Mishra BH, et al. Bone. 2020 Feb;131:115160.
Mishra BH, et al., conducted a study to determine the effect of diabetes mellitus (DM) on periprocedural complications and clinical outcome in patients with heart failure (HF) experiencing implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy (CRT) implantation.
Details from 50 German centres were obtained between January 2007 and February 2014 from the German Device Registry. A retrospective analysis of n = 5329 patients experiencing ICD implantation was performed. Patients’ characteristics, procedural data, periprocedural complications, and post-procedural clinical outcome, which also include a composite clinical endpoint of all-cause mortality, stroke, and myocardial infarction (MACCE), were assessed. For ICD and CRT implantations, subgroup analysis was conducted.
During the study period, 5329 patients with ICD or CRT defibrillator (CRT-D) devices were recruited. Among them, diagnosis of DM observed in 1448 patients (27.2%). Within the cohort, diagnosis of HF was observed in 94% of DM and 90% of non-DM patients. In terms of chronic kidney disease (CKD), 920 patients were grouped to CKD and 4409 patients to non-CKD.
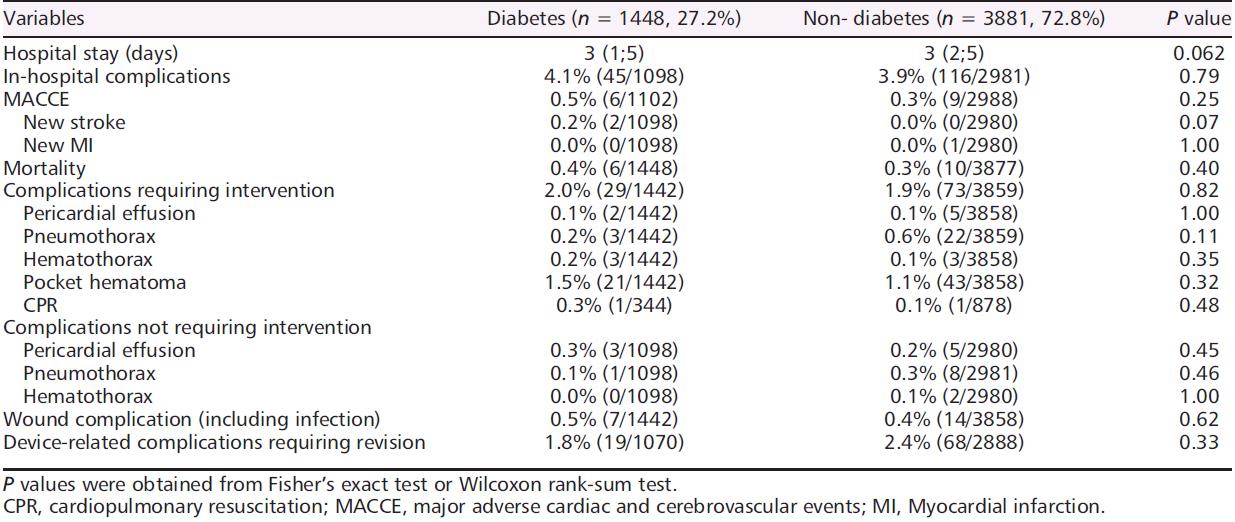
Extensive overview of the in-hospital events including the periprocedural complications showed in Table 1. Complication rates were identical in 4.1% with diabetic patients as compared to 3.9% with non-diabetic patients (p = 0.79, Table 1).
Table 1: In-hospital events
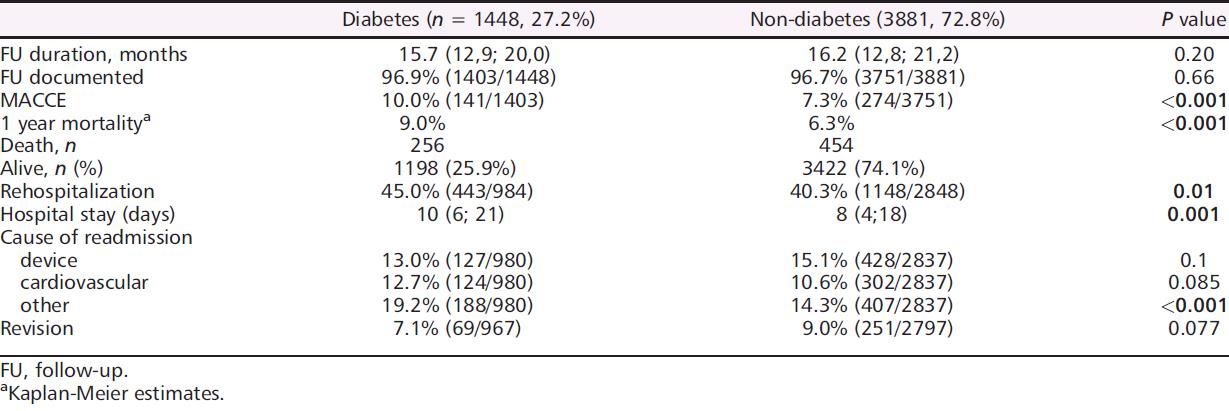
Of 5329 patients recruited, 1 year follow-up was conducted in 5154 patients (96.7%). Predefined MACCE observed in 425 patients (8.2%). Median follow-up was 15.7 (12.9; 20.0) and 16.2 (12.8; 21.2) months in DM and non- DM patients. All results are shown in Table 2.
Table 2: Follow-up at 12 months
Initial time-to-event analysis showed a poor outcome of patients with DM in terms of 1 year mortality (log-rank, p = 0.001; Figure 1A). Constant to the all-over cohort, the subgroup analysis of ICD patients demonstrated a worse diagnosis of diabetic as compared to patients with non-diabetic (Figure 1B). While no significant differences prognosis was observed in terms of the presence of DM in the smaller subgroup of CRT patients (Figure 1C).
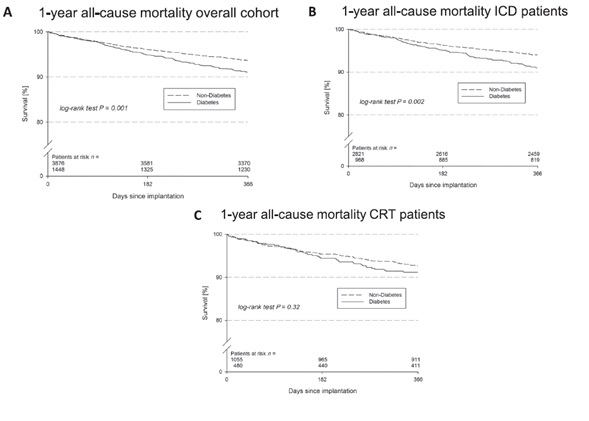
Figure 1: (A) Overall outcome analysis of 1 year mortality, according to presence of diabetes: Kaplan–Meier curve for the time to the first event of all-cause death after 1 year in patients with diabetes (dashed line) and without diabetes (solid line). Kaplan–Meier survival curves for the time to the first event of all-cause death after 1 year in diabetes (dashed line) versus non-diabetes (solid line) patients in the subgroup of (B) implantable cardioverter defibrillator recipients and (C) cardiac resynchronization therapy recipients.
An adjusted analysis was conducted to balance for the covariates age, sex, coronary artery disease, HF, and CKD (Figure 2). The findings of adjusted models did verify an equivalent risk for periprocedural complications in both groups independent from the presence of DM. The adjusted calculations for outcome disappointed to show a contrast between the two groups with regard to 1 year MACCE, the composite of cardiopulmonary resuscitation, ICD shocks, occurrence of ventricular tachycardias or required ablation therapy, and for the endpoint device revision as compared to the unadjusted survival analysis (Figure 2).
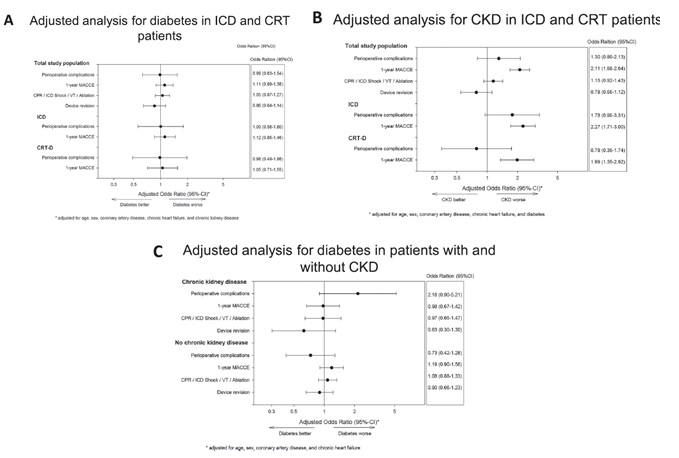
Figure 2: (A) Adjusted analyses of the effect of diabetes in the overall group after multivariable adjustment. A 95% confidence interval adjusted for age, sex, coronary artery disease, chronic heart failure, chronic kidney disease. (B) Adjusted analyses of the effect of chronic kidney disease in the overall group. (C) Adjusted analyses of the effect of diabetes and chronic kidney disease in the overall group. CRT-D, cardiac resynchronization therapy defibrillator; ICD, implantable cardioverter defibrillator; MACCE, major adverse cardiac and cerebrovascular events; VT, ventricular tachycardia.
Thus, the whole risk of periprocedural complications and short-term (1 year) clinical findings in DM and HF patients undergoing ICD or CRT defibrillator (CRT-D) implantation was not enhanced. On the other hand, CKD was linked with an enhanced risk of 1 year MACCE in patients with HF undergoing ICD/CRT-D implantation.

