REALITY – A trial of transfusion strategies for myocardial infarction and anemia
Steg PG presented a live session on REALITY – A Trial of Transfusion Strategies for Myocardial Infarction and Anemia today at the ESC Congress 2020: The Digital Experience. The objective of the trial was to assess the safety and efficacy of a restrictive versus liberal red blood cell (RBC) transfusion strategy among patients with acute myocardial infarction (AMI) and anemia. Patients with AMI and hemoglobin (Hb) ≤8 to ≤10 g/dl during admission were randomized in a 1:1 fashion to either a liberal (for Hb ≤10 g/dl, goal Hb >11 g/dl) (n = 342) or a restrictive (for Hb ≤8 g/dl, target Hb 8-10 g/dl) (n = 324) RBC transfusion strategy. The strategies should be maintained until discharge from hospital or for 30 days, whichever comes first: total number of enrollees: 666, duration of follow-up: 30 days, mean patient age: 77 years, percentage female: 43%. Patients were randomly allocated to either a restrictive transfusion strategy or a liberal transfusion strategy and were followed-up for 30 days. The primary outcome, all-cause death, reinfarction, stroke, and emergency revascularization prompted by ischemia for restrictive vs. liberal transfusion strategy, was 11.0% vs. 14.0% (hazard ratio 0.77, 95% confidence interval 0.50-1.18, p < 0.05 for noninferiority, p = 0.22 for superiority). All-cause mortality: 5.6% vs. 7.7% (p > 0.05); recurrent MI: 2.1% vs. 3.1%; emergency revascularization: 1.5% vs. 1.9%. The secondary outcomes for restrictive vs. liberal transfusion strategy were: Acute renal failure: 9.7% vs. 7.1% (p = 0.24); infection: 0% vs. 1.5% (p = 0.03); acute lung injury: 0.3% vs. 2.2% (p = 0.03); length of stay: 7.0 vs. 7.0 days (p = 0.84); total 30-day hospital costs: €11,051 vs. €12,572 (p = 0.1)
Conclusion: The results of this trial indicate that a restrictive RBC transfusion strategy is non-inferior to a more liberal strategy. In addition, infections and acute lung injury were higher with a more liberal strategy. Total blood utilization and costs were both lower with the restrictive strategy; this strategy was considered cost-dominant.
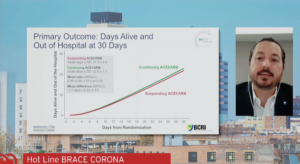
BRACE CORONA: Continuing vs. suspending ACE Inhibitors and ARBs in COVID-19
Lopes R, presented a live session on BRACE CORONA: Continuing vs. Suspending ACE Inhibitors and ARBs in COVID-19 today at the ESC Congress 2020: The Digital Experience. The goal of the trial was to evaluate suspending ACE inhibitors/ARB vs. continuing ACE inhibitors/ARB among patients hospitalized with coronavirus disease 2019 (COVID-19) infection. Patients who were taking ACE inhibitors/ARB medications chronically and were hospitalised with a confirmed diagnosis of COVID-19 were included. The primary outcome, number of days alive and out of the hospital through 30 days, was 21.9 in the suspending ACEI/ARB group compared with 22.9 in the continuing ACEI/ARB group (p = 0.09). The average ratio of days alive and out of hospital between the suspending and continuing groups was 0.95 (p=0.09). The average difference between groups was -1.1 days. The proportion of patients alive and out of hospital by the end of 30 days in the suspending ACE inhibitor/ARB group was 91.8% versus 95% in the continuing group. The secondary outcomes observed were: all-cause death at 30 days: 2.7% in the suspending ACEI/ARB group compared with 2.8% in the continuing ACEI/ARB group (p = 0.95)
Conclusion: The BRACE CORONA trial data concluded that among patients hospitalized with COVID-19 infection and receiving chronic ACEI/ARB, suspending ACEI/ARB was not beneficial. Suspending ACEI/ARB compared with continuing them did not improve the days alive and out of the hospital.
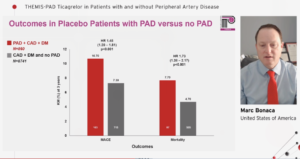
THEMIS-PAD: Ticagrelor in patients with and without Peripheral Artery Disease
Bonaca M, presented a session on THEMIS-PAD trial findings at the ESC Congress 2020: The Digital Experience. The researchers examined data from the 19,220 patients (50+ years of age) with stable CAD and T2D and without a previous myocardial infarction or stroke randomly assigned to ticagrelor plus aspirin or placebo plus aspirin, to characterize the limb events in the group overall and by the presence of PAD, including: acute limb ischemia (ALI); major amputation of vascular etiology; peripheral revascularization (urgent, elective); and overall limb ischemia outcomes defined as composite of the individual events. They also evaluated the efficacy of adding ticagrelor to aspirin to reduce limb ischemic events and whether this effect was similar in patients with and without PAD. The median age of the 1,687 patients with PAD at baseline was 68 years and 27% were women; their median duration of T2D was 12 years, 41% had complications from diabetes and 15% were current smokers. Results showed in patients on placebo, at three years, those with PAD (n=860) had a higher risk of events than those without PAD (n=8,741): limb ischemic events, 9.5% vs. 0.80% (hazard ratio [HR], 10.67); peripheral revascularization, 8.90% vs. 0.80% (HR, 10.54); major amputation of vascular etiology, 0.70% vs. 0.10% (HR, 9.96); and ALI, 0.60% vs. 0.01% (HR, 5.61). In the overall THEMIS population of 19,220 patients, there were 171 leg ischemic events in the placebo group (1.59%) and 131 limb ischemic events in the ticagrelor group (1.30%; HR, 0.77). Broken down by type of event, peripheral revascularization occurred in 1.51% vs. 1.23% (HR, 079); ALI in 0.16% vs. 0.04% (HR, 0.24); and major amputation in 0.12% vs. 0.10% (HR, 0.63). There were more elective than nonelective peripheral revascularizations. In the patients who had PAD at baseline, there were more limb events in the placebo than the ticagrelor group (9.50% vs. 7.60%, respectively; HR, 0.80). In those who did not have PAD at baseline, the rate of events was 0.80% and 0.70%, respectively (HR, 0.76).
Conclusion: The very high risk of limb events in patients with PAD, on top of CAD and T2D, and reductions with ticagrelor of about 50% for major adverse limb events and 20% for peripheral revascularization suggests long-term benefit with the drug for preventing cardiovascular and limb events.
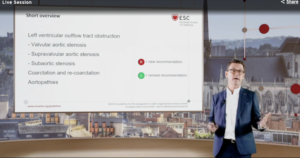
2020 ESC Guidelines on Adult Congenital Heart Disease
The 2020 ESC guidelines on Adult Congenital Heart Disease was presented today at the ESC Congress 2020: The digital experience. Some of the key recommendations presented were:
- For treatment of pulmonary arterial hypertension associated with congenital heart disease, it is recommended that patients with CHD and confirmed pre-capillary PH are counselled against pregnancy
- Risk assessment is recommended in all patients with PAH-CHD
- In low- and intermediate risk patients with repaired simple lesions and pre-capillary PH, initial oral combination therapy or sequential combination therapy is recommended and high risk patients should be treated with initial combination therapy including parenteral prostanoids
- A treat and repair approach may be considered in selected ASD patients and a VSD may be closed after careful evaluation if PVR is >5WU Qp:Qs is >1.5
- An AVSD is not a simple lesions and should only be repaired by a congenital cardiac surgeon
- In symptomatic patients with aortic valve disease, intervention is recommended in all symptomatic patients with severe high-gradient AS (mean gradient ≥40 mmHg)
- Aortic valve repair using the reimplantation or remodelling with aortic annuloplasty technique is recommended in young patients with Marfan syndrome or related HTAD with aortic root dilation and tricuspid aortic valves when performed by experienced surgeons
- If surgical valve replacement is the only option in patients with severe stenosis who are asymptomatic, it is indicated in the presence of one or more of the following: Objective decrease in exercise capacity; ecreasing RV function and/or progression of TR to at least moderate; RL shunting via ASD or VSD; RVSP >80 mmHg
- In systemic RV with severe TR, TV repair or replacement after Mustard/Senning is recommended before the RV has become too bad and in ccTGA, TV replacement is recommended if EF >45% as per ESC 2010 guidelines, but according to the new ESC 2020 guidelines TV replacement is recommended if EF>40%
Advances in heart failure medications: Which drugs for which patient?
The ACC/AHA guidelines created an algorithm to try to incorporate all of the standard therapy in ischemia allow us to make reasonable choices according to what was required to the patient. Traditionally RAAS inhibitor, ACEi or ARB, beta-blockers, diuretics are needed for decongestion. The Landmark championship data, demonstrated that only 1% of eligible patients with HFrEF were simultaneously treated with target dose of ACEI/ARB/ARNI, beta-blocker, and MRA therapy, and <25% of patients simultaneously received any dose of all 3 medications either RAASi, beta-blocker or MRA. This is awfully inadequate. In other therapies, the unique therapies specifically for those patients as African American, combination of HYD/ISDN either individual doses or fixed dose combination when added to ACEi, beta-blockers, there was 43% decrease in mortality as compared to placebo. This therapy was underutilized but remains a very important therapy particularly for patient with personalized care. In patients with elevated HF, there was less outcome, as consequence, the additional agent to slow heart rate was Ivabradine which inhibited hyperpolarization-activated cyclic nucleotide gated channels; it slows down depolarisation; slows heart rate. In SHIFT trial, the primary endpoint i.e. CV death or hospitalization for worsening HF was decreased in Ivabradine group as compared to placebo. In VICTORIA study, the CV death or hospitalization for HF was statistically advantaged by the treatment n-cyclic stimulator. From the HF study of JAMA, SGLT2i showed haematinic effect on heart, profound effect on kidneys. In DAPA-HF study, Dapagliflozin used for HF shows statically significant primary outcomes. The DAPA-HF marked as landmark study; in patients with or without diabetes showed substantial results means that Dapagliflozin showed benefit with glucose lowering effect and is independent of any glucose lowering effect. It is once day therapy; single dose; no need to titration. It showed no episodes of hypoglycaemia or diabetes ketoacidosis with negligible incidence of amputations. NNT was 21 and benefits were seen even with those with >75.
Conclusion: The foundation therapies in HFrEF to reduce mortality were ARNI, ACEi or ARB, MRA, Beta-blocker and Dapagliflozin. There is an opportunity for personalised therapy which has profoundly change the natural history of reducing ejection fraction in HF, particularly by tailoring therapies to specific patients.

Remote heart failure management using a multiparameter implantable cardioverter-defibrillator alert: The multicentric RE-HEART registry
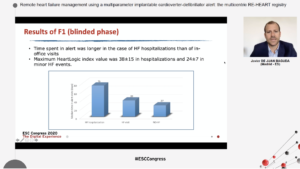
Baguda presented a session on remote heart failure management using a multiparameter implantable cardioverter-defibrillator alert, from multicentric RE-HEART registry at the ESC Congress 2020: The digital experience. The HeartLogic algorithm combines several implantable cardioverter-defibrillator (ICD)-based sensors into an index for prediction of impending heart failure (HF) decompensation. The investigators remotely moitored patients with ICD and cardiac resynchronization therapy ICD at 13 Spanish centers, to analyse the association between clinical events and HeartLogic alerts and describe the use of the algorithm for the remote management of HF. A total of 215 patients (67±13 years old, 77% male, 53% with ischemic cardiomyopathy) with ICD (19%) or CRT-D (81%) were enrolled. They observed that: HeartLogic index crossed the threshold value (set by default to 16) 34 times in 20 patients. HeartLogic alerts were associated with 6 HF hospitalizations and 5 unplanned in-office visits for HF. The rate of unexplained alerts was 0.25 alert-patient/year. The median time spent in alert was longer in the case of HF hospitalizations than of in-office visits (75 [min-max: 30–155] days versus 39 [min-max: 5–105] days). The maximum HeartLogic index value was 38±15 in the case of hospitalizations and 24±7 in that of minor HF events. After HeartLogic activation, 40 alerts were reported in 26 patients. 27 (68%) alerts were associated with multiple HF or non-HF related conditions or changes in prescribed HF therapy. The rate of unexplained alerts not followed by any clinical action was 0.13 alert-patient/year. These alerts were managed remotely (device data review and phone contact), except for one alert that generated an unscheduled in-office visit.
Conclusion: HeartLogic index was repeatedly linked with HF-related clinical events. The activation of the associated alert permitted to remotely detect relevant clinical conditions and to apply clinical actions.
Positive effect of dapagliflozin on left ventricular longitudinal function for type 2 diabetic mellitus patients with chronic heart failure
Type 2 diabetes mellitus (T2DM) is viewed to be an independent predictor of mortality, and also a contributor to the advancement of heart failure (HF) with reduced ejection fraction (HFrEF) and with preserved ejection fraction (HFpEF). Left ventricular (LV) longitudinal myocardial dysfunction has been recognized even in T2DM patients with preserved LV ejection fraction (LVEF), as examined in terms of lower global longitudinal strain (GLS) and should be considered the first marker of a preclinical form of DM-related cardiac dysfunction. Sodium glucose cotransporter type 2 (SGLT2) inhibitors exemplifies a new class of anti-hyperglycemic agents for T2DM, however the impact of SGLT2 inhibitors on LV longitudinal myocardial function remains unknown in T2DM patients with HF. Tanaka H, presented an ePoster ESC Congress 2020: The digital experience which analysed this impact, as well as the correlation of LV longitudinal myocardial function with LV diastolic function following administration of SGLT2 inhibitor in T2DM patients with stable HF, also data from the previous prospective multicenter study was analysed, in which the impact of SGLT2 inhibitor on LV diastolic functional parameters of T2DM patients with stable HF was investigated at five institutions in Japan.
Patients who had been consuming at least one antidiabetic drugs besides SGLT2 inhibitors began taking 5 mg/day of Dapagliflozin. Echocardiography was executed at baseline and 6 months after administration of Dapagliflozin. LV diastolic function was described as the ratio of mitral inflow E to mitral e’ annular velocities (E/e’). LV longitudinal myocardial function was examined as GLS based on the current guidelines. Dapagliflozin showed substantial reduction in E/e′ from 9.3 to 8.5 cm/s 6 months (p=0.020) as previously described, while substantial enhancement in GLS from 15.5±3.5% to 16.9±4.1% (p<0.01) 6 months. In addition, HFpEF patients exhibited more significant improvement of GLS from 17.0±1.9% to 18.7±2.0% (p<0.001), than HFrEF patients from 11.3±3.8% to 11.8±4.6% (p=0.13). It was notable that the change in GLS was the only independent determinant parameter for the change in E/e’ after administration of Dapagliflozin in multiple regression analysis.
Conclusion: Dapagliflozin was found to be correlated with enhancement of LV longitudinal myocardial function, which led to additional enhancement of LV diastolic function of T2DM patients with stable HF. Thus, GLS-guided treatment showed enhanced management of T2DM patients with stable HF.
Natriuretic effect of 2 weeks of dapagliflozin treatment in patients with type 2 diabetes and preserved kidney function: Results of the DAPASALT trial
Sodium glucose co-transporter 2 (SGLT2) inhibitors decrease the risk for heart failure hospitalization, prospectively by enhancing sodium excretion, osmotic diuresis and plasma volume contraction, caused more beneficial systemic hemodynamic function. But, this hypothesis has never been formally analysed as no studies have evalauted cumulative sodium excretion with SGLT2 inhibition in standardized sodium intake.
Heerspink H, presented an ePoster at ESC Congress 2020: The digital experience which analysed the acute impacts (average day 2-4), impacts at steady state (average day 12-14) and impacts in three days wash-out of Dapagliflozin on sodium balance and blood pressure in patients with type 2 diabetes mellitus (T2D) with preserved kidney function, who were acquiring a standardized sodium intake (150 mmol/day) in a mechanistic open label study. Primary outcome estimate was 24-hr sodium excretion in the acute phase. Secondary outcomes were 24-hr glucose excretion and 24-hr blood pressure at each time period and sodium excretion at steady state and in follow-up.
17 patients with T2D were enlisted (64.7% male, mean ± SD age 64.24 ± 7.33 years, weight 99.54 ± 17.36 kg, eGFR 94.53 ± 10.10 mL/min/1.73m2, HbA1c 7.20 ± 0.63%). Average sodium excretion at baseline was 147 ± 32 mmol/24 hr, which did not substantially change in therapy (Change at Day 2-4 [95% CI]: -5.21 [19.54, 9.12] mmol/24 hr; Change at Day 12-14 [95% CI]: 3.69 [-24.82, 32.20] mmol/24 hr). But, sodium excretion was decreased after washout as compared to end of therapy (Change at Day 15-17 [95% CI]: -16.72 [-34.11, 0.66] mmol/24 hr). Glucose excretion was substantially improved all over the study. Systolic blood pressure was 127.0 ± 10.3 mmHg at baseline and substantially decreased at Day 3 [95% CI]: -5.27 [-8.55, -1.99] mmHg and Day 14 [95% CI]: -7.10 [-10.04, -4.16] mmHg as compared to baseline and remained lower after washout.
Conclusion: This study shows that, the SGLT-2 inhibitor Dapagliflozin acutely decreases blood pressure without changing sodium excretion in a standardized sodium intake, signifying possible direct vascular impacts independent of sodium balance.
Effect of empagliflozin versus placebo on body composition in patients with acute myocardial infarction and type 2 diabetes mellitus: Subgroup analysis of the EMBODY trial
Prevention of heart failure is one of the most significant challenges following acute myocardial infarction (AMI). The development of heart failure is closely correlated with fluid balance which can be analysed with the measurement of body composition such as total body water (TBW), extracellular water (ECW), and intracellular water (ICW). Hoshika Y, presented an ePoster of subgroup analysis of the EMBODY trial at ESC Congress 2020: The digital experience which evaluated whether sodium–glucose cotransporter 2 (SGLT2) inhibitor influences fluid balance and improves heart failure in patients following AMI.
In Japan, the EMBODY trial was a potential, multicenter, randomized, double-blind, placebo-controlled trial in patients with AMI and type 2 diabetes. A total of 105 patients were randomized (1:1) to acquire once-daily 10 mg Empagliflozin, an SGLT2 inhibitor or placebo 2 weeks following the onset of AMI. In this subanalysis, the time-course of body composition was investigated which is estimated with a bioelectrical impedance analyzer “InBody®”. The primary endpoints were changes in every particular parameter of body composition at week 0, 4, 12, and 24. Secondary endpoints were changes in blood pressure (BP), body weight and N-terminal pro b-type natriuretic peptide (NT-proBNP).
Altogether, 55 patients were involved in the full analysis set (67.2±10.0 years, male 78.2%, and n = 30 in Empagliflozin group and 25 in placebo group). Baseline characteristics were not substantially different among the two groups. The change in TBW between at baseline and 24 weeks was -0.44 L (p = 0.19) in the Empagliflozin group and +1.14 L (p = 0.0002) in the placebo group, adjusted difference -1.58 L, 95 % confidence interval (CI) -2.46 to -0.70 L (p = 0.0006). The Empagliflozin group exhibited substantial reduction in the body weight, ECW, ICW and systolic BP as compared to the placebo group (-2.2 kg vs, +0.01 kg, p = 0.004, -0.21 L vs, +0.40 L, p = 0.001, -0.23 L vs, +0.74 L, p = 0.0007, and -11.0 mmHg vs, +5.0 mmHg, p < 0.0001, respectively). On the other hand, NT-Pro BNP levels were substantially reduced in the Empagliflozin group and placebo group (1028.7 pg/mL to 370.3 pg/ml, p = 0.0001 and 1270.6 pg/mL to 673.7 pg/ml, p = 0.006, respectively). The change in TBW and ICW for the Empagliflozin group, systolic BP was recognised as a substantial factor in the multiple regression analysis (p = 0.001, and 0.003, respectively). The Empagliflozin group exhibited substantial reduction in body weight, TBW, ECW and ICW than the placebo group, however not below BMI 25 kg/m² group in stratified analysis of BMI 25 kg/m² or more.
Conclusion: Empagliflozin showed reduction in not only body weight, but also in TBW, ECW and ICW. Interestingly, this propensity was exceptional at BMI 25 or more. This study recommended that early SGLT2 inhibitor intake might be efficacious to decrease body weight and TBW in obese patients with AMI and DM.
Effect of empagliflozin as add-on therapy on transtubular potassium concentration gradient in patients with type 2 diabetes hospitalized for acute decompensated heart failure
The transtubular potassium concentration gradient (TTKG) has been described to be a marker of renal aldosterone bioactivity, and has been exhibited to be a surrogate of arterial underfilling in patients with acute decompensated heart failure (ADHF). Furthermore, high TTKG at discharge has been exhibited to be correlated with poor prognosis in ADHF patients. Empagliflozin, one of the sodium glucose cotransporter 2 inhibitors, exhibited reduction in the risk of cardiovascular mortality in patients with type 2 diabetes mellitus (T2D) and cardiovascular disease. But, limited is known about the impact of Empagliflozin as add-on therapy on TTKG in T2D patients with ADHF. Thus, Tamaki S, presented an ePoster at ESC Congress 2020: The Digital Experience which explained the impact of Empagliflozin as an add-on therapy on TTKG in T2D patients with ADHF.
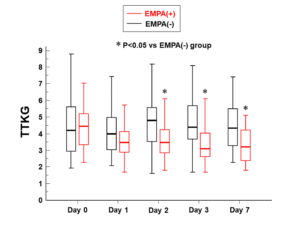
58 consecutive T2D patients admitted for ADHF were enrolled in a study. On admission, patients were randomly allocated in a 1:1 ratio to whether Empagliflozin add-on therapy (EMPA(+)) or conventional glucose-lowering therapy (EMPA(-)). All patients in EMPA(+) group acquired Empagliflozin (10 mg/day) all the time in the study period. Left ventricular ejection fraction (LVEF) was estimated at baseline with echocardiography. Body weight and crucial signs, such as blood pressure and heart rate, were estimated, and blood and urine samples were gathered at baseline and 1, 2, 3 and 7 days following randomization. The TTKG was estimated by the first morning urine samples collected on each day. TTKG was measured as per the following equation: TTKG = (Ku/Ks)×(plasma osmolality/urine osmolality), where Ku is urine potassium concentration and Ks is serum potassium concentration, as previously described. 30 patients were allocated to the EMPA(+) group, and 28 patients were allocated to the EMPA(-) group. There were no substantial baseline differences in LVEF, plasma B-type natriuretic peptide (BNP) level, body mass index, or serum creatinine level among the EMPA(+) and EMPA(-) groups. TTKG did not substantially vary among the two groups at baseline. But, seven days after randomization, EMPA(+) group showed substantially lower level of plasma BNP than EMPA(-) group (median 227 [IQR 114-381] pg/mL vs 362 [227-554] pg/mL, p=0.0294). In addition, TTKG of the EMPA(+) group was substantially lower at 2, 3 and 7 days following randomization (Figure).
Conclusion: This study indicated that Empagliflozin as add-on therapy could decreased TTKG in T2D patients with ADHF.
The effects of empagliflozin on arterial stiffness, endothelial function and ventriculoarterial coupling in type 2 diabetes mellitus: 1 year follow up
Sodium glucose cotransporters inhibitors (SGLT2i) are presently used in the therapy of patients with type 2 diabetes mellitus (T2DM) who have a high cardiovascular risk. But their impacts on arterial stiffness, endothelial function and ventriculoarterial coupling have not been reported. Thus, Ikonomidis I, presented an ePoster at ESC Congress 2020: The digital experience which analysed effects of Empagliflozin on arterial stiffness, endothelial function and ventriculoarterial coupling in T2DM at 1 year follow up. 120 patients with T2DM were recruited. Either the Empagliflozin (n=60) or insulin (n=60) were acquired by them. Following parameters were estimated at baseline and after 1 year of treatment: 1) Perfused Boundary Region (PBR 5-25μm) to analyse endothelial glycocalyx integrity via Glycocheck, 2) Pulse wave Velocity (PWVc-f), 3) central systolic blood pressure (cSBP), 4) central Pulse Pressure (cPP) via Complior, 5) the ratio PWV/GLS using echocardiography to estimate ventriculoarterial coupling (VA coupling).
The patients were matched for age, gender, smoking, hypertension and hyperlipidemia (p=NS). Both groups showed reduction in HbA1c (8.1% vs 8.2%, p=NS). The baseline measurements of aforementioned markers did not vary among the 2 groups (p=NS). PWV was associated with cSBP (r=0.4. p<0.05) and cPP (r=0.35, p<0.05) for all participants at baseline. After 1 year of treatment both groups showed substantial reduction in HbA1c. Patients treated with insulin exhibited an elevation of PWV in contrary with Empagliflogin group (11.4 ± 0.5 to 12.6 ± 0.4 vs 11.7 ±0.5 to 10.9 ±0.4, correspondingly, p<0.05). cSBP significantly decreased in Empagliflozin group (135± 10 to 129±10 vs 134±9 to 136±9 respectively, p<0.05) and cPP remained nearly steady (47±8 to 48±8 vs 49±6 to 55± 6 respectively, p<0.05) as compared to insulin group. PBR discontinued in SGLT2i group (2.20±0.2 to 1.98±0.2, p<0.05) although in insulin group, PBR varied at the same level (2.18±0.2 to 2.15±0.3, p=NS). PWV/GLS decreased in both groups however the Empagliflozin group showed more prominent reduction (-0.72±0.1 to -0.67±0.1 vs -0.72±0.1 to -0.60±0.1 respectively, p<0.05).
|
|
Insulin |
SGLT2i (Empagliflozin) |
||||
|
|
PRE |
POST |
p |
PRE |
POST |
p |
|
PWVc-f (m/s) |
11.4 ± 0.5 |
12.6 ± 0.4 |
<0.05 |
11.7 ±0.5 |
10.9 ±0.4 |
<0.05 |
|
cSBP (mm Hg) |
134±9 |
136±9 |
NS |
135± 10 |
129±10 |
<0.05 |
|
cPP (mm Hg) |
49±6 |
55± 6 |
<0.05 |
47±8 |
48±8 |
NS |
|
PBR (μm) |
2.18±0.2 |
2.15±0.3 |
NS |
2.20±0.2 |
1.98±0.2 |
<0.05 |
|
PWV/GLS |
-0.72±0.1 |
-0.67±0.1 |
NS |
-0.72±0.1 |
-0.60±0.1 |
<0.05 |
Conclusion: 1-year treatment with Empagliflozin showed enhanced markers of arterial stiffness, ventriculoarterial coupling and endothelial function, independently of glycemic control.
The association between SGLT2 inhibitors and new-onset arrhythmias: A nationwide population-based longitudinal cohort study
Clinical trials had exhibited the cardiovascular protective impact of sodium-glucose cotransporter-2 (SGLT2) inhibitors and decreased hospitalization for heart failure. However, no study has estimated the correlation among SGLT2 inhibitors and the risk of arrhythmias. Thus, Siao WUN-ZH, presented an ePoster at ESC Congress 2020: The Digital Experience which analysed the risk of new-onset arrhythmias (NOA) and all-cause mortality with the use of SGLT2 inhibitors. Taiwan’s National Health Insurance Research Database was used in a population-based cohort study. Each patient aged 20 years and older who received SGLT2 inhibitors was allocated to the SGLT2 inhibitor group, although sex-, age-, diabetes mellitus duration-, drug index date-, and propensity score-matched randomly selected patients without SGLT2 inhibitors were allocated to the non-SGLT2 inhibitor group. The study outcome was all-cause mortality and NOA.
A total of 399,810 patients with newly diagnosed type 2 diabetes mellitus (T2DM) were enlisted. For analysis, 1:1 matching propensity procedure was used to match 79,150 patients to 79,150 controls in the non-SGLT2 inhibitors group. The SGLT2 inhibitor group was correlated with a lower risk of all-cause mortality (adjusted hazard ratio [aHR] 0.547; 95% confidence interval [CI] 0.482–0.621; p = 0.0001) and NOA (aHR 0.830; 95% CI 0.751–0.916; p = 0.0002). Subgroup analysis showed that the SGLT2 inhibitor group was correlated with a lower risk of all-cause mortality in all age and extremity of the adapted Diabetes Complication Severity Index (aDCSI) subgroups. In addition, NOA and atrial fibrillation with an aDCSI score of between 1 and 2 were correlated with a lower risk in subgroups.
Conclusion: Patients with T2DM prescribed with SGLT2 inhibitors were correlated with a decreased risk of all-cause mortality and NOA as compared to those not taking SGLT2 inhibitors in real-world practice. The prospective protective impact of NOA and atrial fibrillation is remarked, particularly in individuals with T2DM and an aDCSI score of between 1 and 2.

