Ma HP. BMC Cardiovasc Disord. 2021;21:40.
The number of patients undergoing cardiac surgery is rising annually, and these patients are more vulnerable to the effects of perioperative anemia. In patients with cardiovascular disease (CVD), perioperative anemia is independently correlated with a substantially elevated risk of postoperative mortality and major complications. Blood transfusion is considered the most effective perioperative anemia management practice, which is of critical significance in cardiac surgery since it is directly correlated with oxygen supply and delivery. A simple and precise scoring system to accompany perioperative blood transfusion in patients with coronary artery disease (CAD) undergoing cardiac surgery is missing. The trigger point for blood transfusions for these patients can vary from current transfusion guidelines. Thus, Ma HP, et al., conducted a study to analyse the safety and effectiveness of Cardiac Peri-Operative Transfusion Trigger Score (cPOTTS) in accompanying perioperative blood transfusion in surgical patients with coronary heart disease via a clinical randomized controlled trial, putting the base for accurate transfusion strategies for this patient population.
From January 2015 to May 2018, this multicenter randomized controlled trial was executed at three third-level grade-A hospitals. The patients were incorporated after the diagnostic criteria for CAD outlined using the International Society for CVDs and the World Health Organization. A total of 1512 patients were analysed for eligibility. Finally, 1005 patients were enlisted in the study following exclusions for various medical and other reasons: 503 patients were allocated to the cPOTTS group and 502 patients to the conventional group. Of these, 505 patients (50.2%) (249 in the cPOTTS group and 256 in the traditional group) were additionally excluded following intraoperative haemoglobin (Hb) was not decreased to 10 g/dL, loss of blood flow or other reasons arised in not completing the trial, leaving 500 patients (254 in the cPOTTS group and 246 in the conventional group) as the final analytic sample. The mean age of the cPOTTS group was 63.3 ± 10.8 years, although the mean age of the conventional group was 64.4 ± 10.6 years. A majority of patients were male (65% and 63% in the cPOTTS and conventional group, respectively), with NYHA class II (47.6% and 47.2% in the cPOTTS and conventional group, respectively), were without analysis of vessels concerning CAD, showed hypertension, took the aprotinin and were without previous cardiac surgery.
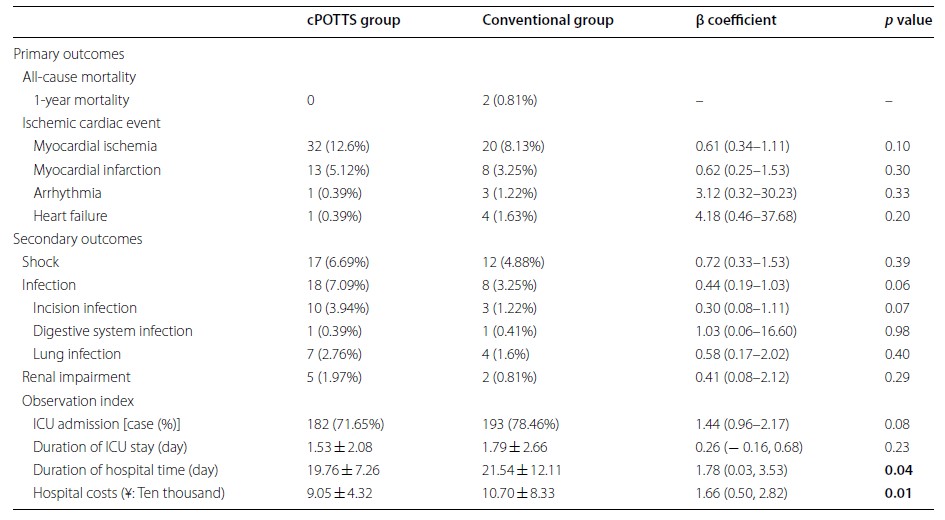
The cPOTTS and conventional groups showed similar Hb concentrations at the time of randomization (mean 114.99 ± 16.55 g/dL vs 114.02 ± 19.99 g/dL, p = 0.555). These two groups exhibited no substantial differences concering baseline characteristics, except for hemofiltration or dialysis, and New York Heart Association (NYHA) class in I, substantially greater in the conventional group. The mean intraoperative blood loss of patients was 395.77 ± 367.68 mL in the cPOTTS group and was 476.30 ± 385.20 mL in the conventional group. The conventional group acquired blood transfusions as compared to the cPOTTS group (n = 68; 26.8% vs n = 134; 54%, p = 0.017). Logistic regression analyses showed no statistical differences among the two groups in primary outcomes, incorporating 1-year mortality and ischemic cardiac incidents (myocardial ischemia, myocardial infarction, arrhythmia, heart failure); secondary outcomes were shock, infections (incision infection, digestive system infection, lung infection); renal impairment; and observation index, incorporating ICU admission and extent of ICU stay. But, the conventional group showed substantially longer hospital stays and greater hospital costs as compared to the cPOTTS group [β = 1.78, 95% confidence intervals (CI) 0.03–3.53, p = 0.04; β = 1.66, 95% CI 0.50, 2.82, p = 0.01, respectively] (Table 1).
Table 1: Primary and secondary outcomes and observation indexes
In the subgroup analyses of perioperative ischemic cardiac events; cPOTTS group showed substantially lower odds ratios in perioperative ischemic cardiac events as compared to the conventional group in the non-hypertension subgroup (OR = 0.17, 95% CI 0.04–0.80, p = 0.012). however, no substantial differences were found among the two groups in other subgroups (Figure 1).
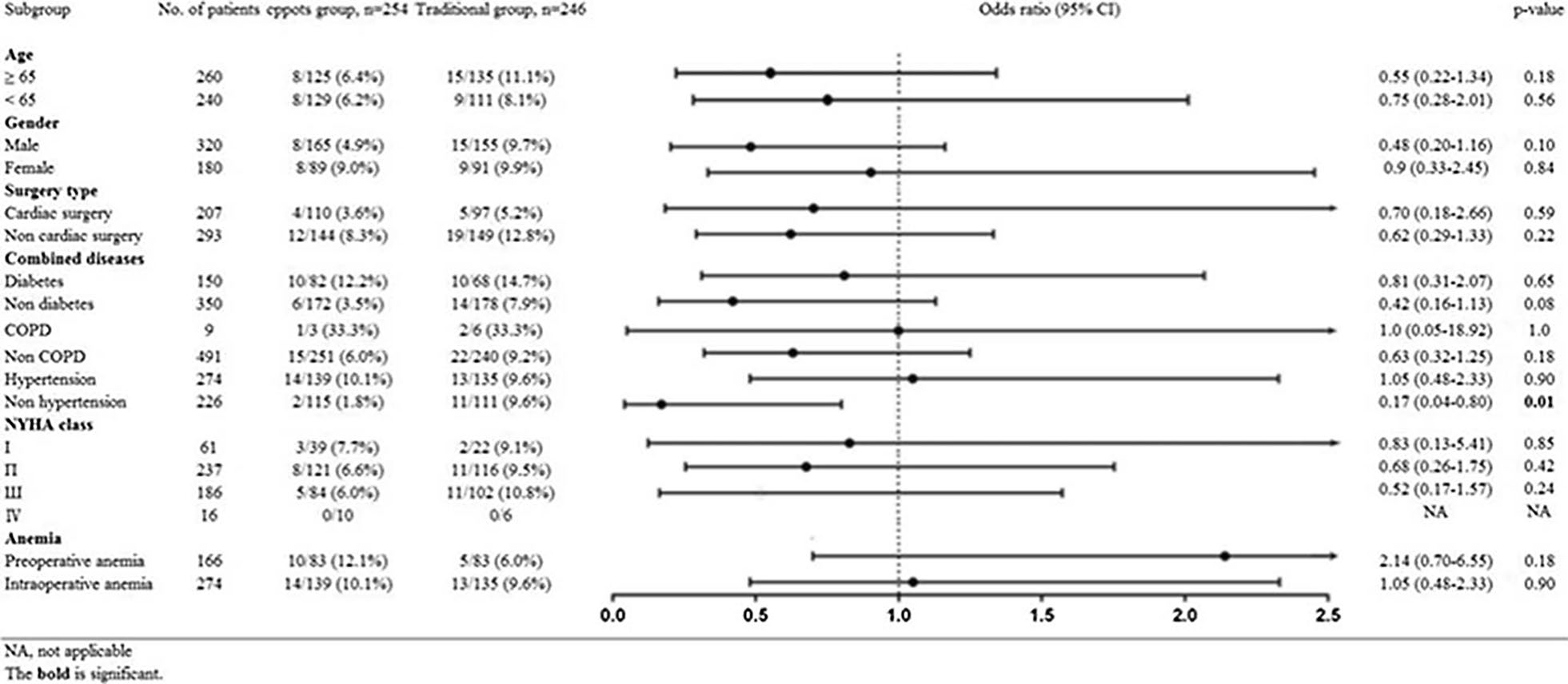
Figure 1: Subgroup analysis of patient characteristics for perioperative ischemic cardiac events between groups
Thus, it was concluded that the Cardiac Peri‑operative Transfusion Trigger Score analysis strategy showed better or equal execution with conventional transfusion guidelines to accompany the application of RBC transfusion in patients with coronary artery disease. This scoring strategy was closer to patients’ physiological requirements for transfusion, decreasing perioperative complications, usage rates and per capita consumption of RBC as compared to surgeon and/or anesthesiologist experience‑based subjective evaluation. Thus, cPOTTS scores could be a realistic and viable strategy for individualizing perioperative blood transfusion in patients with coronary artery disease.

