Kubicki DM. JACC Heart Fail. 2020 Feb;8(2):122-130.
Heart failure (HF) endures a major public health complication despite significant advances in the prevention and treatment of cardiovascular disorder. The American Heart Association recognised seven modifiable risk factors, hypertension, diabetes mellitus, smoking, high cholesterol, high body mass index (BMI), physical underactivity, and poor diet, that significantly contribute to cardiovascular disorder. Most studies of HF risk factors have been held in primarily middle-income, white groups with comparatively low rates of HF. The relative contributions of adjustable risk factors to HF occurrence and whether these differ by race and sex have been understudied in high-risk low-income individuals. Thus, Kubicki DM, et al. conducted a study to analyse the risk of incident HF correlated with the seven adjustable risk factors, distinguished by race-sex group at the individual and population levels in the SCCS.
84,797 participants were enrolled, aged 40-79, nearly two-thirds black, living in 12 southeastern states from 2002 to 2009. 27,078 individuals aged ≥65 years (n=7,001) or <65 years were analysed and each race-sex group being covered by Centers for Medicare and Medicaid Services (CMS) on the baseline questionnaire. Data from participants’ enlistment questionnaires was used to estimate seven adjustable cardiovascular risk factors. HF occurrences were recognised via SCCS linkage with CMS Research Identifiable Files and by using an International Classification of Diseases, 9th revision (ICD-9) code of 428.x in the Medicare institutional. Participants were classified into four race-sex groups, as black male, black female, white male, and white female. A multivariable-adjusted Cox proportional hazards models with robust variance was used to analyse the risk of incident HF correlated with each of the seven adjustable risk factors. Evaluations were repeated after excluding participants with a history of MI or CABG at baseline. Analyses were executed using R or Stata v.13.0.
Most participants were overweight or obese and physically underactive and had hypertension. Other risk factors were also common such as diabetes, high cholesterol, and smoking present in 26.5%, 39.5%, and 43.4% of participants, resp. Almost 99% of participants had one or more of the seven adjustable risk factors, with a median number of 3. 4,341 (16.0%) participants generated HF over a median follow-up of 5.2 years. The aggregation of adjustable risk factors correlated with elevating HF risk, with a 27% increase (95% CI: 24% to 30%) with every additional risk factor. (Figure 1)
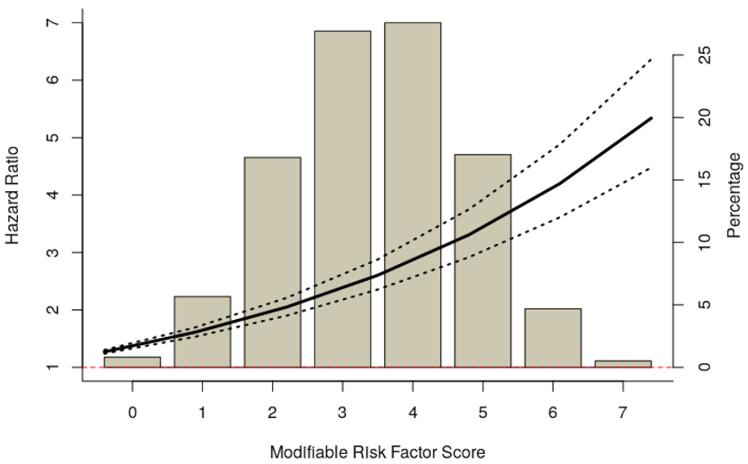
Figure 1: Distribution of Risk Factor Scores and Cumulative Risk of Heart Failure Associated with Risk Factor Score
Hypertension and diabetes were correlated with the highest risks for HF overall, with HRs of 1.69 (95% CI: 1.56 to 1.84) and 1.70 (95% CI: 1.59 to 1.82), resp. In an analysis of the individual seven adjustable factors, hypertension and diabetes were the only adjustable factors substantially correlated with HF risk between black men and women in analyses by race-sex groups. (Figure 2)
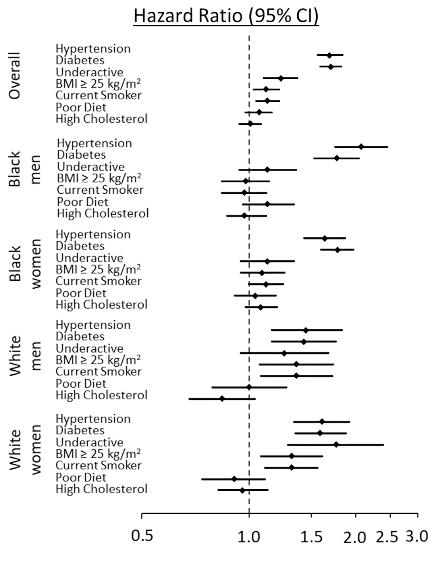
Figure 2: Association of Modifiable Risk Factors and Incident Heart Failure, Overall and by Race-Sex Group
Hypertension and diabetes contributed substantially to the population burden of HF in all race-sex groups, and these were the only risk factors with significant PARs between black participants. Hypertension had the greatest PAR as compared to other risk factors, 40.7% (95% CI: 32.6% to 47.8%) in black men and 31.8% (95% CI: 24.1% to 38.8%) in black women. In white men and women, high BMI was considered for a substantial proportion of the population risk for HF, with respective PARs of 20.9% (95% CI: 4.8% to 34.2%) and 19.5% (5.5% to 31.4%) resp. Smoking also had substantial PARs of 11.9% (95% CI: 3.0% to 19.9%) and 9.7% (95% CI: 3.5% to 15.6%), respectively in white men and women. Physical underactivity was substantial only in white women, with a PAR of 40.2% (95% CI: 20.4% to 55.1%).
It was concluded that contributions of risk factors to HF differed, especially by race in this high-risk low-income group and interferences adapted for specific race and sex groups may be warranted to decrease the population burden of HF.
SCCS: Southern Community Cohort Study; MI: Myocardial infarction; CABG: Coronary artery bypass graft; PAR: Population attributable risk; CI: Confidence interval; HR: Hazard ratio

