility was observed. Intramyocellular lipids were increased and intrahepatic lipids decreased, but skeletal muscle mitochondrial function was not changed by dapagliflozin treatment.
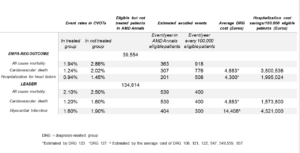
Estimation of hospitalisations cost savings deriving from a wider application of EMPAREG and LEADER inclusion criteria in the real world practice: data from AMD Annals
Porto Da A, presented a study report at the 56th EASD Annual Meeting conducted virtually to quantify the proportion of patients potentially eligible for the EMPA-REG and LEADER studies and to estimate the potential impact on reduction of MACE, HHF and corresponding cost savings resulting if the use of these treatments would have been extended to all eligible patients. In Italy, an initiative of continuous monitoring and quality improvement of diabetes care (AMD Annals) is in place since 2004 promoted by the scientific society of diabetologists (AMD). A network of diabetes centers periodically extracts anonymous data from electronic clinical records for the continuous monitoring of quality of care. The same selection criteria used for recruiting patients in EMPAREG-Outcome and LEADER studies were applied to the AMD Annals population. Reduction in absolute risk of cardiovascular death and hospitalization for heart failure or myocardial infarction was associated with the use of the drugs if all eligible patients had been treated were estimated on the basis of rates shown in the EMPA-REG OUTCOME and LEADER trials. Hospitalization cost savings were estimated from national reference cost in 2018 for diagnosis related group codes (DRG). From the AMD-database including 468,940 patients seen in 222 Diabetes Clinics in 2016, 342,190 had all the data required for evaluating the eligibility for both EMPA-REG and LEADER study. The results observed were: 41,715 patients met the eligibility criteria for EMPAREG study and 139,637 for LEADER study. Although theoretically eligible, in real world setting only 2,161 patients (5.2%) were currently treated with empagliflozin and 4,823 (3.5%) with liraglutide. Estimate numbers of prevented events and potential cost savings are summarized in table 1.
Conclusion: Despite the fact that CVOTs results provide evidence that use of empagliflozin and liraglutide are associated with reduced cardiovascular morbidity and mortality, only a minimal portion of eligible patients are on treatment with these drugs in a real world setting. This cost analysis suggests that a wider use of empagliflozin and liraglutide in patient meeting CVOT eligibility criteria would result in a significant reduction of CV event rate and consequent relevant hospitalization cost saving.
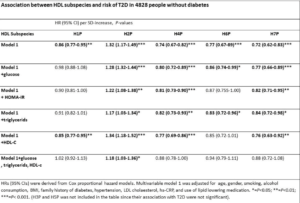
Characterisation of seven HDL subspecies and their association with incident type 2 diabetes in PREVEND study
Oskooei SS, presented a study at the 56th EASD Annual Meeting conducted virtually to investigate seven HDL subspecies and evaluate their association with incident T2D. 4828 subjects of the Prevention of Renal and Vascular End-Stage Disease (PREVEND) study without T2D at baseline were included. HDL subspecies with increasing size from H1P to H7P were measured using the LP4 algorithm of the Vantera NMR platform. Insulin resistance was determined by homeostatic model assessment index (HOMA-IR). The results observed were: among the seven HDL subspecies, H1P, H3P, H4P, H6P, and H7P were inversely associated with HOMA-IR, whereas H2P was positively associated with HOMA-IR. During a median follow-up of 7.3 years, 265 individuals developed T2D. In multivariable-adjusted Cox regression models, higher levels of H1P, H4P, H6P, and H7P were associated with a lower risk of developing T2D, independent of adjustment for baseline covariates, including age, gender, lifestyle, use of medication, BMI, and hypertension. Oppositely, higher levels of H2P were associated with an increased risk of developing T2D. The associations for H2P, H4P, H6P, and H7P remained independent of further additional adjustment for glucose and triglycerides. Moreover, the association of H6P was not independent of HDL cholesterol. In the last model, with adjustment for all relevant variables, H2P was the only subspecies that remained significant, with a positive association with T2D development.
Conclusion: H2P, the predominant HDL subspecies, was positively associated with metabolic factors including HOMA-IR and triglycerides. Additionally, H4P and H7P levels showed the strongest inverse association with incident T2D, whereas H2P levels were positively associated with incident T2D, independent of clinical risk factors.
Effects of patient-initiated visits in the diabetes outpatient clinic: 2 year RCT (DIATAST – the DIAbetes patient TAkes reSponsibiliTy
Drojdahl Ryg N, presented a study at the 56th EASD Annual Meeting conducted virtually to report the effects of patient-initiated visits in the diabetes outpatient clinic on 1) Patient reported experience measures (PREM), 2) Clinical diabetes variables and 3) Number of contacts to the outpatient clinics. Adults with T1DM for more than 6 months, who were internet users, were included. Patients with unstable diabetic complications, large increase in HbA1c within the past 6 months, or found non-eligible because of frailty were excluded. After informed consent and collection of baseline data, patients wererandomized (1:1) to two years intervention with 1) Patient-initiated visits and push reminders every 3 month (INT) or 2) Usual care with pre-scheduled visits (CON). The primary outcome was PREM evaluated by a self-designed questionnaire (5-point Likert scale). Questions were focused on 1) accessibility of the outpatient clinic, 2) the benefit of the consultation and, 3) overall patient satisfaction with the use of the outpatient clinic. Secondary outcomes included Hba1c and other clinical diabetes variables and use of resources in the outpatient clinic. All data were corrected for age, sex, diabetes duration (+/- 5 years), and insulin administration (pump/injection). Of 849 patients screened, 596 were found eligible, and 357 accepted inclusion (INT: 178/CON: 179). The results observed were after 2 years, more patients in the intervention group reported to be able to get an appointment when needed (p<0.001). The INT group experienced more benefit of the consultations within group (p<0.04) and compared with CON (p=0.06). Similarly the INT group reported having fewer unnecessary visits (p<0.005) and being more involved in the content of the consultations compared to CON (p<0.01). Overall patient satisfaction was high in both groups at baseline and at 2 years with no change from baseline to 2 years between groups (p=0.17). The number of visits in the outpatient clinic during the 2 year study period were significantly lower in the INT-group (median 4 [IQR 3;6]) compared to CON (6 [5;8]) (p<0.001) covering visits both at physicians, nurses, and dieticians. Concurrently, there was an increase in the number of telephone contacts (INT: 2 [1;4] /CON: 1 [0;3], p<0.001). Mean HbA1c (mmol/mol) was unchanged within and between groups (INT: 59.7/60.5 (2y); CON: 59.7/59.3), p>0.5. Blood pressure, LDL-cholesterol, and albumin-creatinine-ratio likewise remained equal between groups.
Conclusion: The on-demand structure resulted in high and maintained or improved patient reported experience measures and no decline of in the quality of clinical diabetes care. The total use of outpatient clinic resources was reduced. Implementation of such a concept will potentially save resources that can be relocated to patient groups with special needs.
Effects of liraglutide and semaglutide on stroke subtypes in patients with type 2 diabetes: a post hoc analysis of the LEADER, SUSTAIN 6 and PIONEER 6 trials
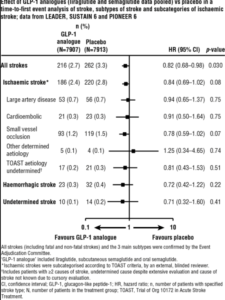
Strain WD, presented a study at the 56th EASD Annual Meeting conducted virtually to report the effect of liraglutide and semaglutide on stroke and its subtypes based on pooled data from LEADER, SUSTAIN 6 and PIONEER 6. Diabetes is an independent risk factor for stroke, with approximately a two-fold excess risk in people with vs those without diabetes. Accumulating evidence suggests glucagon-like peptide-1 (GLP-1) analogues (including liraglutide and semaglutide) may reduce the risk of stroke in patients with type 2 diabetes (T2D). LEADER, SUSTAIN 6 and PIONEER 6 were global randomised cardiovascular (CV) outcomes trials of liraglutide, subcutaneous semaglutide and oral semaglutide, respectively, in patients with T2D at high CV risk. In this post hoc analysis, the effect of these GLP-1 analogue treatments (pooled) on time to first occurrence of all strokes and subtypes of stroke. Ischaemic stroke was sub-categorised according to the TOAST classification, based on aetiology by an external blinded reviewer. A Cox proportional hazards model stratified by trial with pooled treatment as a factor was used to examine treatment effects. The results observed were: across the three trials, 216/7907 (2.7%) patients in the GLP-1 analogue group and 262/7913 (3.3%) in the placebo group had a stroke. The risk of first occurrence of all strokes was significantly reduced in the GLP-1analogue vs placebo group (HR 0.82, 95% CI 0.68-0.98; p =0.030). Treatment effects were consistent across stroke subtypes: ischaemic (HR 0.84, 95% CI 0.69-1.02; p =0.08), haemorrhagic (HR 0.72, 95% CI 0.42-1.22; p =0.22) and undetermined (HR 0.71, 95% CI 0.32-1.60; p =0.41;). Across TOAST subcategories, there was a trend that GLP-1 analogue treatment had the greatest benefit vs placebo in small vessel occlusion strokes compared with large artery disease or cardioembolic strokes; however, no statistically significant effects were found in any subcategory.
Conclusion: In this post hoc analysis of the LEADER, SUSTAIN 6 and PIONEER 6 trials, GLP-1 analogue treatment reduced the risk of stroke in patients with T2D and high CV risk, with an indication using TOAST criteria of the strongest effect on stroke caused by small vessel occlusion.