Beyond PVR: Assessing and Managing the Dysfunctional Right Ventricle
Manreet Kanwar, Co-division Director, Advanced Heart failure and Pulmonary hypertension cardiology, Allegheny General Hospital, Pittsburg, discussed about the topic “Beyond PVR: Assessing and managing the dysfunctional right ventricle” at the HFSA, 2021.
Right heart failure is a hemodynamic disorder with changes in pressure or right ventricle (RV) metrics, changes in NT-proBNP, changes in functional class (FC) and 6 minute walking distance (6MWD), changes in weight and subsquent hospitalization. Acute right heart failure (ARHF) can occur because of abruptly increased RV afterload or decresed RV contractility. Chronic (CRHF) most commonly results from gradual increases in RV afterload caused by pulmonary hypertension (PH) most frequently from LH failure. Each of these conditions present unique challenges for the RV.
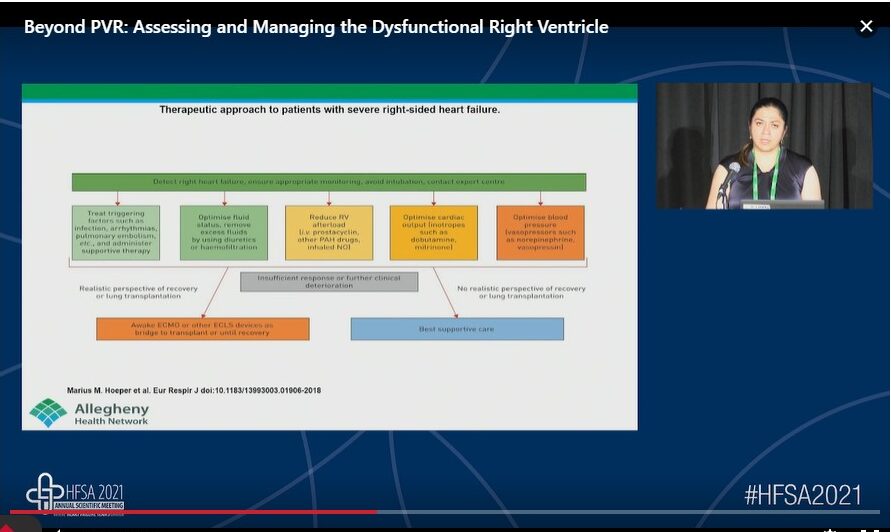
RV dysfunction is very common in end stage left heart failure and is a key predictor of morbidity and mortality. Practical management of RHF requires determining the aetiology and chronicity; evaluation of hemodynamics; treating predisposing factors; and medical and surgical management based on optimization of preload, afterload and contractility. Evaluation of potential triggers for acute RHF includes progression of underlying pulmonary vascular disease, medication/diet non-adherence, pulmonary embolism, new/worsening pulmonary process or infection, surgery, medical conditions i.e. hyperthyroidism, pregnancy/delivery and arrhythmias. The important considerations of management of RHF includes:
- Optimal management requires a multifaceted approach addressing RV preload, afterload, and contractility
- Stabilise the cardiac output and manage rhythm disturbances
- Lower pulmonary vascular resistance
- Use of mechanical circulatory support is reserved for patients in acute or chronic RVF refractory to optimal medical therapy and it is used as a bride to recovery or bridge to transplant
In acute decompensated right heart failure, using a combination of strategies to decrease preload, stabilize cardiac output and lower PVR is critical. Treating the etiology is crucial. Temporary mechanical support strategies such as Venoarterial Extracorporeal Membrane Oxygenation and right ventricular assist device may play a role in stabilizing end organ function in critically ill patients.
Rehospitalization Following Inpatient CardioMEMS Implantation: Insights from the Nationwide Readmissions Database
Charles Sherrod, et al., presented a poster session on the topic “Rehospitalization following inpatient CardioMEMS implantation: Insights from the nationwide readmissions database” at the HFSA, 2021.
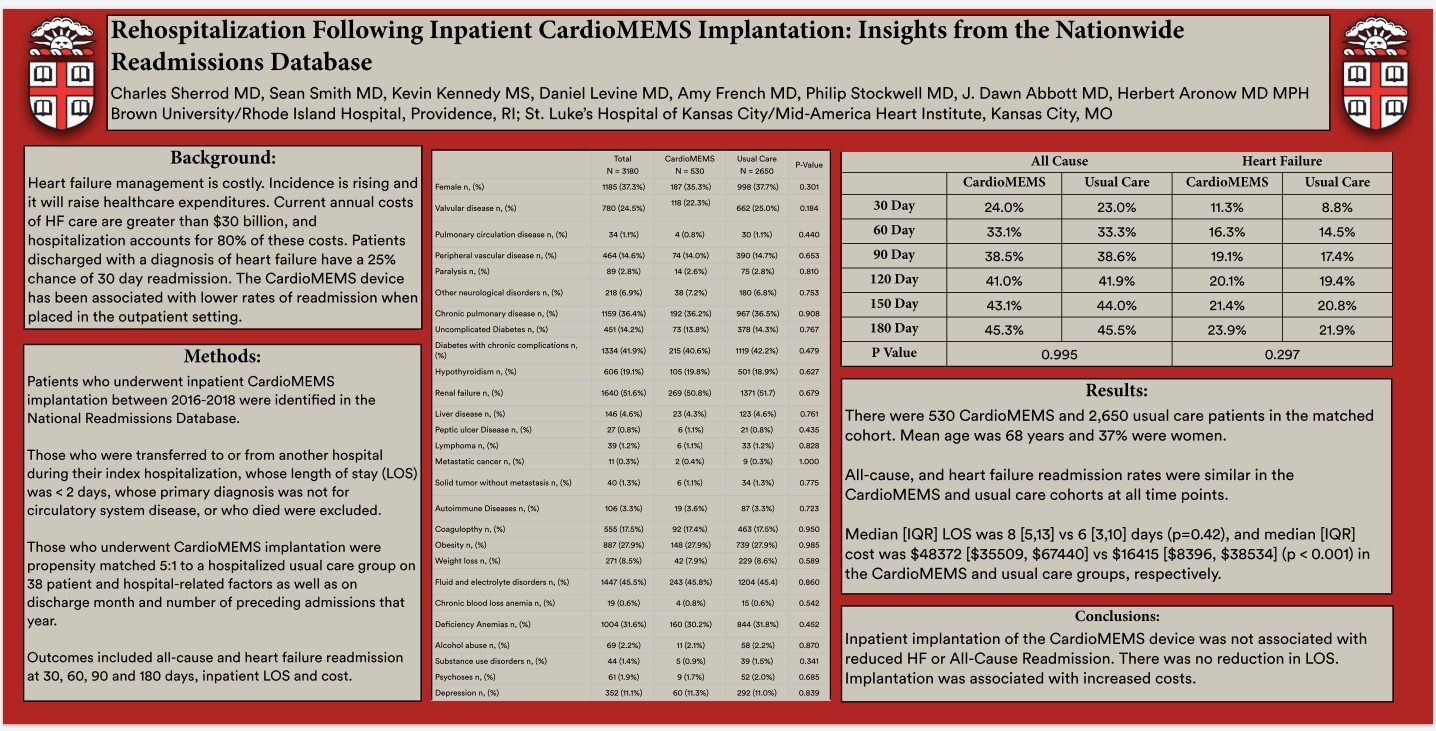
Heart failure management is costly. Incidence is rising and it will raise the health care expenditure. Patients discharged with a diagnosis of heart failure have a 25% cahnce of 30 day readmission. The CardioMEMS device has been assocaited with lower rates of readmission when placed in the outpatient setting.
Patients who underwent inpatient CardioMEMS implantation between 2016-2018 were identified in the national readmissions database. Those who were transferred to or from another hospital during their index hospitalization whose length of stay (LOS) was < 2 days, whose priamry diagnosis was not for circulatory system disease or who died were excluded. Those who underwent CardioMEMS implantation were propensity matched 5:1 to a hospitalized usual care group on 38 patient and hospital-related factors as well as on discharge month and number of preceding admissions that year. Outcomes included all-cause heart failure readmission at 30, 60, 90 and 180 days, inpatient LOS and cost.
Results observed were all cause, and heart failure readmission rates were similar in the CardioMEMS and usual care cohorts at all time points. Median (interquartile range LOS was 6 days (p=0.42) an median (IQR) cost was $48372 vs $16415 (p<0.001) in the CardioMEMS and usual groups, respectively
Inpatient implantation of the CardioMEMS device was not associated with reduced HF or all-cause readmission. There was no reduction in LOS. Implantation was associated with increased costs.
The SCAI is the Limit: Quantification and Classification of Shock
Jacob C. Jentzer, Director of Research, Cardiac Intensive Care Unit, Mayo Clinic, Rochester MN, USA, talked about the much-needed topic in today’s time “the SCAI is the limit: Quantification and classification of shock.” at the HFSA Annual Scientific Meeting 2021.
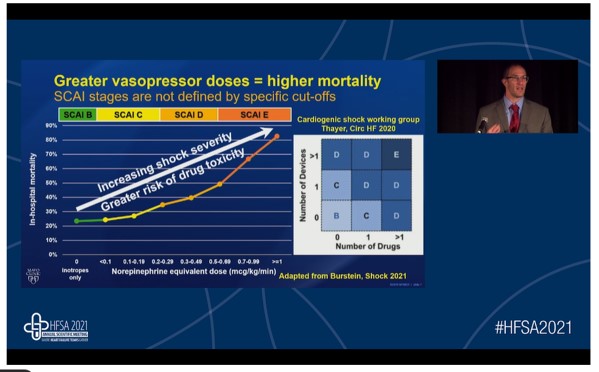
He started his presentation with a very valid and important question, “why does shock severity grading matter?” The answer to this question is that the grading of shock severity is vital for predicting the short-term outcomes, triage and transfer decisions, and determining the need to escalate therapies. The Society for Cardiovascular Angiography and Interventions (SCAI) has given shock classification with the severity of shock being escalated from stage A to E. A and B stages are the pre-shock stages whereas stages C, D, and E can be defined as classic cardiogenic shock stage, deterioration stage, and extremis stage, respectively. SCAI stage E is characterized by severe acidosis and markedly elevated lactate levels. The severity of shocks i.e. escalation from stage A to E is associated with short-term mortality and these findings have been reported to be true for all patient subgroups i.e. acute coronary syndrome/ heart failure. Hence shock severity could be defined by several factors; hemodynamics/, end-organ hyperfusion, hemodynamics support, and response to initial therapy. It is of great interest to note that the greater vasopressor dose is associated with the high risk of mortality as the increase in shock severity increases the risk of drug toxicity. Mortality can be predicted by the severity of lactic acidosis. A cut-off value of >5mmol/L for lactate levels is often used however, the high value is worse. All mortality risk factors are not associated with shock severity; only lactate and renal function are related to shock severity.
Older age, cardiogenic arrest and rhythm, worsening shock, poor hemodynamics, abnormal echocardiography, systemic inflammation, acute kidney injury, and phenotypic cluster are some of the mortality risk modifiers i.e. they influence survival across the various SCAI shock stages. Different cardiogenic shock phenotypes are non-congested, cardiorenal, and hemometabolic type and amongst the SCAI stages C, D, and E, the hemometabolic phenotype is associated with greater in-hospital mortality compared to the other two.
The SCAI classification of shock is a comprehensive tool to predict the short-term outcomes, triage and transfer decisions, and to determine the need to escalate therapies in patients with cardiogenic shocks.
The Implicit Bias in Transplant/LVAD Selection Committee Meetings and the Impact on Patient Care
Raymond Givens from the Advanced Heart Failure and Transplant, Emory University School of Medicine, USA, presented his insights on the topic, “The implicit bias in transplant/LVAD selection committee meetings and the impact on patient care” at the HFSA Annual Scientific Meeting 2021.
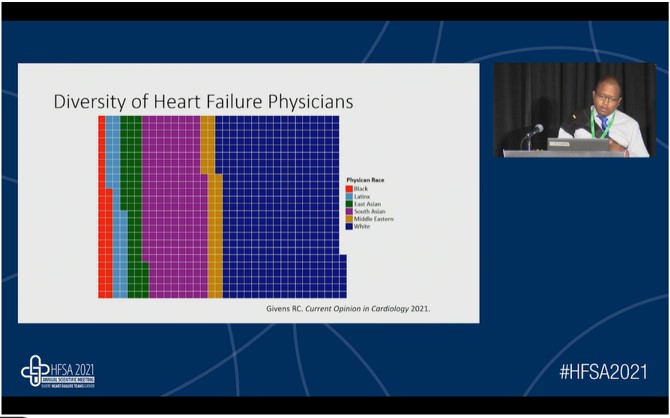
In the advanced heart failure (HF) therapy evaluation, healthcare physicians consider certain medical and psychosocial factors based on the race and origin of the patients. E.g. black candidates are most likely to be sensitized, have higher panel-reactive antibody (PRA) levels, and are more likely to develop de novo donor-specific antibodies (DSAs). As per a recent study, among HF professionals randomized to standardized vignettes, race figured prominently in thought processes about decision-making. Adherence and social history were important factors in decisions about black patients. Black patients were assumed to be sicker and less likely to be adherent. Providers thought they might have difficulty forming a rapport with the black patient. White patients are more likely to be offered heart transplants whereas black patients are more likely to be offered left ventricular assist devices (LVAD). In another study, children were seen as particular liabilities for women especially black women to whom respondents attached concerns about financial stability. The implicit bias results from cognitive processes outside conscious awareness. Pro-white implicit bias is as prevalent among physicians as the general population and is associated with quality of patient interactions, treatment decisions, quality of care, treatment adherence, and outcomes. Most studies reported that those with high levels of pro-white bias have greater difficulties with patient-provider communication.
Implicit bias reduction training might yield meaningful outcomes. A cluster-randomized trial at a large university showed positive short-term changes in women faculty perceptions that their ideas were taken seriously. Brain regions implicated in implicit bias include the amygdala, dorsolateral prefrontal cortex, and fusiform gyrus. Propranolol reduces implicit association scores among white subjects who were shown images of black faces. Dr. Raymond mentioned certain recommendations to manage the implicit bias. He also showed a graph that depicted the diversity of HF physicians; the majority of HF physicians were white.
Implicit bias reduction training should be provided to the HF physicians so that advanced HF therapy can be given to every patient, irrespective of their race and origin.
Clinical Outcomes One Year Post-implant in Patients with Left Ventricular Assist Devices and Pre-implant ICD Shocks
David G. Hann gave an enlightening poster presentation at the HFSA Annual Scientific Meeting 2021. His presentation was focused on the topic “clinical outcomes one year post-implant in patients with left ventricular assist devices and pre-implant ICD shocks.”
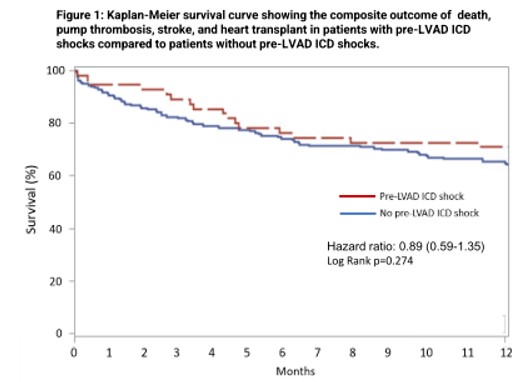
Implantable cardioverter-defibrillator (ICD) shocks after left ventricular assist device therapy (LVAD) are linked to adverse outcomes and may increase mortality. However, there is limited data on the association of pre-LVAD ICD shocks on post-LVAD clinical outcomes. Thus, the objective of the study was to evaluate if pre-LVAD ICD shocks within one year pre-implant are linked to adverse clinical outcomes up to one year post-LVAD.
The study included patients aged ≥18 years with continuous-flow LVADs and ICDs, retrospectively identified within the UPMC system from 2006-2020. The baseline characteristics were similar between the patients with pre-LVAD ICD shocks and patients without pre-LVAD ICD shocks.
Overall results of the study indicated that although pre-LVAD shocks within one year of LVAD implantation predicted the occurrence of post-LVAD ICD shocks, they were not associated with a composite outcome of death, pump thrombosis, stroke, or heart transplant at one year. Also, pre-LVAD ICD shocks predicted post-LVAD hospitalizations for ICD shocks but patients with pre-LVAD ICD shocks had a decreased incidence of heart failure admissions.
In this retrospective study of patients with pre-existing ICDs, pre-LVAD shocks within one year of LVAD implantation were not associated with a composite outcome of death, pump thrombosis, stroke, or heart transplant at one year.
Referral for Heart Failure

Maya Guglin, Director, Heart Failure, Indiana University School of Medicine, discussed about the topic “Who is the right patient/? When is the right time” under the session “Referral for Heart failure” at the HFSA, 2021.
Dr Maya presented a case of 68-year-old male with history of STEMI (acute totoal LAD occluison) one year ago which resulted in ischemic cardiomyopathy with LVEF 20% presented with increasing shortness of breath and edema. The patient could barely walk across the room. He was on lisinopril, carvedilol and furosemide. He was also recently tapped for ascites, His BP was 96/67 mmHg and heart rate of 104 bpm. He was admitted for fluid overload. The right showed the following values: right atrial pressure: 18 mmHg, pulmonary artery: 82/45/51 mmHg, wedge 40 mmHg, cardiac output: 4L/min, index 2L/ min. His creatinine was 3 mg/dL.
Three critical questions were answered during the course of his treatment.
- Is transplant/LVAD indicated?
- Are there contraindications?
- Transplant or LVAD?
The patient was hospitalised and treated with inotropes, defibrilallator shocks, edema/esclating diuretics in view of heart failure NYHA class III and IV, end organ dysfunction (liver and kidneys), ejection fraction <25%, low blood pressure. Use of pulmonary artery catheter is associated with lower rates of mortality in overall and advanced stages of HF. Contraindications include for transplant severe COPD, systemic illness, malignancy with poor prognosis, liver cirrhosis, dementia or psychiatric illness, social issues (substance abuse, lack of support), pulmonary hypertension for transpant. Contraindication for left ventricular assist device (LVAD) includes RV failure.
Transplant does help in prologning the survival rate of patients with heart failure.
The Association of Resting Heart Rate with Beta Blocker Up-titration in Patients with Heart Failure and Reduced Ejection Fraction: A Single Center Experience from the Middle East
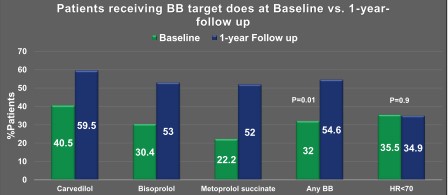
Mania Y gave a presentation at the HFSA, 2021 on the topic “The Association of Resting Heart Rate with Beta Blocker Up-titration in Patients with Heart Failure and Reduced Ejection Fraction: A Single Center Experience from The Middle East”. He aimed to determine utilization of beta-blocker patterns, predictors of BB dose up titration, and its association with resting HR in a newly established heart failure program in the Middle East.
Beta-blocker therapy is an essential part of guideline-direct medical therapy (GDMT) for heart failure with reduced ejection fraction (HFrEF). specified target dose or the maximum tolerable BB dose is associated with beneficial effects that might extend beyond those related to HR reduction.
A retrospective chart review was conducted which included 152 patients treated with a BB. Data on patient characteristics and medication use at baseline and 12-month follow-up were collected and compared between patients who did and those who did not achieve BB target dose using appropriate tests.
In this study, patients were treated with 12-months follow up, most commonly with bisoprolol (63.1%), followed by carvedilol (24.3%) and metoprolol (12.5%). More patients achieved BB target dose overtime (32% to 54.6%, p<0.01). Proportion of patients achieving resting HR<70 bpm did not change (35.5% vs. 34.9%, p=0.9). Patients receiving BB target dose at FU (n=83) were younger and more likely to be diabetic.
Nearly half of HFrEF patients did not achieve BB target dose over a year of FU, with majority of them having uncontrolled resting HR.
Tafamidis Reduces the Decline in Global Longitudinal Strain and Stroke Volume in Patients with Transthyretin Amyloid Cardiomyopathy
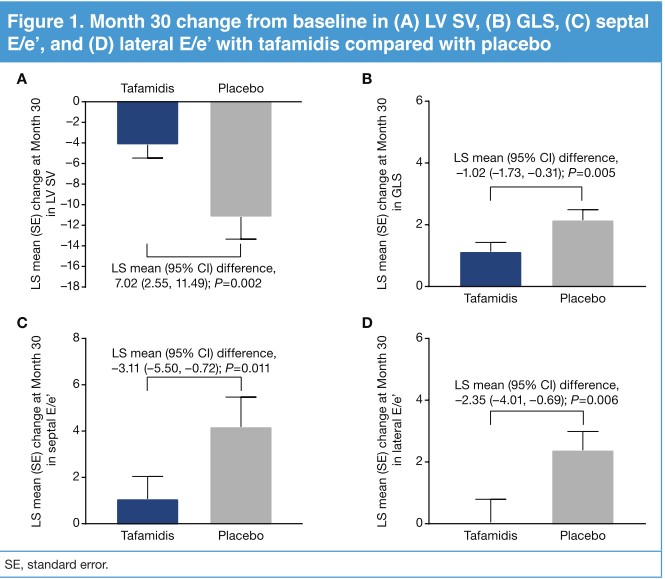
Elliot P gave a presentation at the HFSA, 2021 on the topic “Tafamidis Reduces the Decline in Global Longitudinal Strain and Stroke Volume in Patients with Transthyretin Amyloid Cardiomyopathy” . This study aimed to hypothesise that treatment with tafamidis significantly reduces the worsening of echocardiographic variables in patients with transthyretin amyloid cardiomyopathy (ATTR-CM)
The significant predictors of mortality in patients with transthyretin amyloid cardiomyopathy (ATTR-CM) are echocardiographic measures, including global longitudinal strain (GLS) and stroke volume (SV). In the Tafamidis in Transthyretin Cardiomyopathy Clinical Trial (ATTR-ACT), tafamidis significantly reduced mortality and cardiovascular-related hospitalizations.
In this trial, patients were randomized to tafamidis 80 mg (n=176) or placebo (n=177) for 30 months. Echocardiography was conducted at enrolment, and at Months 6, 18, and 30, using a standardized protocol with all images reviewed and analysed by an independent central laboratory.
At month 30, there was a significant reduction in least-squares (LS) mean difference (95% CI) with tafamidis vs placebo for each measure. The decline in SV and GLS was apparent from Month 6 in all patients, while the difference between tafamidis and placebo groups was apparent from Month 18 and through to Month 30. The decline in E/e’ (indicative of elevated LV filling pressures) was apparent from Month 6 and through to Month 30 with placebo but only minimally changed at each time point with tafamidis
Treatment with tafamidis significantly reduced worsening of LV systolic function (GLS, SV) and diastolic function (E/e’) over 30 months in patients with ATTR-CM.
Implementing GDMT in Severe Heart Failure Patients – Easy or Challenging? A Debate (No CEUs)
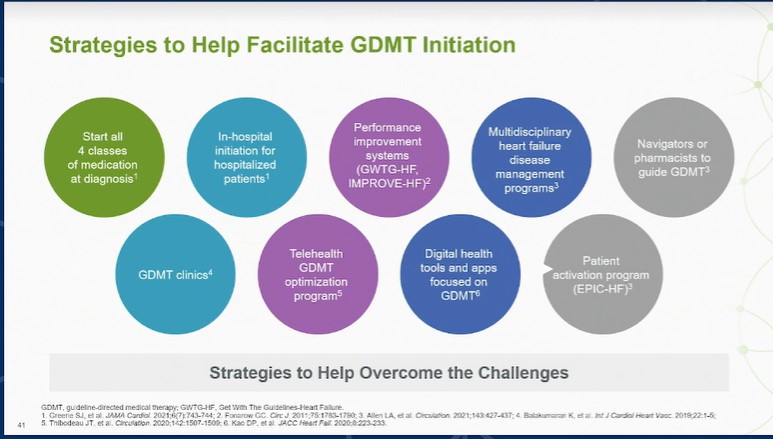
Albert N and Fonarow G presented a session at the HFSA, 2021 on the topic “Implementing GDMT in Severe Heart Failure Patients – Easy or Challenging? A Debate (No CEUs)”. Nancy Albert and Fonarow G aimed to emphasise on the fact that GDMT should be easy and there are US guidelines and recent consensus pathway which offer specific details about medical therapy.
National guidelines assume that if patients can tolerate medications, we must document patient adverse effects and contradictions, patient preferences, target doses when not supported by RCTs and national guidelines, and titration plan. Implementation/monitoring programs are common in HF clinics, transitional care programs, shared medical appointments, and hospital up titration predischarge.
GDMT in acute HF settings provide helpful systems/tools like prognosis and risk scores, eMR cues and flags, pocket card, and “see something say something” approach. Stakeholders of GDMT in heart failure are system, insurance, provider, industry, family, patient, friends, and community supporters.
Implementation of GDT is easy and success requirements depend on agreeing on what severe HF means, open and honest patient communication, and utilization of resources including pharmacy, screening for cognitive dysfunction, treatment of underlying disease, and assure that providers are fully educated. Reasons for underutilization of GDMT are gaps in knowledge and awareness, lack of systems, therapeutic inertia, uncertainty regarding effectiveness, concerns about side-effects, costs, and value, and various other challenges
GDMT implementation can be challenging in severe patients. The optimal approach to GDMT implementation is to utilize each medication demonstrated to reduce all-cause mortality.
Arrhythmia Assessment with 30-day MCT Patch Challenges Traditional Holter Monitoring
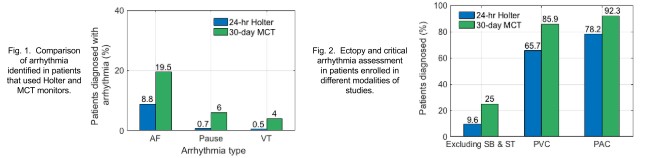
Mahajan R gave a presentation at the HFSA, 2021 on the topic “Arrhythmia Assessment with 30-day MCT Patch Challenges Traditional Holter Monitoring”. She aimed to identify if cardiac monitoring with a 30-day MCT patch provides better patient outcomes than with the 24-hr Holter. To do so, we compared the arrhythmia and ectopy diagnostic yield of both modalities.
It was conducted as a retrospective study to analyse data ECG data recorded from 14,514 patients (male-43%, female-57%, median age-64 years). Patient’s data was also evaluated to identify sinus rhythms -sinus bradycardia (SB) and sinus tachycardia (ST), and any of the following arrhythmias, atrial fibrillation, pause, and Ventricular tachycardia (VT). Mean arrhythmia diagnostic yield of 38.1% in 30-day MCT studies is significantly different from 29.1% in 24-hr Holter studies (p<0.001). A total of 25% critical arrhythmias in patients with MCT patches in contrast to 9.6% in Holter. PVC beats were identified in 85.9% and 65.7%, whereas PAC beats in 92.3% and 78.2% of MCT and Holter studies, respectively
Results demonstrate that 30-day monitoring with MCT patch provides a better diagnostic yield than 24-hr Holter monitoring. Timely diagnosis with MCT patch can aid in early therapeutic intervention resulting in better patient care.

