Menachem JN, et al. JACC Heart Fail. 2020 Feb;8(2):87-99.
>90% of children born with CHD are expected to survive to adulthood because of enhancements in care for patients with congenital heart disease (CHD). For these adults, heart failure (HF) is the prime cause of death. But, in this heterogeneous population, advanced cardiac therapies are complex. Several CHD adults with risk profiles exhibit successful results after heart transplantation (HT) despite their complexity. Actually, for those who survive the first year, survival is better to non-CHD patients experiencing HT. These results are based on an understanding of the unique anatomic issues and co-morbidities seen in adults with CHD and advanced HF. Additionally, many factors affect transplant results such as thoughtful patient selection, intense multidisciplinary collaboration, and an appreciation for the multitude of factors.
It is especially concerning that many adults with CHD and HF do not present with typical symptoms, making it more tough to recognize HF early. Thus, it is necessary for cardiologists who take care of adults with CHD to not only identify the symptoms which are under-reported but also decreased baseline exercise capacity, and many other signs, symptoms, or laboratory test results which must be recognized as risks for HF and death. They should also be closely associated with an adult HF group that takes care for failing patients with CHD. In non-CHD patients being estimated for HT, the hemodynamic analysis particularly focuses on analysing cardiac output/ mixed venous saturation and pulmonary vascular resistance (PVR). A comprehensive anatomic and hemodynamic analysis is warranted to recognize potentially correctable residual deficiencies from the original anomaly or following repairs in an adult with CHD who shows evidence of HF. In general, pulmonary hypertension (PH) in the 2-ventricle CHD circulation is analysed and managed in a way similar to PH with heart disease, or in pulmonary arterial hypertension because of other WHO group 1 etiologies. Unlike the outlines of PH in 2-ventricle patients, there is further complexity in estimating the hemodynamics of the Fontan patient.
One of the most tough aspects of caring for adults with CHD is recognising the appropriate time for successful HT. In an attempt to minimize the number of patients whose disorder is too advanced for successful HT, it is suitable to begin a collaborative HF analysis, incorporating one for advanced treatments, before additional high-risk palliative or corrective techniques are undertaken. Perioperative morbidity and mortality remain high in adults with CHD who experience transplantation despite enhancements in patient selection and pre-operative management. Adults with CHD needing longer lengths of stay were at elevated risk for dialysis, major bleeding, stroke, and graft dysfunction; and showed more than 2-fold higher 30-day mortality, with primary graft dysfunction being the most common cause of death as compared to non-CHD transplant recipients after HT. But, for patients who survive to 1 year, long-term survival is better to non-CHD patients, with lower risks of malignancy, rejection, and cardiac allograft vasculopathy. Results are better between medium and high-volume HT centers as compared to low-volume centers, irrespective of the volume of the associated CHD program with the complexities involved in patients undergoing transplantation. Currently, at a low-volume center (<14 HT per year), 27% of adults with CHD go through HT, where 30-day and 1-year mortality is statistically greater than at higher volume centers (Figure 1).
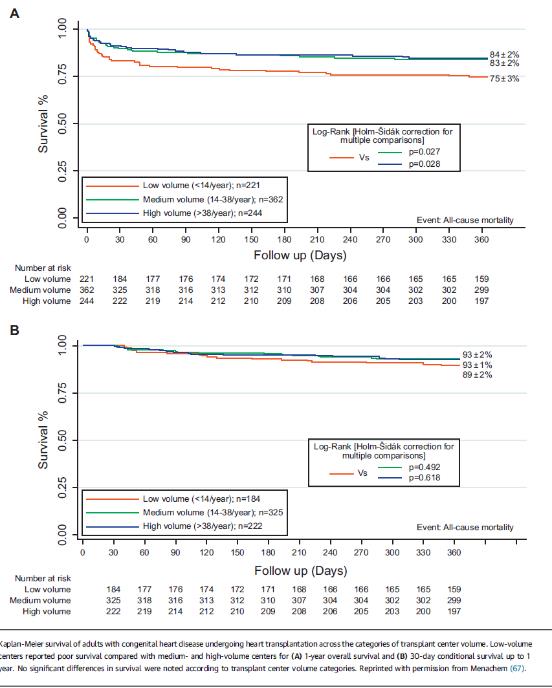
Figure 1: Transplant Survival Based on Transplant Center Volume (A) 1-year overall survival and (B) 30-day conditional survival up to 1 year
Patients with d-TGA required atrial switch and patients with l-TGA commonly generate systemic right ventricular failure as adults and may need VADs. Surgically, the pyramidal geometry of a morphological right ventricle commonly entails resection of trabeculae and/or alternate positioning of the inflow cannula, frequently on the diaphragmatic surface or free wall (Figure 2).
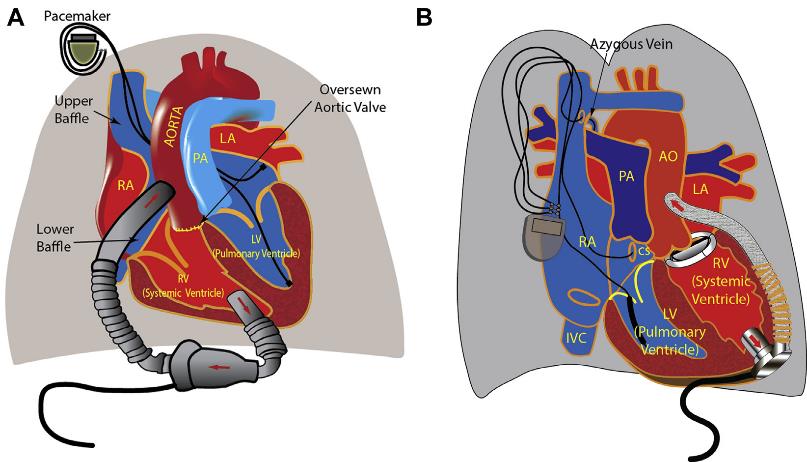
Figure 2: VAD in d-TGA and l-TGA
Thus, it was concluded that advanced HF therapies such as HT and VAD are efficacious therapy strategies for selected adults with CHD along with end-stage cardiac disease. A new issue of advanced HF was faced because of the enhanced survival of adults with CHD. There are exciting opportunities to cooperate over specialties and institutions to thoughtfully improve trials and enlarge training opportunities. In combination, these should lead to enhancements in immediate and long-term results.
WHO: World Health Organization

