Hohmann C. Sci Rep. 2020 Feb 3;10(1):1685.
The prime states susceptible to atrial fibrillation (AF) are aging, arterial hypertension, coronary artery disease, congestive heart failure and valvular heart disease. In addition, extracardiac factors such as diabetes mellitus, thyroid disease, obesity, obstructive sleep apnea and heavy alcohol consumption are known factors that are partly responsible to the progress of this arrhythmia. Several inflammatory markers such as C-reactive protein (CRP), tumor necrosis factor alpha (TNFα) or interleukin 6 (IL-6) showed correlation in the presence of both AF and the risk of developing AF in the future in the epidemiologic and clinical studies. More particularly, anti-inflammatory treatments with statins, steroids or vitamin C showed a significant reduction of AF episodes. But, there have only been few previous histological surveys evaluating the correlation among inflammation and AF considering increased inflammatory cell counts in human tissue samples and these studies partially only depend on material from bioptic samples or right atrial appendage tissue and that evaluation of distinct immune cell populations vary among the different assays. Further, data concerning immunohistochemically investigation of various stages of AF and sinus rhythm (SR) are usually lacking. Hence, Hohmann C et al., conducted a study to examine the correlation of inflammatory B- and T-cell infiltration in left atrial appendages tissues of patients with paroxysmal, persistent and permanent AF in comparison to SR. Additionally, association of the presence of atrial immune cells populations with markers of systemic inflammation was studied.
10 patients were enrolled in the monocentric, prospective observational study between 2013 and 2018. Left atrial appendages were gained from patients undergoing coronary artery bypass surgery, mitral valve repair or replacement, tricuspid valve repair, aortic valve replacement, surgical bipolar AF ablation or any combination. 2 patients with SR, 2 patients with paroxysmal AF, 3 patients with persistent AF and 3 patients with permanent AF were included in the study. In patients with SR, left atrial appendages were cut out in case of significantly dilated left atria and the presence of ≥ 3 risk factors for the enlargement of atrial fibrillation. Serum markers of inflammation were gathered before surgery in the clinical history and laboratory findings. The heart rhythm was determined from electrocardiograms just before the operation. Whole left atrial appendages were continuously stitched which were obtained during open-heart surgery and incisions.
The 4 groups (SR, paroxysmal AF, persistent AF, and permanent AF) did not vary in age, gender, heart failure status, or with regard to structural heart disorder. Inflammatory markers did not substantially vary neither among patients with SR or AF nor within the different subgroups of AF. But, in patients with persistent and permanent AF, greater levels of CRP and IL-6, resp. were observed. The AF groups showed substantially greater number of inflammatory cells recognised as CD3-positive T cells in the left atrial appendage tissues as compared to the number of inflammatory cells in the left atrial appendage tissues in the SR group (p < 0.001). (Figure 1)
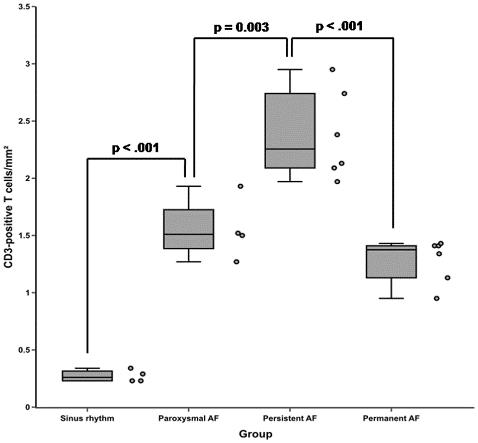
Figure 1: Frequency of CD3-positive T cells in left atrial appendage tissues of patients with sinus rhythm (SR) or paroxysmal, persistent and permanent atrial fibrillation (AF)
Though samples from the SR group and the three individual subgroups of AF patients were compared, patients with paroxysmal AF and persistent AF showed substantially greater number of inflammatory CD3-positive T cells than the SR group (p < 0.001) and subgroup of paroxysmal AF (p = 0.003) resp. Fascinatingly, these cells were generally arranged in small clusters in patients with persistent AF. Following, the number of inflammatory CD3-positive T cells was decreased and substantially lower in patients with permanent AF as compared to persistent AF patients (p < 0.001). The number of inflammatory CD3-positive T cells did not vary among the subgroups of paroxysmal and permanent AF (p = 0.502). In total numbers, the average count of CD3-positive T cells per 1 mm² was 0.27 ± 0.05 in the SR group, 1.55 ± 0.27 in patients with paroxysmal AF, 2.38 ± 0.39 in the subgroup of persistent AF and 1.28 ± 0.19 in patients with permanent AF, resp. (Figure 2)
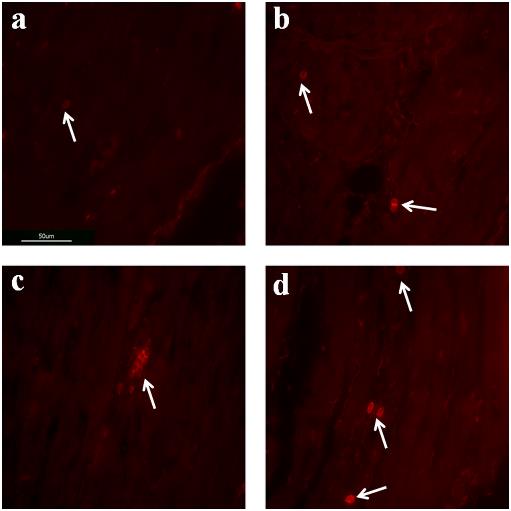
Figure 2: Immunofluorescent staining’s of human left atrial appendage tissues for CD3-positive T cells. Sections of left atrial appendage tissues demonstrating the presence of CD3-positive T cells (1 cell, white arrow) in patients with sinus rhythm (a), paroxysmal (3 cells, white arrows) atrial fibrillation (b), persistent (7 cells, white arrow) atrial fibrillation (c) and permanent (4 cells, white arrows) atrial fibrillation (d)
Thus, it was concluded that the cellular component of the immune system showed prospective important role in the evolution and perpetuation of AF. Nevertheless, further studies are required to estimate the temporal succession and consistency between inflammation and AF duration particularly considering the development of potential new therapy strategies.

