Liao H. Heart Rhythm. 2021 Jan;18(1):10-19.
Specific localization of the sources of LV ostium sites and an improved understanding of the optimal anatomical perspectives for effective ablation has the prospective to enhance outcomes, reducing the requirement for repeat processes. Multiple electrocardiographic patterns are used to vary left from right origins. Specific signatures for the region of the anterior LV ostium incorporating a qrS or notched pattern in leads V1-V3 are prognostic of sites of origin at the junction of the right and left coronary cusps in the aortic root and a R wave pattern break in lead V2 characterised an origin close to the anterior interventricular sulcus. Liao H, et al. conducted a study to report the prevalence, attributes, and outcomes of a new distinct electrocardiographic pattern of outflow tract ventricular arrhythmias (OTVA) with left bundle branch morphology and sudden transition in lead V3 (ATV3) that localizes to the septal margin of the LV summit. The anatomy of the right-left aortic interleaflet triangle (R-L ILT) is featured as an anatomic vantage point from the endocardial anterior LV ostium to reduce these refractory arrhythmias.
157 successive patients with premature ventricular contractions (PVCs) were assigned to the University of Chicago Medicine Center from Mar 2016 to Sept 2019 for Arrhythmia Care for detailed mapping and ablation, of which 78 successive patients assigned for catheter ablation of OTVA were evaluated. In a prospective UChicago VT Ablation Registry, all patients were given written informed consent and were enlisted. Standard 12-lead surface ECGs were recorded and evaluated. Precordial leads were affirmed in standard positions. The ATV3 pattern of OTVA was described as an R wave amplitude in V3 3 times higher as compared to that in V2 with a precordial transition at V3. This sudden transition was hypothesized to be due to activation in a posterior direction away from leads V1 and V2 with inferior and leftward activation directed toward V3 (Figure 1A).
The prevalence of ATV3, pattern break V2, and qrS pattern or notching in V1-V3 was analyzed. The V2 transition ratio, V3 transition ratio and QRS durations were calculated. Ablation was performed targeting the earliest endocardial activation site using a 4 mm open irrigated tip ablation catheter. In cases where great cardiac vein and anterior interventricular vein junction (GCV/AIV) was the earliest activation site, ablation was first attempted from the anatomically adjacent endocardial vantage point of the right-left aortic interleaflet triangle (R-L ILT). To target the R-L ILT, the catheter was prolapsed retrograde into the left ventricle and pulled back with a small curve positioned underneath the junction of the right and left commissure along the LV ostium, confirmed by fluoroscopy and intracardiac echocardiography (Figure 1B). Outpatient visits or telehealth visits were routinely performed 1, 3, 6 and 12 months after procedure. Twelve-lead electrocardiogram (ECG) and/or 24h Holter monitoring was recorded during follow-up.
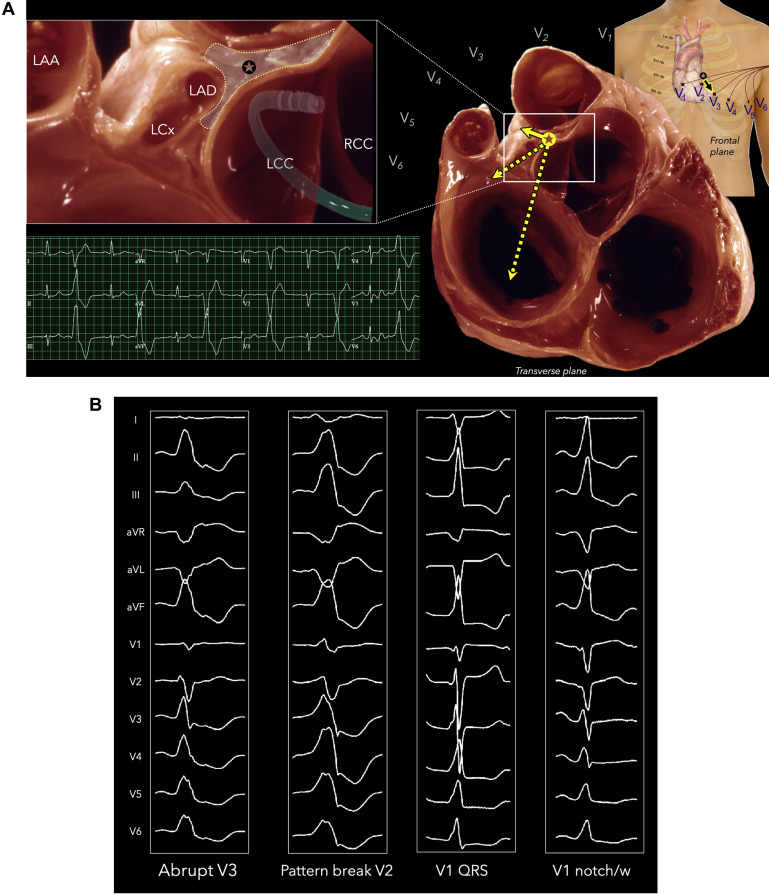
Figure 1A: Anatomic basis for vector orientation to produce ATV3 pattern. In the transverse plane, activation proceeds leftward toward V3, away from V1 and V2.
In the frontal plane, activation of the left ventricle proceeds inferiorly toward V3 as the septal margin of the LV summit is immediately posterior to V2. Catheter prolapsed underneath the R-L commissure adjacent to the septal margin of the LV summit. Adapted from Wallace A. MacAlpine; Courtesy of UCLA Cardiac Arrhythmia Center, with permission.
Figure 1B: Typical morphologies of abrupt V3 transition (ATV3), pattern break V2, qrS pattern in V1-V3, and presence of notching or w in V1
A total of 20 patients (26%) demonstrated an ATV3 pattern, representing 31% amongst those referred after failed ablation (FIGURE 2). The mean PVC burden in the ATV3 group was 23±17% and the mean EF was 48±12%. The remaining 58 patients were included as a control group. Overall 44 (57%) of OTVA patients previously had undergone at least one failed ablation and 65% of patients with ATV3 had prior failed ablation. There were more females within the ATV3 group than the control group. Amongst all 78 patients with OTVA, baseline sinus rhythm showed precordial transition at V1 in 8% V3 in 19%, at V4 in 54%, and at V5 in 9% patients. No intrinsic precordial transition was present in 10% (1 transition beyond V6, 3 RBBB, and 4 with permanent ventricular pacing). Only 1 patient in ATV3 and 1 patient in the control group exhibited an ATV3 pattern during intrinsic sinus rhythm activation.
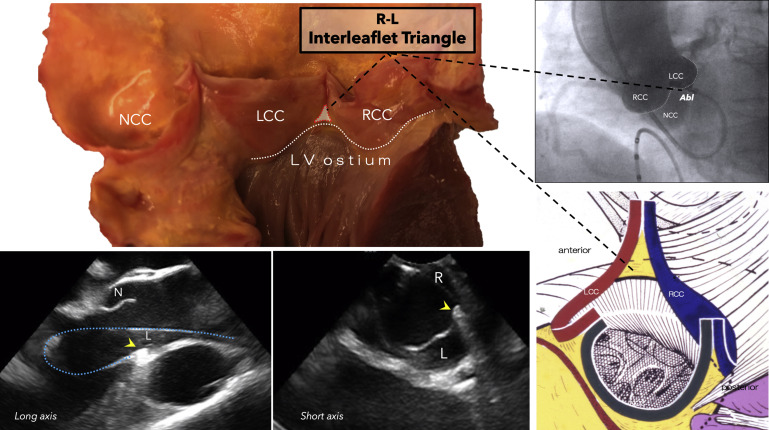
Figure 2: Anatomy of the aortic right-left interleaflet triangle and optimal catheter profile positioned on LAO fluoroscopy and intracardiac echocardiography
In the control group, PVCs with left bundle branch block (LBBB) morphology exhibited transition at V2 in 18%, V3 in 30%, V4 in 45%, V5 in 7% of the patients. Compared with the control group, R amplitudes in V1 and V2 and S amplitude in V3 were significantly lower in the ATV3 group. In VA with ATV3, the mean R wave in V2 of 0.22±0.15 mV, which transitioned abruptly to V3 amplitude of 1.45±0.67mV (6.6-fold increase in R wave from V2 to V3) (Figure 3).
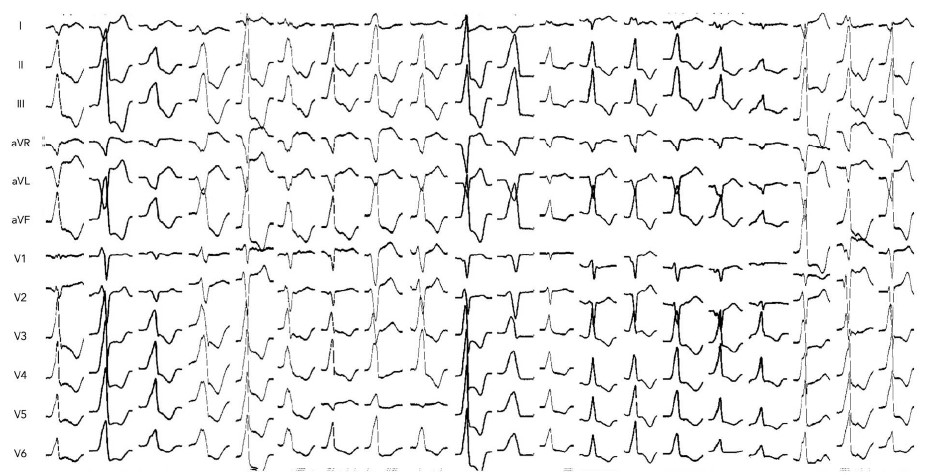
Figure 3: Twelve-lead surface ECGs of all 20 patients with OTVA exhibiting an ATV3 pattern
Pattern breaks V2, qrS pattern in V1-V3, and notch or w in V1 were more frequently seen in the ATV3 group than in the control group. No significant differences were observed in S amplitude in V1, V2 and R amplitude in V3, QRS duration and maximum deflection index (MDI) between two groups.
All the patients in the ATV3 group had acute procedural success with, 80% ablated from the RL ILT. (Figure 4). The ATV3 pattern showed higher sensitivity, specificity, predictive value, and accuracy than validated ECG criteria (notch or “w” pattern in lead V1, qrS pattern in leads V1 through V3, and pattern break V2) for predicting successful ablation in the region of the anterior LV ostium. At 12±11 months, freedom from ventricular arrhythmia recurrence was 89% and 82% in the ATV3 and control groups, respectively.
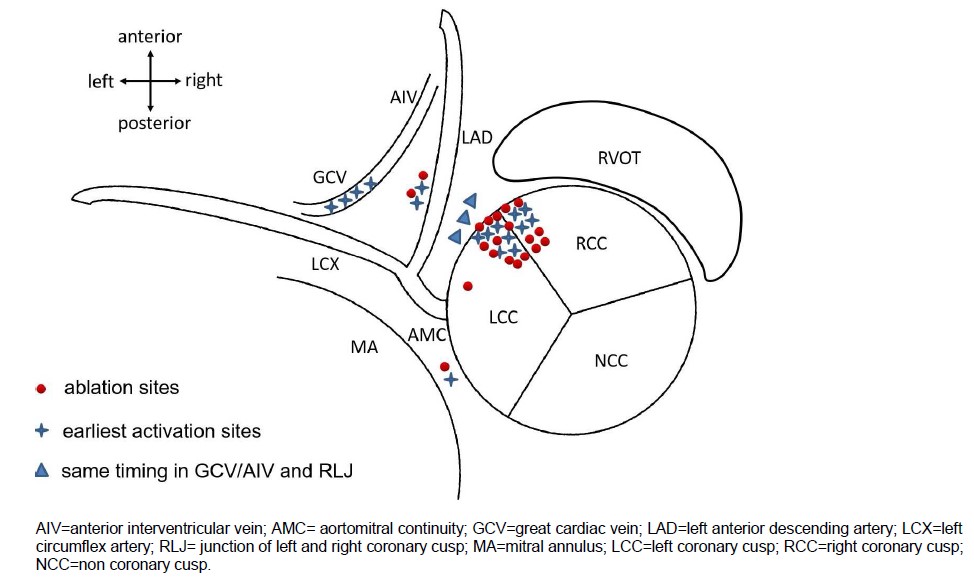
Figure 4: Location of the earliest activation sites and successful ablation targets of the ATV3 group
Thus, it was concluded that ATV3 is a new and simple electrocardiographic pattern observed in 26% of patients referred to a tertiary center for refractory OTVA ablation, indicative of a site of origin from the septal margin of LV summit. The endocardial vantage point of the R-L ILT at the LV ostium can be effective to eliminate OTVA with ATV3 that overwhelmingly exhibit earliest activation in the epicardium or midmyocardium. Test characteristics for ATV3 pattern were superior to established ECG signatures that have been validated for the anterior LV ostium.

