Safford MM. Circulation. 2021 Jan 19;143(3):244-253.
Coronary heart disease (CHD) inconsistencies are still present in the modern era, and social determinants of health (SDH) are progressively a focus of efforts to reduce these inconsistencies. SDH like low educational attainment, low income, social isolation, racism, suboptimal built environments, and obstacles to obtaining high quality healthcare have each been correlated with worse CHD effects. The contribution of SDH to health outcomes may prevail that of biological influences or medical care, still they are not consistently operationalized as definite risk markers in clinical care settings. Safford MM, et al., conducted a study to analyse the correlations of the number of SDH and fatal incident CHD and, separately, incident nonfatal myocardial infarction (MI). It was hypothesized that as the number of SDH rise, the risk of fatal incident CHD and nonfatal MI also elevate.
The REGARDS study was outlined to explain reasons for regional and racial differences in stroke mortality; CHD effects are being analysed via an ancillary study. A community-dwelling Black and white adults age >45 years living in the 48 contiguous US states in 2003-2007 were enlisted. Sampling targeted to balance on race and sex, with oversampling of the stroke and the stroke belt, regions with the greatest stroke mortality in the US. Participants were recruited by commercially available lists and gone through 45-minute computer assisted telephone interviews (CATI) regarding medical history, health behaviours, and risk factors followed by in-home visits at which physiologic parameters (height, weight, blood pressure) and electrocardiography were evaluated. Blood and urine samples were gathered. 7 SDH from the 5 healthy people 2020 domains incorporated social context (Black race, social isolation); education (educational attainment); economic stability (annual household income); neighbourhood (living in a zip code with high poverty); and healthcare (lacking health insurance, living in one of the 9 US states with the least public health infrastructure). In the two weeks, medications were taken before the study visit were recorded via pill bottle review, and a food frequency questionnaire was remained for self-administration. Participants were contacted every 6 months using telephone to diagnose potential study endpoints.
The primary outcome was fatal incident CHD, described as death within 28 days of an adjudicated precise or probable MI, or CHD or sudden death as the adjudicated cause of death. Heart-related hospitalizations or deaths diagnosed in follow-up activated medical record retrieval and adjudication of study endpoints by clinician experts with national guidelines. The secondary outcome was nonfatal MI.
Almost 22,152 individuals free of vascular disease at baseline were incorporated. Of 22,152, 58.8% were women, 42.0% were Blacks, 20.6% had no SDH, 30.6% had 1, 23.0% had 2, and 25.8% had >3 in the study sample. Over a cumulative 10.7-year follow-up [IQR 6.6— 12.7], there were 411 fatal CHD cases and 828 nonfatal MIs. There were 463 fatal incident CHD events and 932 nonfatal MIs over median 10.7 years [IQR 6.6-12.7]. Fewer SDH were correlated with nonfatal MI as compared to with fatal incident CHD. Fatal incident CHD per 1000 person-years was elevated with each additional SDH, with incidence over twice as high for those with >3 SDH (2.86/1000 person-years) as compared to those without SDH (1.30/1000 person-years) (Figure 1A). Participants with higher counts of SDH also showed successively decreased survival probability (Figure 2A, p<0.001). Non-fatal incident MI per 1000 person-years was elevated with each additional SDH; those with >2 SDH (5.44/1000 person-years) showed 39% greater incidence than those with no SDH (3.91/1000 person-years) (Figure 1B). Participants with higher counts of SDH also showed successively greater cumulative incidence of nonfatal MI (Figure 2B, p<0.001). Participants with higher counts of SDH showed higher risk for fatal incident CHD (Table 1). Comparing respondents with > 3 versus no SDH, crude HR was 2.78 (95% CI 2.07, 3.74). Having >3 versus no SDH was correlated with fully adjusted HR 1.50 (95% CI 1.09, 2.06) with p for trend <0.0001 for both minimally and fully adjusted models. Participants with greater counts of SDH showed higher risk for non-fatal MI (Table 1). Comparing participants with >2 versus no SDH, Crude HR was 1.577 (95% CI 1.30, 1.90). A graded correlation remained present following multivariable adjustment however was not statistically substantial (adjusted HR for >2 SDH vs. none 1.14; 95% CI 0.93, 1.41).
Thus, it was concluded that a higher burden of SDH was correlated with a graded increase in risk of incident CHD, with higher magnitude and independent correlations for fatal incident CHD. Computing the number of SDH may be a favourable approach that could be included into clinical care to recognize individuals at high risk of CHD.
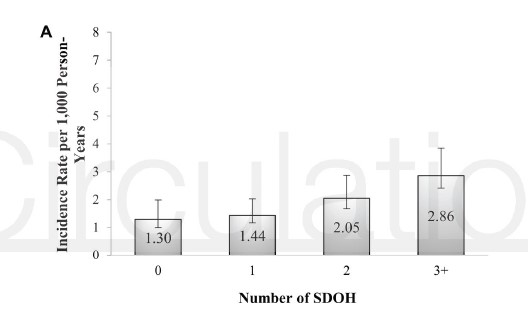
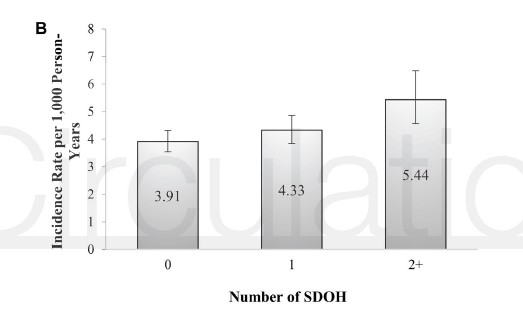
Figure 1: Age-adjusted Fatal Incidence of Coronary Heart Disease (A)* and Age-Adjusted Incidence of Nonfatal Myocardial Infarction (B)** per 1,000 Person-years, by Number of Social Determinants of Health*
*Social determinants for fatal incident coronary heart disease included Black race, low education, low annual household income, zip code with high poverty, residence in the worst ranked states for public health infrastructure, lack of health insurance, social isolation (saw no friends/family in the past month).
**Social determinants for incident nonfatal myocardial infarction included low education, low annual household income and lack of health insurance
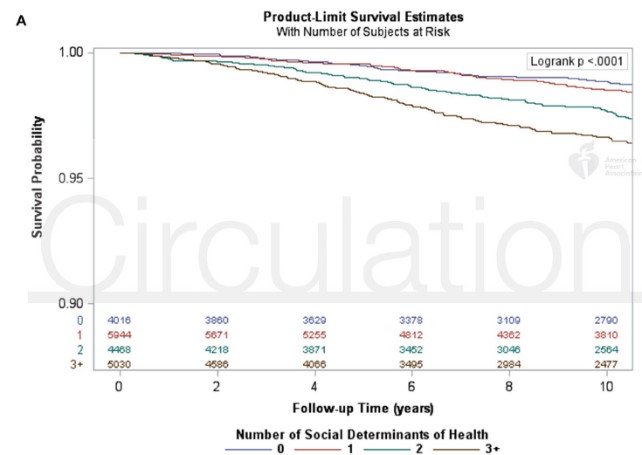
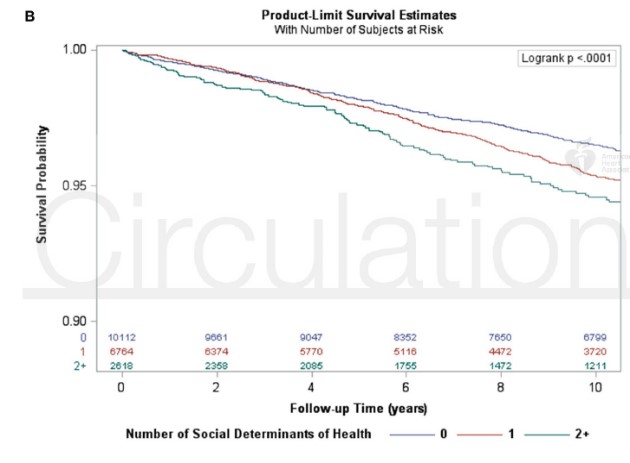
Figure 2: Kaplan-Meier Survival Curves by Number of Social Determinants of Health* and Fatal Incident Coronary Heart Disease (A)* and Incident Nonfatal Myocardial Infarction (B)**
*Social determinants for fatal incident coronary heart disease included Black race, low education, low annual household income, zip code with high poverty, residence in the worst ranked states for public health infrastructure, lack of health insurance, social isolation (saw no friends/family in the past month)
**Social determinants for nonfatal myocardial infarction include low education, low annual household income and lack of health insurance
Table 1: Number of Social Determinants of Health and Associations with Fatal Incident Coronary Heart Disease and Incident Nonfatal Myocardial Infarction
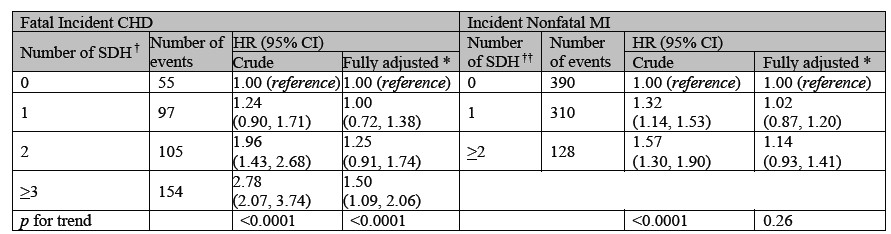
* Adjusted for sociodemographic factors, medical conditions, use of medications, functional status, health behaviours, and physiologic variables † SDOH included Black race, low education, low annual household income, zip code with high poverty, residence in the worst ranked states for public health infrastructure, lack of health insurance, social isolation (saw no friends/family in the past month). Note that not all available events are included in this table due to missing data on SDH; all events were used in modeling with multiple imputation. †† SDOH included low education, low annual household income and lack of health insurance CHD = coronary heart disease. CI = confidence interval. HR = hazard ratio. MI = myocardial infarction. SDH = social determinants of health

