Boyalla V. Open Heart. 2021 Aug;8(2):e001653.
Internationally practice has leaned towards providing catheter ablation as first-line therapy for symptomatic paroxysmal atrial fibrillation (PAF), with high success rates. But, the success rate in ablating non-PAF is highly different, hence, appropriate patient selection is predominant. A scoring system for non-PAF, predicting successful restoration of sinus rhythm following single or multiple ablations, would be priceless for guiding patients before beginning on an invasive therapy. Such a score has not been recommended in international guidelines. Thus, Boyalla V, et al. developed an internationally relevant scoring system by first recognising baseline clinical variables independently predictive of a successful outcome of catheter ablation of non-PAF at a hospital in London (UK) and procured a scoring system to predict procedural outcomes. Later, this scoring system was externally validated between an independent group of patients at a hospital in California (USA).
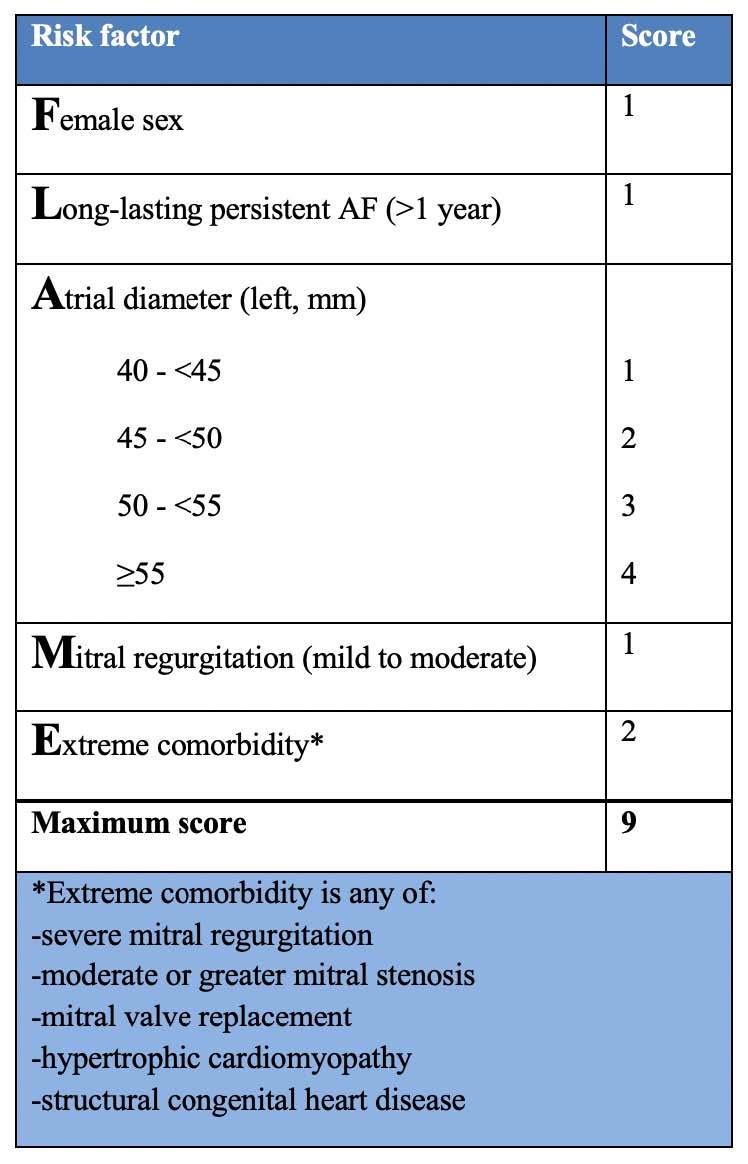
17 preoperative clinical variables were analysed as possible predictors of individual procedure outcome (IPO), as well as regardless of a redo procedure, the number of previous ablations, presence of LA tachycardia (AT) in redo procedures and follow-up duration. At a London centre, a total of 416 non-PAF ablations were analysed between 361 patients by binary logistic regression. The mean duration of follow-up was 12±3 months. Antiarrhythmic drugs were discontinued after 368 (88%) procedures. Pre-procedural variables were recognized which independently predicted freedom from atrial tachyarrhythmia. 21 possible predictive variables and a model with c-statistic 0.751-explained effect difference in London at mean follow-up 12±3 months. The FLAME score developed an additive point score (range 0–9): female=1; long-lasting persistent atrial fibrillation=1; left atrial diameter in mm: 40 to <45 = 1, 45 to <50 = 2, 50 to <55=3, ≥55 =4; mitral regurgitation (MR) mild to moderate=1; extreme comorbidity=2. Extreme comorbidities incorporate severe MR, moderate mitral stenosis, mitral replacement, hypertrophic cardiomyopathy or congenital heart disease.
In California, a total of 882 methods were analysed between 619 patients. The Californian patients showed smaller left atrial (LA) (p<0.0001), superior left ventricular function (p<0.0001) and less extreme comorbidity (p=0.0001), brought out a substantially decreased FLAME score (p<0.0001). They were, but consequently older (p=0.001), with substantially more hypertension (p<0.0001) and pulmonary disease (p=0.002), and had taken more antiarrhythmic drugs (p<0.0001) with the longer duration of follow-up (p<0.0001). For first ablation after follow-up of 2.1 years (median, IQR 1.0–4.1)), FLAME score: 0–1 predicts 62% success, 2–4 44% and ≥5 29% (ptrend <0.0001). (Table 1, Figure 1A and 2A). Following the final ablation (mean procedures: 1.4±0.6, follow-up 1.8 years (median, IQR 0.8–3.6)), FLAME score: 0–1 predicts 81% success, 2–4 65% and ≥5 44% (ptrend <0.0001). (Table 1, Figure 1B and 2B).
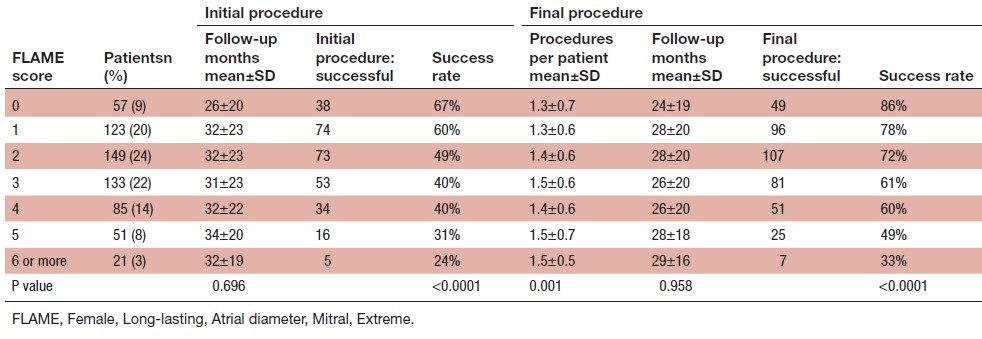
Table 1: Success rates and other variables by FLAME score in California

Figure 1: Outcome of ablation in California by FLAME Score group.
Kaplan-Meier curves describing freedom from recurrence of sustained atrial arrhythmia (by ECG or symptoms) following an initial (A) or final (B) ablation. Curves show FLAME score groups. FLAME, Female, Long-lasting, Atrial diameter, Mitral, Extreme.
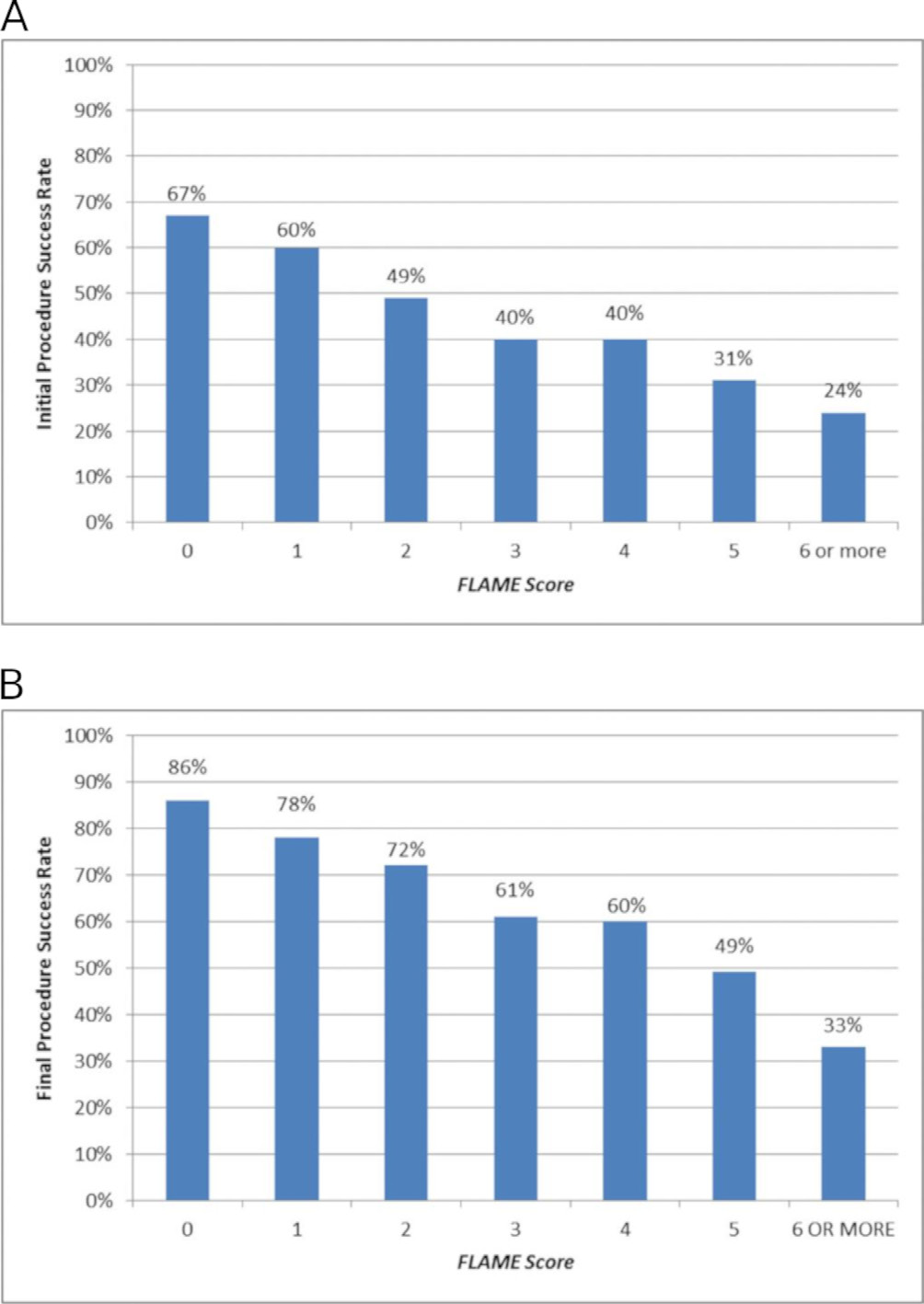
Figure 2: Success rate following the initial (A) and final (B) ablation in California by FLAME score. FLAME, Female, Long-lasting, Atrial diameter, Mitral, Extreme.
It was concluded that the FLAME score is easily measured from baseline clinical variables, was acquired from an examination of individual procedural outcomes of catheter ablation for persistent AF in London. It efficaciously differentiated the outcomes of first or multiple catheter ablations for persistent AF in California. Such a score may aid to superior advice for individual patients about the efficacy of catheter ablation for non-PAF.

