Huang T. JACC. 2020 Mar;75(9):991-99.
The cardiovascular system showed strong circadian rhythms to retained normal functioning. Irregular sleep schedules, specified by high day-to-day irregularity in sleep period or timing, may show milder however chronic disturbance of the circadian clock that is broadly pertinent over the population. Particularly, individuals who commonly modify their sleep period or sleep timing on a night-to-night basis may have greater cardiometabolic risk because of disturbed circadian functions. An actigraphy was used across several days to estimate sleep timing and duration over multiple nights for evaluation of sleep regularity. Greater irregularity in sleep duration or timing is correlated with unfavourable metabolic profiles, such as higher blood pressure, dysregulated blood lipids, and insulin resistance. Since these adverse metabolic factors are precursors and strong forecasters for CVD, irregular sleep may enhance CVD risk via affecting metabolic health, in addition to its direct effect on the inherent rhythmicity of the cardiovascular system. The general population showed irregular sleep schedules, characterized by high day-to-day irregularity in sleep duration or timing and represent possibly milder however much more common and chronic disturbance of circadian rhythms as compared to shift work. Thus, Huang T et al., conducted a prospective study to analyse the correlation among sleep regularity and risk of cardiovascular disease (CVD).
The data was collected from the MESA (Multi-Ethnic Study of Atherosclerosis) group, a prospective study of clinical and subclinical risk factors for the development of atherosclerosis. 6,814 white (38%), African American (28%), Hispanic (22%), and Chinese American (12%) participants aged 45 to 84 years who were free of clinical CVD were enlisted from 6 field centers across the United States in 2000 to 2002. Participants wore the Actiwatch Spectrum wrist actigraph on their nondominant wrist for 7 continuous days, while also displaying their sleep and wake times in the following sleep diary. 2 SD measures were considered to estimate sleep regularity: 1) 7-day SD in sleep duration; and 2) 7-day SD in sleep-onset timing. Incident cardiovascular occurrences were recognised by telephone interviews held every 9 to 12 months as well as at each MESA follow-up analysis. The primary endpoint was incident total CVD events, which incorporated myocardial infarction, CHD death, resuscitated cardiac arrest, angina followed by revascularization, stroke, stroke death, and other atherosclerotic or CVD deaths. The secondary endpoint was the occurrence of a hard CVD effect that comprised of fatal and nonfatal CHD and stroke. Cox proportional hazards regression was used to analyse HRs and 95% CIs for occurrence CVD in association to quantify sleep regularity.
786 (39.5%) patients showed sleep duration SD of >90 min and 510 (25.6%) had sleep-onset timing SD >90 min from 1,992 MESA participants. A total of 111 incident total CVD occurrences arose after a median follow-up of 4.9 years (including 35 myocardial infarctions, 16 CHD deaths, 30 strokes, 17 other coronary events, and 13 other atherosclerotic or CVD deaths), providing an overall occurrence rate of 11.8 per 1,000 person-years. In unadjusted analysis, after adjustment for CVD risk factors (model 2), the risk for incident CVD enhanced continuously with elevating sleep duration irregularity. Compared with sleep duration SD ≤60 min, the HRs (95% CIs) were 1.07 (0.61 to 1.88) for sleep duration SD 61 to 90 min, 1.54 (0.89 to 2.65) for 91 to 120 min, and 2.02 (1.20 to 3.39) for >120 min. Sleep duration SD as a continuous variable showed that every 1-h rise in sleep duration SD was correlated with 36% greater CVD risk (95% CI: 1.07 to 1.73; p = 0.02). The multivariable-adjusted HRs (95% confidence intervals) for CVD over categories of sleep duration SD were 1.00 (reference) for ≤60 min, 1.09 (0.62 to 1.92) for 61 to 90 min, 1.59 (0.91 to 2.76) for 91 to 120 min, and 2.14 (1.24 to 3.68) for >120 min (p = 0.002). Similarly, the HRs (95% confidence intervals) for CVD, compared with participants with a sleep timing SD ≤30 min, were 1.16 (0.64 to 2.13) for 31 to 60 min, 1.52 (0.81 to 2.88) for 61 to 90 min, and 2.11 (1.13 to 3.91) for >90 min (p = 0.002). The HRs (95% CIs) for CVD, compared with sleep-onset timing SD ≤30 min after adjusting for CVD risk factors and sleep-related factors (model 3) were 1.16 (0.64 to 2.13) for 31 to 60 min, 1.52 (0.81 to 2.88) for 61 to 90 min, and 2.11 (1.13 to 3.91) for >90 min, with 18% higher risk (95% CI: 1.06 to 1.31) for every 1-h rise in sleep-onset timing SD (p = 0.002). (Table 1)
Thus, it was concluded that new risk factors for CVD are variable sleep duration and timing, independent of traditional CVD risk factors and sleep quantity and/or quality.
Table 1: Associations of 7-Day Variability in Sleep Duration and Sleep-Onset Timing with Risk of Total Cardiovascular Disease
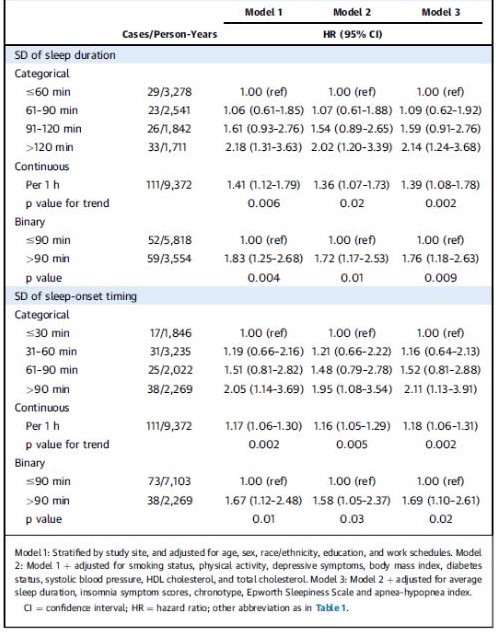
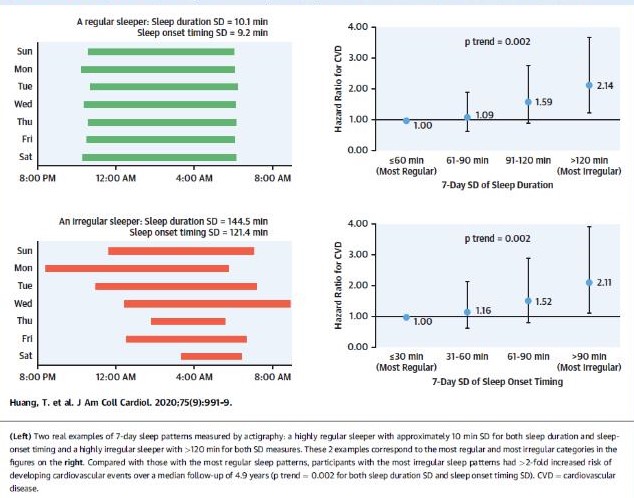
Figure 1: Regular and Irregular Sleep Patterns in Relation to Cardiovascular Disease Risk
HR: Hazard ratio; CI: Confidence interval

