Dodeja AK. Open Heart. 2021 Aug;8(2):e001587.
Traditionally, women with cardiomyopathy (CM) are frequently advised to avoid pregnancy given the high risk for maternal major adverse cardiovascular events (MACE). Though, with advances in medical care, women with CM repeatedly seek counselling to precisely measure individual risk in pregnancy. The heterogeneous nature of CM induces risk stratification challenging. Thus, Dodeja AK, et al. conducted a study to analyse maternal cardiovascular outcomes in the tertiary care centre’s high-risk cardio-obstetrics programme, to analyse the effect of CM phenotype on peripartum and post pregnancy outcomes and results were qualitatively compare to systematic literature review from the same time period (2009–2019).
The baseline demographic data, type and duration of underlying CM, results from cardiac studies (echocardiogram, cardiac magnetic resonance imaging, etc.), guideline directed medical therapy (GDMT) use, maternal outcomes, obstetric outcomes and fetal outcomes were gathered. A maternal functional class and cardiac function at most recent follow-up, when accessible were also evaluated to estimate the late impacts of pregnancy in women with underlying CM. Composite maternal MACE (composite MACE) was described in the setting of pregnancy as any one of the following: maternal death, inotrope use, requirement of left ventricular assist device (LVAD), orthotopic heart transplant (OHT) and/or escalation in OHT listing status, acute decompensated heart failure and sustained ventricular tachycardia (VT) or ventricular fibrillation (VF). All composite MACE events were assessed up to 1 year following delivery.
From 875 women (979 pregnancies), 32 showed CM (29±7 years old, gravida 3±3, para 1±1, left ventricular ejection fraction ((LVEF) 41%±12%). CM phenotypes included: 3 ischaemic CM (ICM), 10 peripartum CM (PPCM), and 19 non-ICM (NICM). Women with the NICM phenotype were most likely to have used beta-blocker treatment (16 (84%) vs 4 (40%) PPCM & vs 2 (66%) ICM, p=0.05). While there was no difference in LVEF at baseline (MACE vs No MACE: 35±11% vs 43±12%, p=0.22), women with MACE showed a substantial decrease in LVEF post-partum (27%±5% vs 41±2%, p<0.05) at 32±13 days. The same women continued to show constantly depressed LVEF (28%±5% vs 44±2%, p<0.01) at late a follow-up of 1.4±0.3 years post-delivery (Table 1, Figure 1).
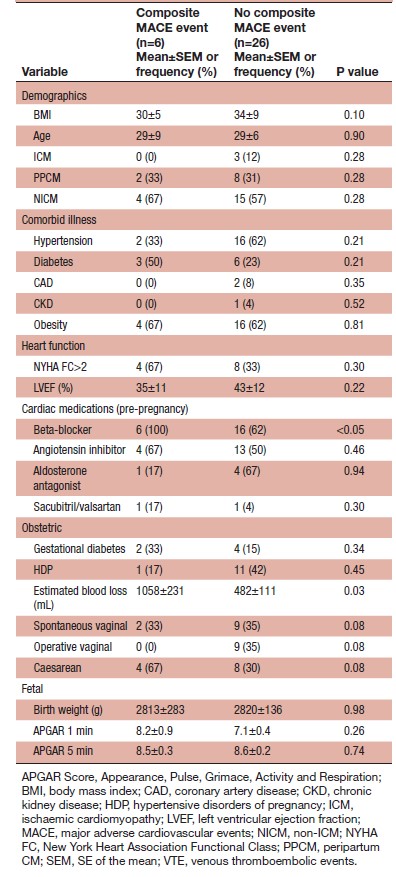
Composite MACE events happened in 6 (18%) women (2 (33%) PPCM, 4 (67%) NICM), who were more likely to be have received beta blocker treatment (6 (100%) vs 16 (62%), p<0.05). (Table 2).
Table 1: Demographic data
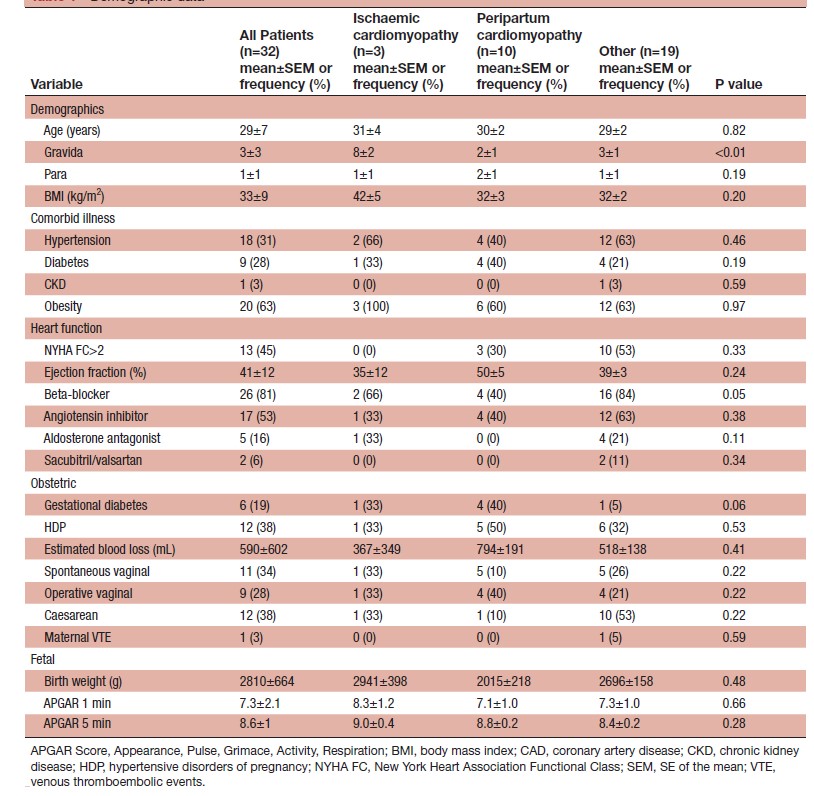
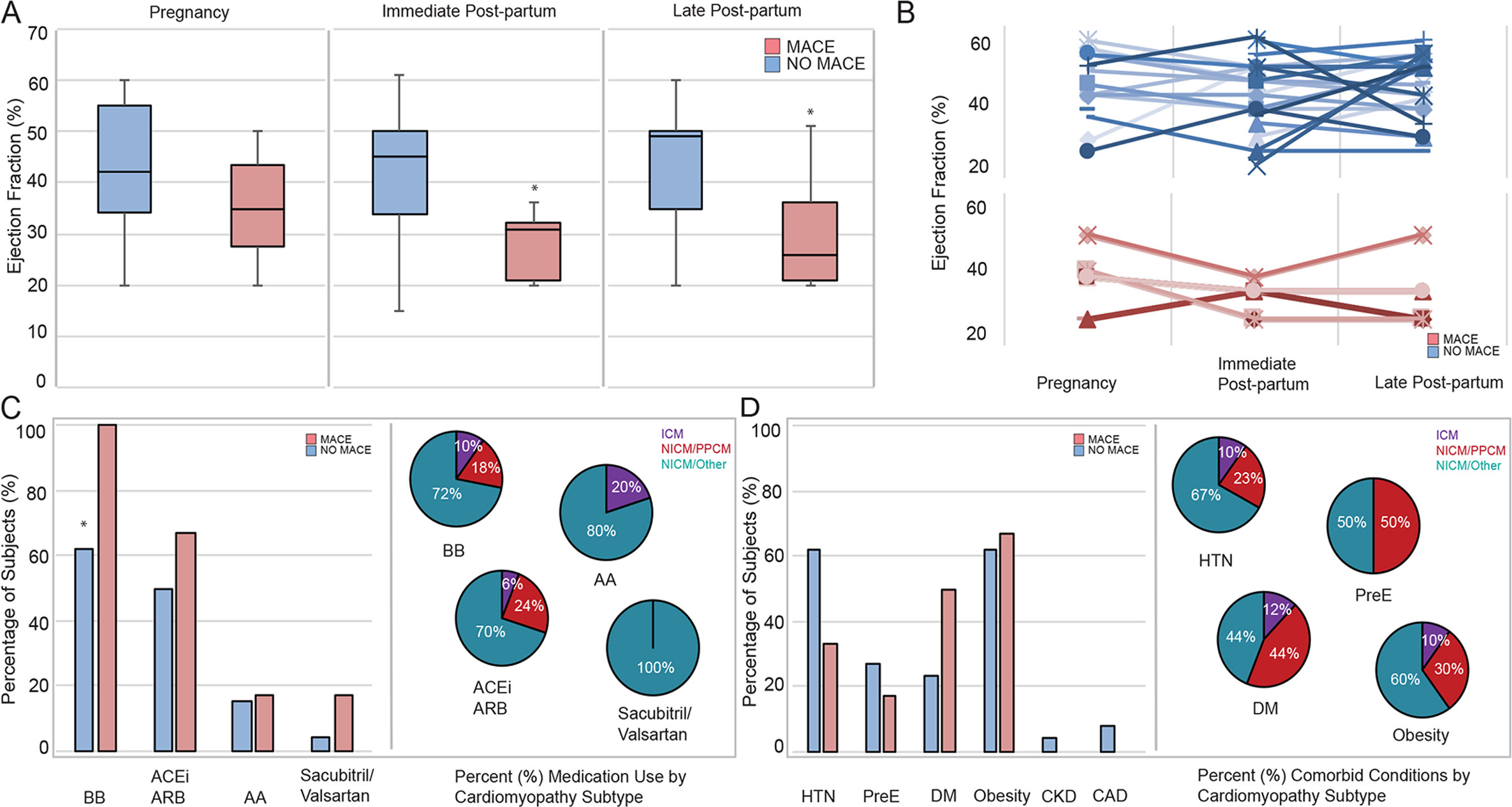
Figure 1: Maternal cardiovascular outcomes. In 32 women with underlying cardiomyopathy (CM) and pregnancy, six women had a major adverse cardiovascular event (MACE).
Left ventricular ejection fraction (LVEF) at baseline was similar in the mace and no mace groups, however, women with mace had lower LVEF in the immediate post-partum (27%±5% vs 41±2%, p<0.05) and at late follow-up (28%±5% vs 44±2%, p<0.01). (A) Subject-level data indicating EF in pregnancy, immediately post-partum and late post-partum in those with and without mace are shown (B) women with mace events were more likely to be taking a beta blocker, however, there was no difference in other cardiovascular medication (C) or underlying comorbid medical illness (D) based on subtype of CM. The pie charts demonstrate the proportion of women with medication prescription or comorbid disease prior to pregnancy, relative to the subtype of CM (C, D). CAD, coronary artery disease; CM, cardiomyopathy; CKD, chronic kidney disease; NICM, non-ischaemic CM; PPCM, peripartum CM
Table 2: Composite maternal MACE events
It was concluded that maternal MACE rates were lower as compared to previously outlined, and were less frequent in PPCM than ICM and NICM in this contemporary group of women with CM. Heart function in women with MACE was negatively affected immediately following delivery and recommending that pregnancy itself likely has impact on future left ventricular function in women with underlying CM in late postpartum follow-up.

