DEFINE-FLOW: An Observational Study of Deferred Lesions After FFR and CFR Assessment
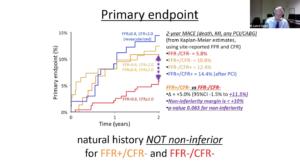
Johnson N, presented findings of the DEFINE-FLOW trial at the TCT Connect 2020 virtual conference. In the current age, the role of invasive coronary flow reserve (CFR) assessment remains unclear, as fractional flow reserve (FFR) has become a reference norm guiding revascularization decisions. While observational data from invasive and non-invasive tools have shown that intact CFR lesions perform well, few of these studies simultaneously evaluated FFR. Researchers designed and conducted the DEFINE-FLOW analysis to overcome the shortcomings of the existing literature.
Out of 12 sites in six countries, a total of 455 patients were registered. Of those enrolled, 430 patients (533 lesions) underwent protocol treatment and two years of follow-up. Stable coronary lesions were determined simultaneously in at least duplicate FFR and CFR with central core laboratory analysis of the tracings. According to a standardized protocol, treatment adopted local measurements, whereby only lesions with both FFR 0.8 and CFR < 2.0 underwent percutaneous coronary intervention (PCI). All other combinations, including FFR ≤ 0.8 but intact CFR > 2.0, received initial medical therapy. The composite of all-cause death, myocardial infarction, and revascularization at two years was the primary endpoint. The study findings for MACE were 5.8% for FFR-/CFR-, 10.8% for FFR+/CFR-, 12.4% for FFR- /CFR+, and 14.4% for FFR+/CFR+ (after PCI). The difference between FFR+/CFR- and FFR-/CFR- was 5.0% (95% CI -1.5% to +11.5%, p-value 0.065 for non-inferiority). The analysis therefore found that vessels with irregular FFR ≤ 0.8 but intact CFR ≥ 2.0 had no non-inferior results relative to FFR > 0.8 and CFR ≥ 2.0 when treated medically.
Conclusion: Natural history of FFR ≤ 0.8 / CFR ≥ 2 is not non-inferior to lesions with FFR > 0.8 / CFR ≥ 2.
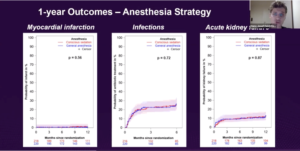
SOLVE-TAVI: One-Year Outcomes of a Factorial Randomized Trial of Self-expandable vs Balloon-expandable TAVR and General vs Local Anesthesia
Feistritzer HJ, presented findings of the SOLVE-TAVI trial at the TCT Connect 2020 virtual conference. As a proven treatment technique for patients with symptomatic aortic stenosis, transcatheter aortic valve implantation (TAVI) has emerged. Present developments of valves are aimed at solving prior limitations such as suboptimal deployment, disruptions of conduction, and paravalvular leakage. A comparison of newer generation self-expandable (SEV) and balloon-expandable valves (BEV) demonstrated equivalence in the short-term follow-up of the SOLVE-TAVI trial. The clinical outcome data at 1-year follow-up was reported in this study. In the randomised, multicenter, 2×2, open-label SOLVE-TAVI trial, 447 patients with severe, symptomatic aortic stenosis were randomly assigned to transfemoral TAVI using either BEV (Edwards Sapien 3, Edwards Lifesciences, Irvine, California) or SEV (CoreValve Evolut R, Medtronic Inc., Minneapolis, Minnesota) as well as general and local anaesthesia. For clinical outcome assessment and echocardiographic valve function evaluation, patients were followed-up for 1 year. At 1-year follow-up, rates of all-cause death (17.0% vs. 17.6%; HR 0.96, 95% CI 0.60 to 1.55), cardiovascular death (1.8% vs. 0.5%; HR 3.89, 95% CI 0.44 to 34.67), moderate or severe prosthetic valve regurgitation (4.5% vs. 7.0%; HR 0.63, 95% CI 0.27 to 1.45), and permanent pacemaker implantation (20.2% vs. 24.7%; HR 0.79, 95% CI 0.53 to 1.16) were similar between the BEV and SEV group. Higher stroke rates were seen in BEV treated patients (6.9% vs. 1.0%; HR 7.13, 95% CI 1.62 to 31.32). Mean aortic valve gradients were 10 (interquartile range [IQR] 8 to 12) mmHg in BEV and 6 (IQR 4 to 8) mmHg in SEV treated patients.
Conclusion: Similar composite endpoint rates of all-cause death, stroke, moderate / extreme PVL, and permanent pacemaker implantation, was seen in symptomatic patients with severe aortic stenosis undergoing transfemoral TAVR when newer generation SEV was compared to BEV. Besides, higher stroke rates in BEV-treated patients and similar time-related safety according to the VARC-2 criteria-lower aortic gradients were seen in SEV-treated patients.
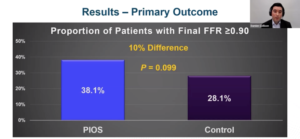
TARGET FFR: A Randomized Trial of Physiology-Guided PCI Optimization
Collison D, presented findings of the TARGET FFR trial at the TCT Connect 2020 virtual conference. Trial of Angiography versus pressure-Ratio-Guided Enhancement Techniques (TARGET) FFR was an investigator-initiated, single-center, randomized controlled trial. This trial tested the hypothesis that Application of a Physiology-guided Incremental Optimization Strategy (PIOS) can increase the proportion of patients achieving a final post-PCI FFR ≥0.90 by 20%. 260 patients after ensuring angiographically successful PCI procedures were randomized 1:1 to either the PIOS intervention group or a blinded control group. The trial’s primary endpoint was defined as the proportion of patients with a final post-PCI FFR result ≥ 0.90. The study found that in the PIOS group, the incidence of final FFR ≥ 0.90 was 10% higher than in the control group, but that the difference was not statistically significant (38.1% vs. 28.1%, p=0.099). In the PIOS group, however, the secondary endpoint of the study, the percentage of patients with final FFR ≤ 0.80, was slightly lower (18.6 % vs. 29.8 %, p=0.045). Based on the FFR pullback assessment of the stented vessel, 60 of the 131 (46%) patients randomised to PIOS had a target for further optimization, and operators found it necessary to conduct additional post-dilatation + /- stenting in 40 of these 60 (66%) patients. Mean post-PCI FFR increased significantly from 0.76 to 0.82 (p<0.001) and mean coronary flow reserve (CFR) increased from 3.0 to 4.0 (p=.02) among patients who had further intervention / optimization performed.
Conclusion: Application of an FFR-guided optimization strategy after stenting led to improvements in both FFR and CFR and significantly reduced the proportion of patients with a final post-PCI FFR ≤ 0.80.
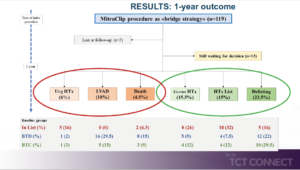
MITRABRIDGE: Outcomes of MitraClip Treatment as Bridge Therapy to Heart Transplantation
Godino C, presented findings of the MITRABRIDGE trial at the TCT Connect 2020 virtual conference. In order to minimise the deterioration and worsening of the underlying condition, patients undergoing heart transplantation (HTx) frequently require bridging therapies. There is minimal evidence available on the use of the MitraClip treatment for this clinical condition in secondary mitral regurgitation. The authors examined 119 patients (median age: 58 years) with moderate-to-severe or severe secondary mitral regurgitation and advanced heart failure (HF) (median left heart failure) (median left heart failure) in an international, multicenter (17 centres) registry according to 1 of the following criteria: (1) patients active on HTx list (in list group) (n = 31); (2) patients suitable for HTx but awaiting clinical decision (bridge to decision group) (n = 54); or (3) patients not yet suitable for HTx because of potentially reversible relative contraindications (bridge to candidacy group) (n = 34). In 87.5 % of cases, procedural success was achieved, and 30-day survival was 100 %. Kaplan-Meier estimates of freedom from the composite primary end point (death, urgent HTx or implantation of left ventricular assist system, first HF rehospitalization) were 64 % at 1 year. 15 % of patients underwent elective transplantation at the time of the last available follow-up (median: 532 days), 15.5 % remained or could be included on the HTx waiting list, and 23.5 % were no longer recommended for HTx due to clinical improvement.
Conclusion: In patients with advanced HF with severe mitral regurgitation, the MitraClip procedure as a bridge strategy to HTx was safe and two thirds of patients remained free of adverse events at 1 year of age. To direct further research for percutaneous intervention in high-risk patients with advanced HF, these results should be considered exploratory and hypothesis generating.
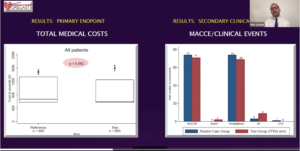
FORECAST: A Randomized Trial of CTA/FFRCT Decision-making in Patients with Chest Pain
Curzen N, presented findings of the FORECAST trial at the TCT Connect 2020 virtual conference. The objective of the FORECAST trial was to determine whether, in a population of patients presenting to Rapid Access Chest Pain Center in the UK, routine fractional flow reserve management derived from computed tomography (FFRCT) as a default test is superior in terms of resource utilization, when compared with routine clinical pathways algorithms recommended by NICE CG95. This was a randomized control trial where 1400 patients were randomized to the reference group also the routine care group and the test group also the CTCA+FFRCT group. 0.4% of patients in the reference group had previous MI compared to 0.7% in the test group. The primary endpoint of the FORECAST trial was resource utilization derived from non-invasive cardiac tests, invasive angiography, coronary revascularization, hospitalization for a cardiac event, and cardiac medications at nine months. Prespecified secondary endpoints included major adverse cardiac and cerebrovascular events, revascularization, angina severity, and quality of life (QOL). The 9 months tests and revascularization showed 14% lower total invasive coronary angiography (ICA) seen in the test group vs. the reference group (p=0.02) and 22% fewer patients had ICA in the test group vs. the reference group. In patients with new onset stable chest pain, the FFRCT CTCA strategy did not substantially reduce the overall total costs in the NHS system compared with the routine care strategy (£1,605.50 vs. €1,491.46, p=0.962). The number of patients performing the following non-invasive tests in the test arm at nine months was: CTCA (674), FFRCT (220), stress echo (13), perfusion scan (4), MRI stress (15), ECG exercise (27). The number of patients in the reference arm who underwent these tests was: CTCA (460), FFRCT (9), stress echo (124), perfusion scan (34), stress MRI (20), and exercise ECG (99).
Conclusion: In patients presenting with new onset stable chest pain, a strategy of CTCA with FFRCT when compared to routine care did not considerably reduce costs in the NHS system and is associated with notably lower rate of ICA and is not associated with significantly different rate of MACCE or revascularization.
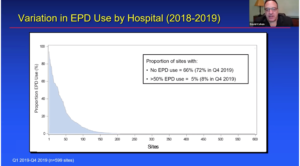
STS/ACC TVT Registry: Cerebral Embolic Protection and TAVR Outcomes
Cohen DJ, presented findings of the STS/ACC TVT Registry at the TCT Connect 2020 virtual conference. A debilitating complication remains stroke after transcatheter aortic valve replacement (TAVR), which has persisted through procedure refinements and improved operator experience. Although cerebral embolic protection devices (EPDs) were designed to mitigate this risk, there is limited evidence on the effect of EPDs on stroke and other outcomes after TAVR. This was an observational study, which used data from the STS/ACC TVT registry to examine the association between EPD use and TAVR outcomes. The research included consecutive adults at hospitals conducting > 20 TAVR procedures / year who underwent elective or urgent transfemoral TAVR between July 2017 and December 2019. In-hospital stroke was the primary result. In-hospital death or stroke, in-hospital stroke or TIA, in-hospital death, effectiveness of the TAVR system, 30-day mortality, and 30-day stroke were secondary outcomes. The authors analysed temporal patterns in the proportion of EPD sites and procedures, as well as site-level variance in the proportion of sites and procedures used. The association between EPD use and clinical outcomes was also evaluated using 2 complementary techniques: (1) instrumental variable (IV) analysis with site-level preference for EPD use as the instrument; and (2) a propensity-score based comparison using inverse probability of treatment weighting. IV analysis is an econometric technique that can account for both measured and unmeasured confounding in observational studies. Over time, the use of EPD during TAVR increased, reaching 28 % of sites and 13 % of all TAVR procedures by December 2019. There was a wide variance in the use of EPD across hospitals, with 8.3 % of sites performing > 50 % of TAVR procedures with an EPD and 71.8 % in the last quarter of 2019 performing no cases with an EPD. The baseline characteristics of patients treated with or without EPD were identical, while hemodialysis and morphology were less likely to occur in patients who received EPD, they were less likely to be on hemodialysis and more likely to have had a bicuspid valve, received conscious sedation during TAVR, and to have been treated at a higher volume TAVR center.
Conclusion: Use of EPD was generally safe, with no evidence of increased vascular complications, major bleeding, or device failure. There was no significant reduction in in-hospital or 30-day mortality rates. Nonetheless, both the secondary (propensity-weighted) analysis and the CI for the primary analysis are consistent with a possible modest reduction in stroke (~20% RRR, NNT ~300 for major stroke).
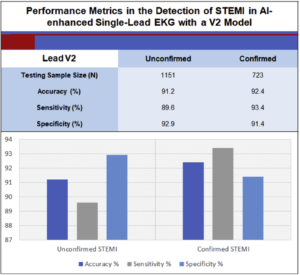
Artificial Intelligence Single Lead ECG as a Blueprint for Symptom-to-Balloon Time Reduction
Decreasing door-to-balloon time has demonstrated a favourable strategy for enhancing in-hospital ST-segment elevation myocardial infarction (STEMI) care, still pre-hospital management remains sluggish as patient’s disease perception and initiative to look for care yet limits the advantages of early therapy. Thereby, an attractive key is use of portable artificial intelligence-driven single-lead electrocardiogram (ECG) technology. Mehta S, presented a study at TCT Connect 2020 virtual conference which explored this artificial intelligence single lead ECG as a blueprint for the time reduction of symptom-to-balloon. During April 2014 to December 2019, total 11,567 12-lead ECG records were obtained from the Latin America Telemedicine Infarct Network database. The database incorporated unconfirmed and angiographically confirmed STEMI, branch blocks, nonspecific ST-T changes, normal, and abnormal (remaining 200+ CPT codes). Cardiologist annotations assured accuracy. First and last 250 samples were removed to inhibit a standardization pulse. Ascertained classes were “STEMI” and “non- STEMI.” A 1-D convolutional neural network was instructed and assessed for each lead with a dataset proportion of 90/10, respectively. The last dense layer delivered output as STEMI or non-STEMI. The model was copied with another data subset excluding unconfirmed STEMI data for control purposes. Performance metrics are outlined for the best lead on each experiment. Unconfirmed STEMI showed accuracy of 91.2%, sensitivity with 89.6% and specificity of 92.9%. Confirmed STEMI showed accuracy of 92.4%, sensitivity with 93.4% and specificity of 91.4%.
Conclusion: Efforts to compatibly enhance the tried and tested AI-guided single lead ECG algorithm continuously showed auspicious outcomes. This algorithm’s execution and dependability will continue to be examined for future clinical validation as a prospective remote monitoring device.
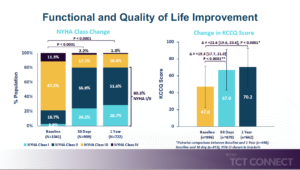
GLOBAL EXPAND: One-Year Outcomes with Third Generation MitraClip NTR and XTR Systems
Kar S, presented findings of the GLOBAL EXPAND trial at the TCT Connect 2020 virtual conference. To evaluate contemporary real- world clinical outcomes in subjects treated with the MitraClip NTR and XTR Systems, the EXPAND study was initiated. EXPAND is a prospective, multi-center, worldwide, single-arm study enrolling patients with mitral regurgitation (MR, both main and secondary) severity > 3 + in 57 centres in Europe and the United States (US). Topic follow-up is conducted at 30 days and 12 months per care protocol. To analyse all echocardiograms, an independent echocardiographic core laboratory (ECL) was used. Study outcomes included: MR severity, the occurrence of major adverse events (all-cause death, myocardial infarction, stroke, or non-elective cardiovascular surgery for device related complications) and procedural outcomes. Between April 2018 and March 2019, 1041 patients were registered with EXPAND. The patients were 77.3 ± 9.7 years old, 55% male, 61% in Europe and 39% in the US. The baseline STS predicted risk for mortality score was 6.3 ± 6.3% for repair and 8.0 ± 6.4% for replacement. The majority of subjects (78.5 % in NYHA functional class III or VI) with a baseline KCCQ score of 47 ± 24 were symptomatic. One MitraClip unit was used to treat 55 % of participants, 40 % with two clips and an average mean of 1.5 ± 0.6 clips per subject. Significant MR reduction from baseline through 1 year was maintained; Trace MR was achieved in 18.9%, MR ≤ 1+ was achieved in 89.2% and MR ≤ 2+ was achieved in 97.3% at 1 year follow up. At 1 Year MR reduction to ≤ mild maintained in 84.5% and 93% subjects in primary and secondary MR respectively. The 1-year all-cause mortality rates were 14.9% in the All EXPAND group (n=1041), 12.5% in the Primary MR patients (n=422) and 17.7% in the Secondary MR patients (n=413).
Conclusion: This analysis reflects the first contemporary 1-year results associated in patients with both primary and secondary MR treated with the third generation MitraClipTM NTR and XTR Systems. Results suggest that MR ≤1+ is being achieved more frequently with the third generation MitraClipTM (compared to prior generations) that is maintained at 1 year. Important reductions in MR have been associated with persistent improvements in the quality of life and symptoms of heart failure after 1 year. The implementation of extra clip size, XTR and delivery system enhancements resulted in a greater decrease in MR without an increase in adverse events.
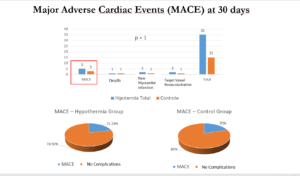
Cooling as an Adjunctive Therapy to Percutaneous Intervention in Acute Myocardial Infarction: COOL-MI InCor Trial
Endovascular therapeutic hypothermia (ETH) decreases the damage caused due to post-ischemia reperfusion injury syndrome in cardiac arrest; but, its role in ST-segment elevation myocardial infarction (STEMI) remains contentious. Dallan LA, presented a study at TCT Connect 2020 virtual conference which explored the safety, viability and 30-day efficiency of ETH as adjunctive treatment to percutaneous coronary intervention (PCI) in STEMI patients. Patients within 6 h of angina onset, with anterior/inferior STEMI eligible for PCI were enrolled in this prospective, controlled, randomized, interventional trial. Patients were randomized to hypothermia group (primary PCI + HT) or control group (primary PCI) in 4:1 ratio. Primary safety outcomes were 1) door-to-balloon (DTB) delay; and 2) major adverse cardiac events (MACE) at 30 days. The primary outcomes of efficacy were infarct size and left ventricular ejection fraction (LVEF) at 30 days. In total, 50 patients were included in which 35 (70%) patients were randomized to the hypothermia group and 15 patients (30%) to the control group. All 35 patients tried ETH (100%) exhibited successful cooling, with mean endovascular coronary reperfusion temperature of 33.1 ± 0.9ºC. The mean ischemic time was 375 ± 89.4 min in the hypothermia group and 359.5 ± 99.4 min in the control group. The mean DTB was 92.1 ± 20.5 min in the hypothermia group and 87 ± 24.4min in the control group. The absolute difference of 5.1 min was not analytically substantial (p =0.509). MACE rates were similar among both groups (21.7% vs. 20%, respectively; p = 0.237). No analytically substantial differences were observed at 30 days among mean infarct size (13.9 ± 8% vs. 13.8 ± 10.8%, respectively; p = 0.801) or mean final LVEF (43.3 ± 11.2% vs.48.3 ± 10.9%, respectively; p = 0.194) in the comparison among the hypothermia and control groups.
Conclusion: Hypothermia as a supportive treatment to primary PCI in STEMI is viable and can be applied without delay in coronary reperfusion. Hypothermia was safe concerning the occurrence of MACE at 30 days. However, the hypothermia group showed a greater occurrence of arrhythmia and in-hospital infection, with no increase in mortality. Concerning effectiveness, there was no difference in infarct size or LVEF at 30 days that would advocate additional myocardial protection with ETH.
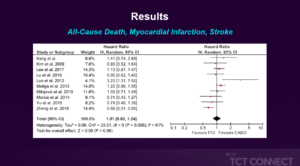
Percutaneous Coronary Intervention Versus Coronary Artery Bypass Grafting for Left Main Coronary Artery Disease in Diabetic Patients: A Meta-Analysis
In appropriate patients, percutaneous coronary intervention (PCI) of the left main (LM) coronary artery is arising as a feasible option to coronary artery bypass grafting (CABG). Nevertheless, there are restricted data comparing these 2 approaches for LM disorder in diabetic patients. Kim J, presented a meta-analysis report at TCT Connect 2020 virtual conference which analysed the current data for this subgroup of patients. A systematic search of database was executed from the PubMed for studies outlining outcomes of PCI with drug-eluting stents versus CABG for LM disorder in diabetic patients. Hazard ratios (HRs) with 95% CIs were obtained by random effects model. 4 randomized controlled trials and 8 observational studies met inclusion criteria with 2,456 patients incorporated in the PCI group and 2,776 patients in the CABG group. The average outlined follow-up time was 4.0 years (range: 2.1 to 7.1 years). There was no difference between PCI and CABG with concerns to the composite endpoint of all-cause death, myocardial infarction, and stroke (HR: 1.01; 95% CI: 0.82 to 1.24). Moreover, all-cause death (HR: 1.12; 95% CI: 0.92 to 1.36) and cardiovascular death (HR: 1.57; 95% CI: 0.69 to 3.55) did not vary between the 2 groups. The occurrence of stroke was lower with PCI (HR: 0.37; 95% CI: 0.23 to 0.62). There was enhanced rate of major adverse cardiac and cerebrovascular incidents, described as the composite of all-cause death, myocardial infarction, stroke, and repeat revascularization, in the PCI group (HR: 1.28; 95% CI: 1.11 to 1.48) and an enhanced rate of repeat revascularization with PCI (HR: 2.98; 95% CI: 2.02 to 4.41).
Conclusion: PCI and CABG were similar with concerns to all-cause mortality and the composite endpoint of all-cause death, myocardial infarction, and stroke. Although PCI showed a lower rate of stroke, there was an enhanced rate of major adverse cardiac and cerebrovascular occurrences seen with PCI than CABG which was predominantly managed by elevated rate of repeat revascularization. These consequences assist the concept that, in selective diabetic patients, PCI is a feasible option to CABG for LM disorder.
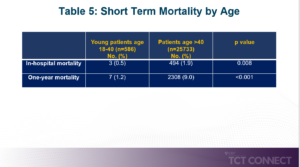
Clinical Profile and Mortality in Young Patients with Acute Myocardial Infarction
Coronary artery disease (CAD) firstly arises in patients across the age of 40, but it is now seen as an emerging issue in the younger population. It is significant to characterize myocardial infarction in the young population because of its destructive and long-term results. The classic demonstration of worsening angina is rare and most patients are shown as Non- ST elevation myocardial infarction. Coronary angiography commonly discloses single vessel disorder. In-hospital and short-term outcomes are normally beneficial in the younger population as compared to the patients > 40. Nadadur M, presented a study at TCT Connect 2020 virtual conference which analysed the clinical characteristics and short-term outcomes of young patients age 18 to 40 years vs. patients > 40 years of age hospitalized for myocardial infarction. In this retrospective observational cohort study, consecutive patients who underwent cardiac catheterization for acute myocardial infarction between 2006 and 2016 in an integrated health care system in Southern California were enrolled. Among patients aged 18 to 40 years and patients aged >40 years, clinical characteristics, length of stay, in-hospital mortality, and 1-year mortality were compared. A total of 26,319 patients underwent cardiac catherization for acute myocardial infarction, of which 586 (2.2%) patients were aged 18 to 40 years. A majority proportion of young patients were men (76.8% vs. 68.2%; p < 0.001), were from racial/ethnic minority groups (68.2% vs. 43.5%; p < 0.001), and showed low annual household income <$45,000 per year (32.6% vs. 25.4%; p < 0.001). Young patients were more probably to be active smokers (14.9% vs. 11.7%; p < 0.023). Prevalence of comorbidities including hypertension, hyperlipidemia, diabetes, heart failure, stroke, and renal failure was decreased in young patients. Young patients exhibited lower length of stay (1.8 ± 4.7 days vs. 2.7 ± 6.1 days; p < 0.001). Younger patients showed substantially lower in-hospital mortality and 1-year mortality (in-hospital mortality: 0.5% vs. 1.9%; p = 0.008; 1-year mortality: 1.2% vs. 9.0%; p < 0.001).
Conclusion: Young patients with acute myocardial infarction were more probably to be men, from racial/ethnic minority groups, and showed low household income. Inhibitory measures targeting these populations have the prospective to inhibit premature cases of myocardial infarction.
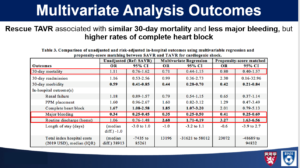
Transcatheter versus Surgical Aortic Valve Replacement in Acute Cardiogenic Shock
Cardiogenic shock secondary to decompensated aortic stenosis (AS) indicates a poor prognosis. A restricted data is available concerning optimal therapy strategy. Studies have exhibited correlation with greater 30-day and 1-year mortality in urgent/emergent transcatheter aortic valve replacement (TAVR) compared with elective TAVR. Nevertheless, in-hospital mortality was substantially lower as compared to TVT Registry predicted model. Till now, there is no direct comparison between SAVR and TAVR in the setting of acute cardiogenic shock. Trager L, presented a study at TCT Connect 2020 virtual conference which analysed outcomes of TAVR as rescue treatment by surgical aortic valve replacement (SAVR) as a benchmark based on a population-based, nationally representative investigation. All adult patients with AS and cardiogenic shock who underwent emergent/urgent TAVR or SAVR were recognised by the 2016 to 2017 Nationwide Readmission Database (NRD). Baseline characteristics were gathered, and outcomes were analysed with multivariate analysis and propensity score matching (1:1). In total, 804 patients were enrolled in a study of which 420 patients underwent SAVR and 384 patients underwent TAVR. Before matching, TAVR patients were older (77 vs. 64; p < 0.001) and showed a greater comorbid burden. Following matching (n = 129), TAVR showed similar 30-day mortality (16.3% vs. 18.6%; p = 0.623) and was correlated with substantially lower 30-day morbidity (87% vs. 77%; p = 0.04), less major bleeding (60% vs. 40%; p = 0.001), and more routine home discharges (31% vs. 14%; p = 0.001). In multivariate analysis, TAVR was correlated with similar 30-day mortality (odds ratio [OR]: 0.71; 95% confidence interval [CI]: 0.44 to 1.15) and less major bleeding (OR: 0.35; 95% CI: 0.25 to 0.50), however greater rates of complete heart block (OR: 1.85; 95% CI: 1.07 to 3.20) was observed.
Conclusion: Rescue TAVR may confer similar outcomes to SAVR in this high-risk population with severe AS and cardiogenic shock. TAVR should be a part of the armamentarium in managing critically ill patients.