DECIDE-Salt, Effects of Salt Substitute and Stepwise Reduction of Salt Supply
Yangfeng Wu from the Peking University, Beijing, China presented an informative talk on the topic, “DECIDE-Salt, effects of a salt substitute and stepwise reduction of salt supply” at the European Society of Cardiology conference 2021.
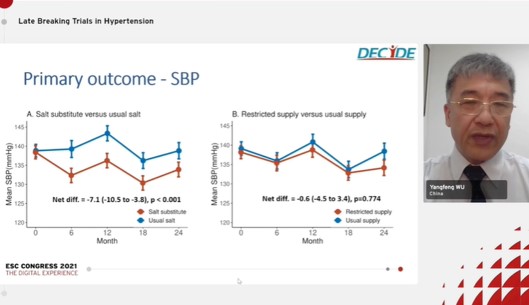
Yangfeng Wu showed the results of the DECIDE-Salt Trial whose primary objective was to study the impact of salt supply on blood pressure in residents in senior residential facilities. The salt substitute has been proved effective in lowering blood pressure but concerns with its safety, hyperkalemia is held widely. In the current multicentre 2-2 factorial, cluster-randomized and blind study, usual salt was replaced with a salt substitute in facility kitchens, and salt or salt substitute supply was reduced to facility kitchens step by step. Salt substitute comprised 62.5% NaCl, 25% KCl, 12.5% dried food ingredient flavorings, and traces of amino acids while usual salt consisted of over 99% NaCl. The kitchen-based stepwise salt supply control program was planned. The primary outcome of the study was systolic blood pressure (SBP), analyzed among the 1612 individuals aged 55 years or over with baseline blood pressure measurements. The secondary outcomes were diastolic blood pressure (DBP), cardiovascular events, and death, analyzed primarily among 1612 eligible participants and also among all 2248 residents. Other outcomes were safety, continuous, events and dichotomous safety outcomes. The baseline characteristics were similar in all the groups; salt substitute group, usual salt group, restricted supply group, and usual supply group. Mean SBP was significantly reduced in the salt substitute group than the usual salt group whereas in the restricted supply group, mean SBP was lower than the usual salt group but, the difference was not statistically significant. The total mortality rate among participants eligible for primary outcome assessment (N=1612); hazard ratio (HR) of salt substitute vs. usual salt group was 0.84 and that of restricted supply vs. usual supply group was 1.19. The total mortality rate among all participants living in the facilities (N=2248); HR of salt substitute vs. usual salt group was 0.84 and that of restricted supply vs. usual supply group was 1.22. The incidence of hyperkalemia was highest in the salt substitute group than the usual salt group. Among 50 participants with biochemical hyperkalemia, 2 participants had serum potassium high at both 12 and 24 months, 2 died and 3 had a non-fatal stroke.
Salt substitute reduced blood pressure and cardiovascular events with fairly good safety. Although salt substitute increased the risk of biochemical hyperkalemia, there was no evidence of associated adverse clinical outcomes. The DECIDE-Salt efforts to restrict the supply of salt/salt substitute to facility kitchens were unsuccessful and therefore could not meaningfully alter sodium intake as measured by urinary sodium excretion, thus no effect on blood pressure and clinical outcomes.
Efficacy of Digital Therapeutics for Essential Hypertension (HERB-DH1 Pivotal Study)

Kazuomi Kario from Jichi Medical University-Tochigi, Japan talked about the much-needed topic in today’s time, “Efficacy of digital therapeutics for essential hypertension (HERB-DH1 pivotal study)” at the European Society of Cardiology conference 2021.
Digital therapeutics refers to an emerging branch of medicine that utilizes technology-based software algorithms or applications. The HERB system is a new interactive smartphone app designed to help users make intensive and consistent lifestyle modifications to reduce blood pressure (BP). The study was conducted in Japan to evaluate the efficacy and safety of digital therapeutics using the HERB in hypertensive patients. The study included 946 patients aged 20-65 years diagnosed with essential hypertension (24-hr systolic BP ≥130 mmHg). Out of 946, 390 eligible patients were randomized to digital therapeutics and control group. The primary outcome of the study was the change in 24-hr systolic BP (SBP) by Ambulatory blood pressure monitoring (ABPM) at 12 weeks. There was no statistical difference in the baseline characteristics between the two groups. The change in BP (ABPM 24-hr SBP, ABPM daytime SBP, ABPM night time SBP, morning home SBP, evening home SBP, office SBP) from baseline to 12 weeks was greater in the digital therapeutics group than in the control group. Individual patient responses at 12 weeks were significantly better in the digital therapeutics group than in the control group. A greater reduction in morning home SBP was noted in the digital therapeutics group. The need for hypertension medication was also lower in the digital therapeutics group. The change in body weight from baseline to 24 weeks was greater with digital therapeutics and was maintained throughout the study. The salt intake score from baseline to 24 weeks was reduced more in the digital therapeutic group and was maintained throughout the study. The study has a few limitations; enrolment of a selected group of patients with hypertension, limited on-med data, insufficient period to evaluate BP, and determination of adherence based on app engagement and implementation of app-suggested lifestyle modifications. The results of this study highlight the potential effects of digital therapeutics for non-pharmacological lifestyle modification to reduce BP in untreated patients with essential hypertension.
The International Society of Hypertension has highlighted the need for population-level initiatives to reduce the global burden of elevated BP, including diet and exercise recommendations and reducing salt intake. Digital tools such as the HERB system have the potential to contribute to these individual-level initiatives for patients with early-stage hypertension by facilitating the implantation and effectiveness of lifestyle modification messages and behaviors.
Quadruple UltrA-low-dose tReaTment for hypErTension – QUARTET
Clara Chow from the University of Sydney, Sydney, Australia gave a presentation on a very unique topic entitled, “Quadruple UltrA-low-dose tReaTment for hypErTension – QUARTET” at the European Society of Cardiology conference 2021.
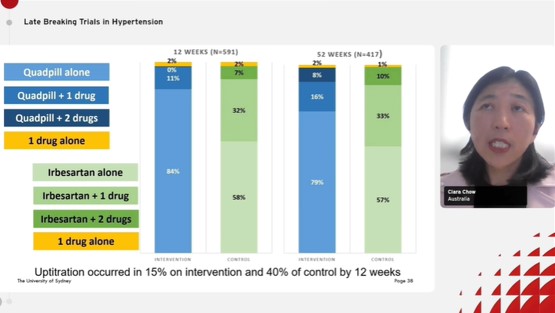
Blood pressure (BP) control is poor globally despite the availability of medicines. The major reasons behind the poor BP control are the need for multiple medications, treatment inertia, and concerns regarding adverse events. In 2017, a pilot and systematic review were carried out to study the effect of quarter dose on BP lowering. The study demonstrated that four drugs at a quarter dose were more effective than monotherapy. However, there were few reports on adverse events and no data was compared to guideline-based or usual care regimens or on long-term effects. Hence, the QUARTET study was carried out to estimate whether hypertension management started with a single pill containing quarter-standard doses of four types of BP lower medicines (Quadpill) is more effective than an approach that starts with standard-dose monotherapy. The QUARTET study was based on the hypothesis that a strategy of initial combination pill of 4 X ¼ standard doses (irbesartan 37.5 mg, amlodipine 1.25 mg, indapamide 0.625 mg, bisoprolol 2.5 mg) will lower BP more effectively than initiating standard-dose monotherapy (irbesartan 150 mg) as per common guidance. The primary outcome of the study was the change in mean automated unattended office systolic BP (SBP) at 12 weeks The secondary outcomes were the change in mean automated unattended office SBP/diastolic BP (DBP) at 52 weeks, change in mean 24-hour SBP/DBP at 12 & 52 weeks, % requiring a step up, BP control at 6,12,52 weeks and safety and tolerability. A total of 591 patients were randomized to either initial Quadpill or initial monotherapy group. Baseline characteristics were similar between the two groups. 84% and 79% of patients continue to use Quadpill alone at 12 and 52 weeks, respectively, while in the control group, 58% and 57% of patients in the control group used irbesartan alone at 12 and 52 weeks, respectively. At 12 weeks, the primary outcome of unattended office BP was lower in the initial Quadpill vs. the initial monotherapy group by 6-9 mmHg. At 12 months, a significant lowering in systolic blood pressure was noted in the Quadpill group. Despite greater up-titration at every step in the usual care group, BP control rates remained higher with Quadpill. The Quadpill group had lower daytime and nighttime BP. Tolerability was found to be equivalent in both groups. A strategy starting with the quarter-dose Quadruple combination more effectively lowered BP compared to the common approach starting with standard-dose monotherapy.
The study demonstrates the simplicity and efficacy of a Quadpill-based strategy to achieve and maintain BP control i.e. BP control achieved in a single step.
2021 ESC Guidelines on Cardiac Pacing and Cardiac Resynchronisation Therapy

Glikson M and Nielsen JC together presented updated ESC Guidelines on cardiac pacing and cardiac resynchronization therapy (CRT) at the European Society of Cardiology (ESC) Congress 2021: The Digital Experience on 29th August 2021.
Many areas have developed after all the previous guidelines were published in 2013, and new recommendations are now required in areas such as pacing following syncope, pacing after transcatheter aortic valve implantation (TAVI), pacing after heart surgery and pacing in patients with cardiomyopathy or various rare disorders. Concerning decision-making on whether a device is required, a new section provides guidance on the evaluation of patients for pacing; for example, when imaging, certain laboratory tests or genetic examinations should be executed. The section on CRT has been expanded and updated, and now incorporates several evidences for CRT in heart failure (HF), which have been changed in agreement with the ESC HF Guidelines Task Force. Furthermore, there are new recommendations for the use of CRT for prevention of pacing-induced cardiomyopathy. There is a whole new section on different pacing strategies and sites. Prof. Glikson said that pacing was at a fixed rate in the early days, but today it is much more sophisticated. The guidelines introduce novel ways to pacing the conduction system to gain more physiological pacing, including His bundle and left bundle pacing.
Attention has increased in other areas, such as how to systematically reduce procedural risk and avoid complications of cardiac pacing, and how to treat patients with pacemakers in special situations, such as when magnetic resonance imaging or irradiation are required. Guidance on device follow-up is also given, incorporating recommendations on when remote device management is appropriate.
Finally, there is a new section highlighting the requirement for patient-centred care. The guidelines highlight the significance of shared decision-making among patients and clinicians, both preoperatively and in follow-up. Topics of education are reported to aid patients make informed choices. Decisions on the type of pacemaker treatment should be based on the best available scientific proof, risk-benefit judgements of the therapy options, and the patient’s preferences and goals of care.
NATURE-PCSK9 Trial
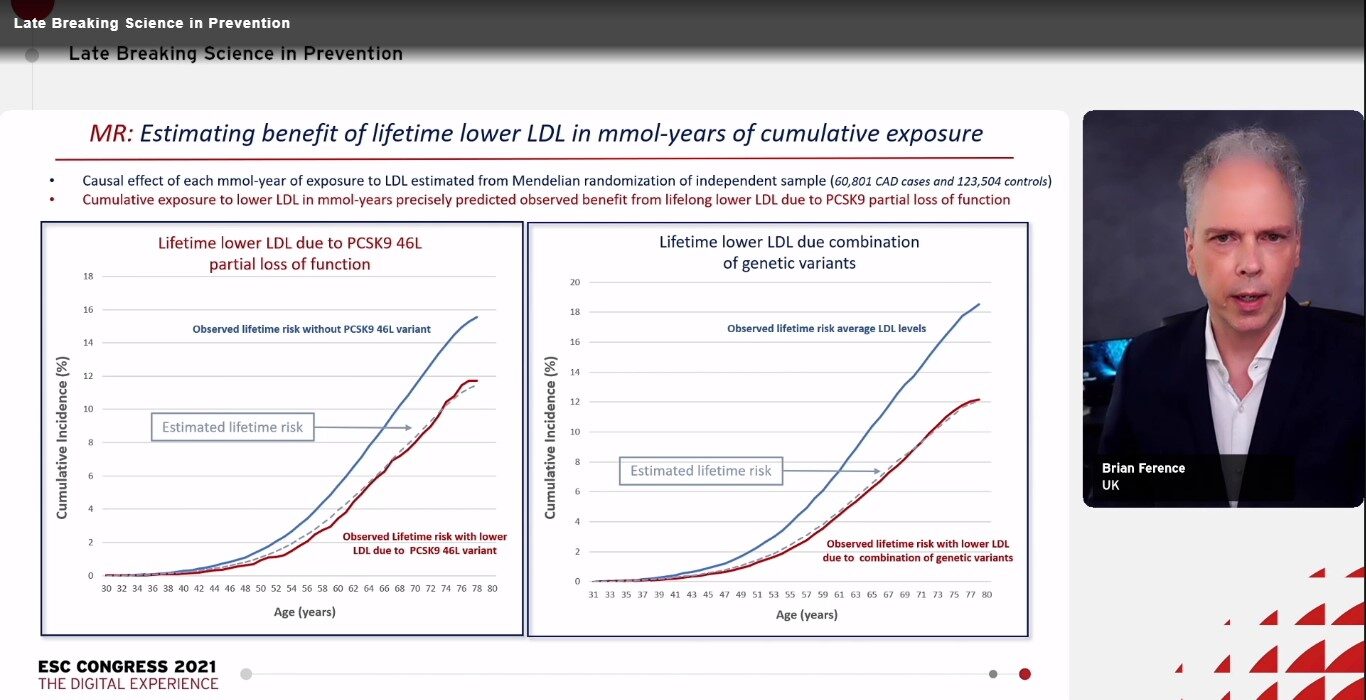
Individuals who inherit low-density lipoprotein (LDL)-lowering variants in the PCSK9 gene showed large reductions in lifetime risk of cardiovascular (CV) events. As a once-yearly dose of PCSK9 small-interfering RNA (siRNA) has been shown to decrease LDL levels by 34%,1 it was stated that a vaccine-like strategy using a PCSK9 siRNA may prospectively decrease the lifetime risk of CV events, recapitulating the phenotype of the LDL-lowering PCSK9 variants.
A 50-year randomised clinical trial to analyse the hypothesis is impractical. Ference BA, presented a Late-Breaking Science session at the European Society of Cardiology (ESC) Congress 2021: The Digital Experience on 29th August 2021 which presented a naturally randomised ‘target’ trial was designed to analyse the effects. The NATURE-PCSK9 trial assessed the clinical advantage and optimal timing of a PCSK9 siRNA vaccine-like strategy using data from the PCSK9 variants that the siRNA was designed to mimic to anticipate the expected outcome.
A total of 445,765 participants enlisted in the UK Biobank without a diagnosis of atherosclerotic CV disease, diabetes, or cancer before the age of 30 years were incorporated in the assessment. The impacts on the lifetime (up to age 80 years) risk of major coronary events caused by lowering LDL, starting at ages 30, 40, 50 or 60 years, was measured using expressing the causal effect of LDL-lowering PCSK9 genetic variants in mmol-years of LDL. The primary outcome was age at first occurrence of a major coronary events (fatal or non-fatal myocardial infarction, or coronary revascularisation). The key secondary outcome was age at first occurrence of a major CV event (major coronary events or ischaemic stroke).
Baseline LDL level was 3.5 mmol/L (136 mg/dL) and 23,032 of the participants showed a first major coronary event before the age of 80 years. Compared with usual care, it was measured that a sustained annual reduction of 34% in LDL because of siRNA-induced inhibition of PCSK9 would caused significant decrease in the lifetime risk of major coronary events, with a hazard ratio [HR] of 0.48 when LDL lowering began at 30 years of age, a HR of 0.54 for LDL lowering beginning at 40 years, a HR of 0.63 for LDL lowering from 50 years and a HR of 0.73 for LDL lowering from 60 years. Similar step-wise increased decrease in the lifetime risk of major CV events and the individual components of the composite outcomes were noticed with each decade of earlier initiation of LDL-lowering treatment. Extended PCSK9 inhibition-mediated LDL lowering did not increase the lifetime risk of type 2 diabetes or cancer.
The findings exhibited that a vaccine-like strategy to reduce LDL using a once-yearly dose of a PCSK9 siRNA can significantly decrease the lifetime risk of CV events, the impact being higher prior the LDL-lowering siRNA treatment is initiated.
A Prospective Evaluation of COVID-19 Associated Coagulopathy with Acute Coronary Syndrome (ACS)
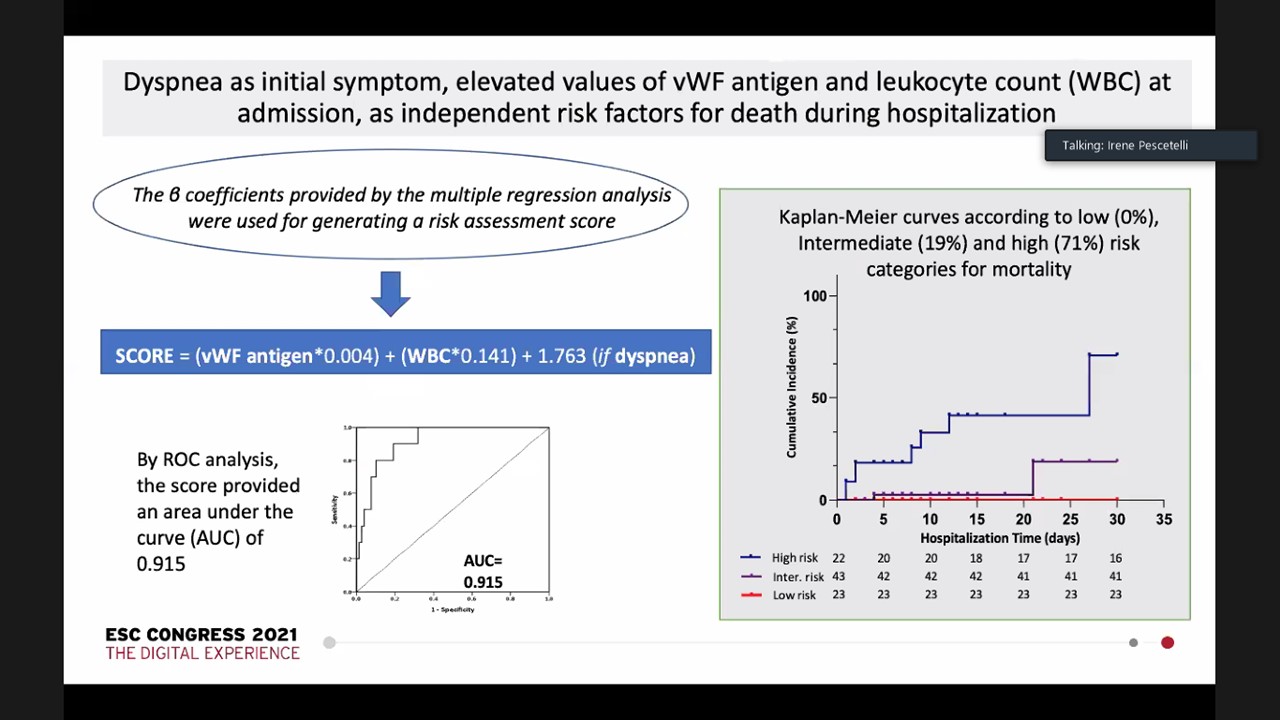
Hospitalised COVID-19 pneumonia patients are attributed by the incidence of a hypercoagulable state correlated to a high risk of thromboembolic occurrences. The main laboratory results of this coagulopathy incorporate D-dimer increase, mild thrombocytopenia, prolonged PT, and increase endothelial activation biomarkers (vWF, thrombomodulin). No data are accessible regarding coagulation profile in patients presenting with an acute coronary syndrome (ACS) combined with SARS-CoV-2 infection. Pescetelli I, presented a session at the European Society of Cardiology (ESC) Congress 2021: The Digital Experience on 29th August 2021 which analysed the contribute of concomitant SARS-CoV-2 infection to the haemostatic system derangement (i.e., from endothelial cell activation to fibrinolytic phase) noticed in patients with ACS . Moreover, the role of haemostatic biomarkers (HB) for in-hospital mortality risk prediction was also investigated.
The study enrolled the succeeding patients admitted to the hospital for ACS at peak intensity of local pandemia. At admission, all patients underwent routine blood tests with blood count, serum biochemical tests and an extensive coagulation profiling. Data were gathered following coronary angiography and percutaneous coronary intervention (PCI). In-hospital major adverse cardio and cerebrovascular events –MACCEs- (total and cardiovascular death, stroke, systemic or pulmonary embolism, re-MI and bleedings) are outlined. Results. A total of 99 (76M/23F) successive patients with a median age of 66.7 (±12.1) were enlisted. 24 patients were SARS-CoV-2 positive and 75 negative as per the nasal swab. The 2 groups with similar age, sex and cardiovascular risk factors, substantially varied in presenting symptoms (p<.001) and radiological signs of pneumonia (p<.0001). At admission, no difference was seen in routine laboratory values among groups. HB examination exhibited significantly higher values of D-dimer, vWF antigen, vWF activity and vWF;RiCof, t-PA and PAI-1 and lower levels of ADAMTS-13 in the positive group. Additionally, in ACS patients, both STEMI and NSTEMI patients, positive for SARS-CoV-2, showed substantially greater plasma values of all the HB than the respective negative counterparts, with SARS-CoV-2 positive STEMI patients with the highest values. When executed, PCI finished more commonly with a final TIMI flow <3 (p=.004) in positive patients. SARS-Co-V2 positive group showed higher prevalence(p<.0001) with 24% in-hospital rate of MACCEs (24/99 patients). Cardiovascular mortality reported the majority of deaths (8/10; p=.019). At multivariable examination, dyspnoea was recognised at presentation with vWF antigen and leukocyte values as independent risk components for in-hospital death.
An additional HB asset derangement with active endothelial cell activation happens in patients with ACS integrated with SARS-Cov-2 infection which negatively affect the result, nevertheless of the invasive therapy.
Atrial Fibrillation Self-screening, Management and Guideline Recommended Therapy (AF SELF SMART): Improving AF Screening in General Practice by Utilising Self-Screening Stations in GP Waiting Rooms
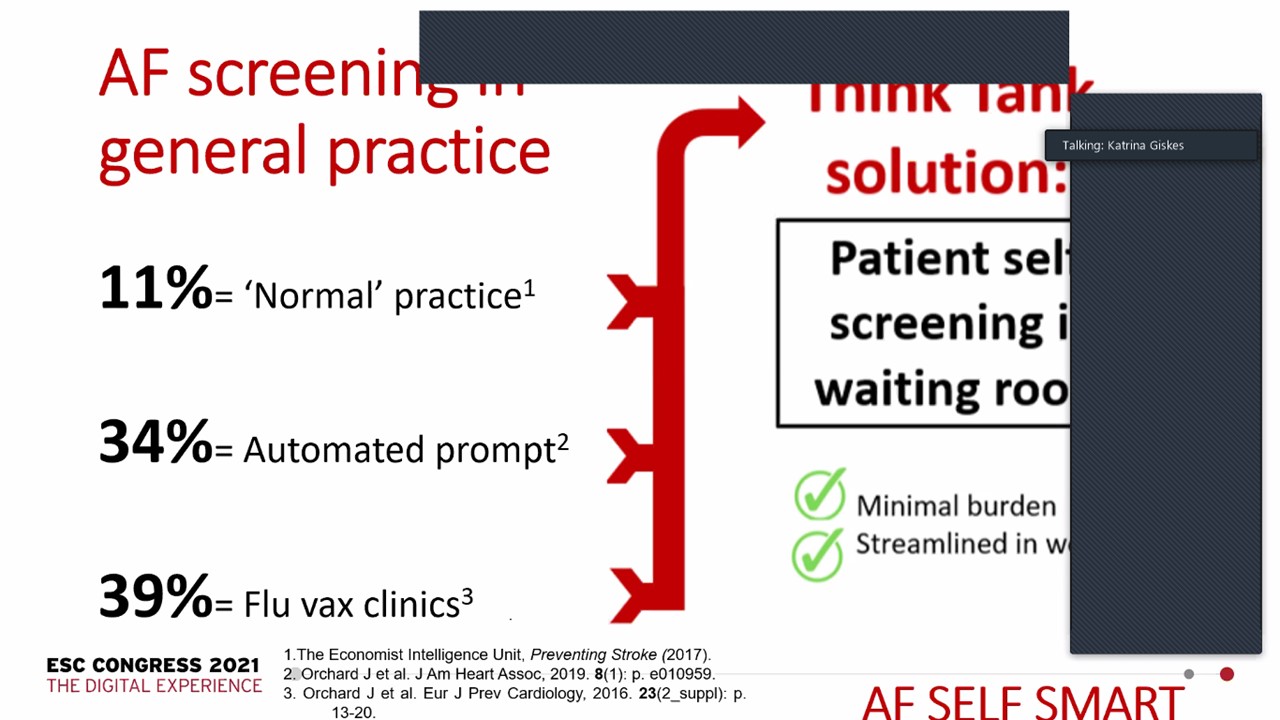
Giskes K, presented a session at the European Society of Cardiology (ESC) Congress 2021: The Digital Experience on 29th August 2021 which conducted to increase the proportion of patients examined for atrial fibrillation (AF) in general practice by executing AF self-screening stations in waiting rooms.
the study group developed and analysed an AF self-screening station by a single-lead ECG and app with automated ECG examination accompanying with customised software that fully combines the self-screening station with GP medical software and the practice workflow. The system:
- Automatically recognizes eligible patients (aged ≥65 years, no AF diagnosis) from the practice appointment diary, and sends an SMS concerning self-screening earlier to their appointment
- Automatically generates individualised patient QR codes, which yielded to the patient by the receptionist
- The patient later scans QR code and self-screens at the station in the waiting room
- The ECG and finding are automatically imported into the patient’s record before the GP consultation.
3 general practices were enrolled in the study. Each practice participated for approximately 3-months. In this period, 825 patients with mean age 74.2 years and 45% male completed AF self-screening.
The evaluation showed that the mean proportion screened in practices was 52% (range 38-65%) when expressed as a proportion of the actual eligible patients attending the practice in the study period. 37/825 patients (4.5%) with mean age 77.2 years 43% male exhibited ‘Possible AF’ by device algorithm.
An AF self-screening station assigned in GP waiting rooms that are combined with the practice software and workflow may accomplish greater screening rates for AF in general practice as compared to standard practice and thus contribute to higher decrease in stroke.
Derivation and Validation of a Pretest Probability Score for Deep Vein Thrombosis Before Surgery
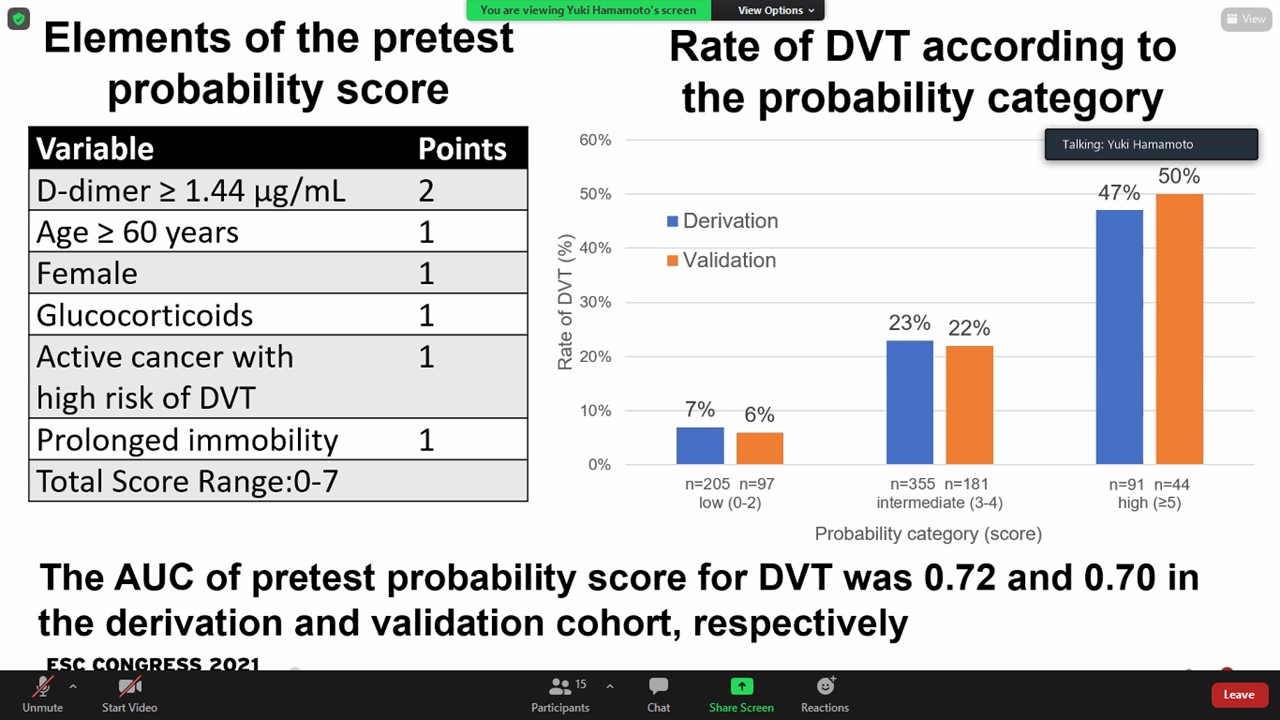
Venous thromboembolism shows a vital perioperative complication and causes morbidity and mortality. It is significant to forecast deep vein thrombosis (DVT) before surgery under general anaesthesia. Hamamoto Y, presented a session at the European Society of Cardiology (ESC) Congress 2021: The Digital Experience on 29th August 2021 which developed a pretest probability score for forecasting DVT with perioperative clinical and laboratory factors.
Total 7435 patients were enrolled for surgery under general anaesthesia in 2017 and 2018. 1313 patients were executed whole leg ultrasonography suspected DVT by cutoff point of d-dimer ≧1μg/ml. Patients of age < 18 years, ongoing anticoagulant treatment, other thrombosis, protein C deficiency, disseminated intravascular coagulation, central venous catheter, pregnancy and aneurysm were excluded. 971 patients were enlisted and divided into the derivation group or the validation group. A derivation group of 651 patients showed correlation of DVT with multiple variables. The score validated in an independent group of 322 patients from the same study. We also executed a validation of this model in an independent group of patients obtained from the same observational study.
6 clinical and 1 laboratory parameters were found that forecasted DVT in patient’s prior surgery. The prediction rule for DVT allocated 2 points for D-dimer more than 1.44 μg/ml and 1 point for age ≥60 years, female, ongoing steroid, active cancer with high risk of DVT, prolong immobility and antipsychotic drug. Area under the curve was 0.73 and 0.70 in derivation and validation groups, respectively. New preoperative risk model with these characteristics stratified patients into 3 individual classes corresponding to the risk of DVT. Rates of DVT were 6% and 7% in low-risk (score 0-2), 22% and 21% in intermediate-risk (score 3-4), and 49% and 47% in high-risk (score ≥ 5) category in the derivation and validation groups, respectively. Rates of fresh DVT were 1% and 3% in low-risk, 10% and 9% in intermediate-risk, and 33% and 19% in high-risk category.
This score stratifies perioperative DVT risk and may efficaciously diagnose DVT. The results should be contemplated with the additional prospective research.
Assessment of Vascular Endothelial Function in COVID-19 Patients
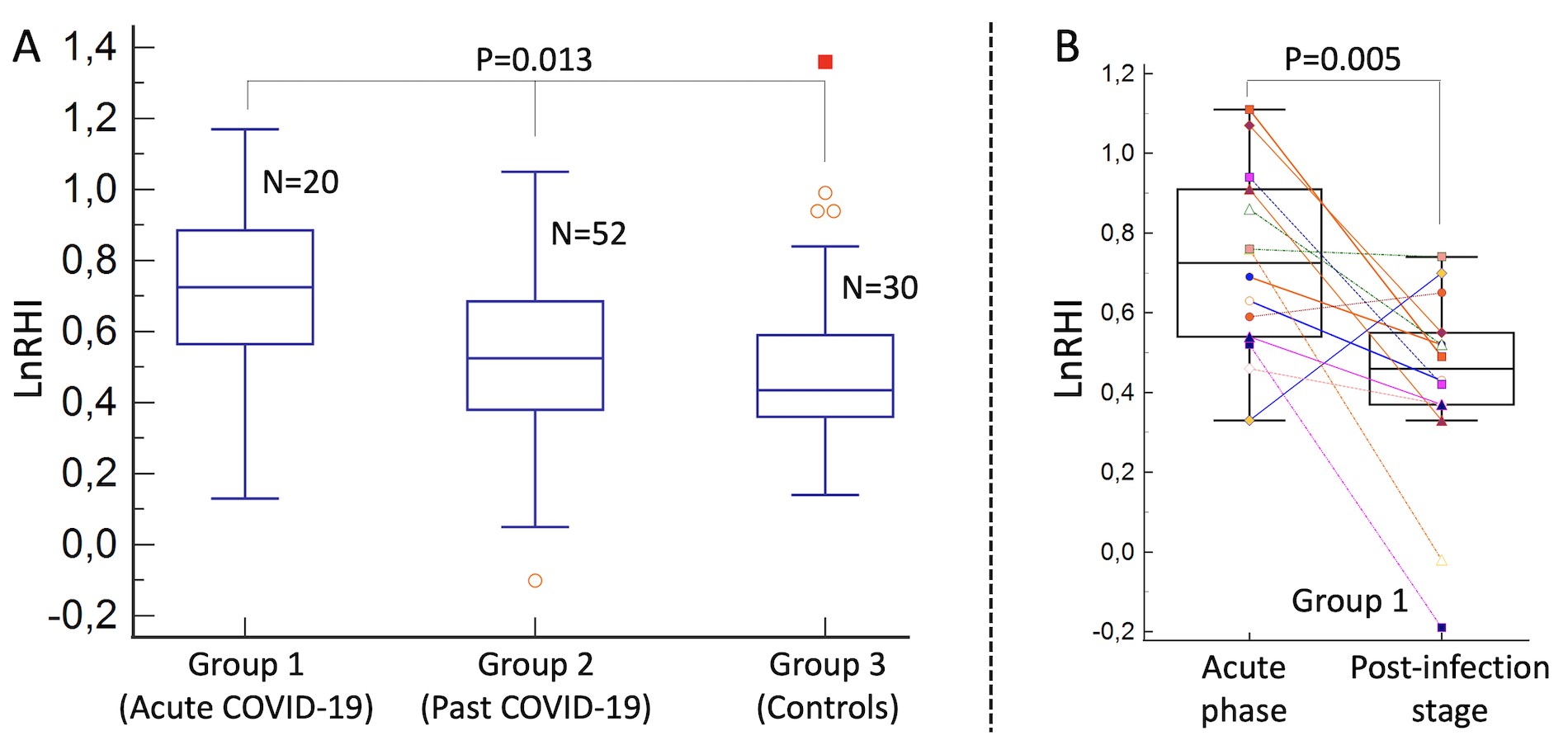
Severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) uses angiotensin-converting enzyme 2 (ACE2) receptor as a way to enter the host. High density of ACE2 receptor in vascular endothelial cells may investigate why vascular complications correlated to endothelial dysfunction happen in COVID-19. But in vivo evaluation of vascular endothelial function in COVID-19 has not been outlined.
Renteria HM, presented a session at the European Society of Cardiology (ESC) Congress 2021: The Digital Experience on 29th August 2021 which assessed the vascular endothelial function and its temporal changes in COVID-19 patients.
The prospective blinded study in which systemic endothelial function was examined by plethysmography-derived peripheral arterial tonometry (PAT). The reactive hyperemia index (LnRHI), a measure of endothelium-mediated hyperaemia, and the augmentation index, a measure of arterial vascular stiffness, were estimated in 102 individuals over 3 study groups by PAT: group 1 (active infection), represented by 20 patients hospitalised because of acute COVID-19; group 2 (past infection), constituted by 52 patients who had recovered from COVID-19; and group 3 (controls), represented by 30 healthcare workers not infected with SARS-CoV-2. Furthermore, in group 1, PAT analysis was repeated in 14 patients several weeks following recovery from acute COVID-19. PAT studies were examined at a blinded fashion with respect to the allocated study group.
The acute COVID-19 patients had lower resting PAT amplitude than the other groups (ratio of arterial tone signal between hyperemia to resting condition was 1.5 [interquartile range, 1.1] in group 1, 1.3 [0.3] in group 2 and 1.2 [0.3] in group 3, p=0.041). On the contradictory, no substantial differences between groups were found with respect to the hyperemic PAT amplitude (867.9 [486.1] in group 1, 944.7 [748.1] in group 2 and 819.3 [639.6] in group 3, p=0.444). There was a paradoxically substantially elevated LnRHI in acute COVID-19 than past infection and controls because of the lower resting PAT amplitude (0.73 [0.32] vs. 0.53 [0.31] vs. 0.44 [0.23], respectively; p=0.013) (Figure A). Additionally, in group 1 patients, LnRHI normalised significantly from acute COVID-19 to past infection stage (0.73 [0.32] vs. 0.49 [0.28], respectively; p=0.005) (Figure B). Acute COVID-19 showed substantially higher augmentation index compared to past COVID-19 and controls (9.6 [19.1] in group 1, 6.97 [18.6] in group 2 and -0.35 [20.53] in group 3; p=0.045 for COVID groups vs. controls).
Non-invasive evaluation of systemic vascular endothelial function with PAT showed substantial differences among patients with acute COVID-19, past COVID-19 and controls. Lower baseline PAT amplitude and high augmentation index recommend vasoconstriction at rest in the acute phase of COVID-19. These results open new research opportunities to demonstrate the forecasting value of PAT in COVID-19 patients.
Early Experience Utilizing Bivalirudin as Anticoagulation in Extracorporeal Membrane Oxygen in Coronavirus Disease 2019
Extracorporeal membrane oxygenation (ECMO) is used as rescue treatment in patients detected with coronavirus disease 2019 (COVID-19) with refractory respiratory or cardiogenic failure. Systemic anticoagulation with heparin remains the first choice for thromboembolism prophylaxis in ECMO-managed patients. But, heparin has the risk of severe complications, such as heparin-induced thrombocytopenia (HIT), and obtained antithrombin deficiency. Bivalirudin has been recommended as an alternative anticoagulant since it neither needs anti-thrombin III monitoring nor activates HIT.
There data on the use of bivalirudin in patients with COVID-19 managed with ECMO is very inadequate. Jones C, presented a session at the European Society of Cardiology (ESC) Congress 2021: The Digital Experience on 29th August 2021 which assessed the clinical safety and effectiveness of using bivalirudin. 17 patients diagnosed with COVID-19 were retrospectively reviewed who were treated with ECMO from 7/31/2020 to 12/20/2020. All patients acquired bivalirudin for thromboprophylaxis while on ECMO support.
The mean age of the study group was 45 years. 13 patients (76.4%) were of either Hispanic or African American descent. Of the 17 patients, 6 (35.3%) patients showed deep venous thrombosis and 1 (5.9%) patient showed pulmonary embolism. Two (11.8%) patients showed a clotted circuit that needed exchange. 15 (88.2%) patients exhibited hemorrhage needing transfusion with the gastrointestinal tract as the most frequent bleeding site. 9 (52.9%) patients showed thrombocytopenia. Six (35.3%) patients were discharged home or to a long-term acute care center; 11 (64.7%) patients died. The average length of stay was 37 days.
In the small case series, while using bivalirudin as anticoagulation of choice in patients diagnosed with COVID-19 and treated with ECMO exhibited high rates of complications and mortality. Additional studies are required to assess the optimal anticoagulant in this population.

