Behnes M, et al. Sci Rep. 2019 Oct 3;9(1):14291.
The most common arrhythmia worldwide is atrial fibrillation (AF), as about 33.5 million individuals were analysed to endure from AF in 2010. A mechanistic link among AF and ventricular tachyarrhythmias is recommended with accumulated evidence, which may be described by decreased ventricular refractoriness and pro-arrhythmic short-long-short sequences prior the onset of ventricular tachyarrhythmias in the presence of AF instead of in sinus rhythm. But, no data is currently available on whether mortality in sequential real-life patients may be correlated independently with the presence of AF presenting on admission with ventricular tachyarrhythmias. Hence, Behnes M, et al., conducted a study to analyse the differences of short- and long-term survival of patients with ventricular tachyarrhythmias on admission regulated by the presence or absence of AF. The present study is obtained from the RACE-IT which incorporated all patients presenting with at least one episode of ventricular tachyarrhythmias and sudden cardiac arrest from 2002 to 2016 at one institution retrospectively. 12-lead electrocardiogram (ECG), ECG tele-monitoring, ICD or external defibrillator monitoring documented ventricular tachyarrhythmias. Only patients presenting with and surviving ventricular tachyarrhythmias at index hospital stay were included for the present evaluation. As per the European guidelines, risk-stratification was executed according to the presence of AF. The primary endpoint was described as long-term all-cause mortality at 2.5 years of follow-up. Secondary endpoints were all-cause mortality at 30-days, in-hospital death at index and all-cause mortality of surviving patients of index hospitalization (i.e. after discharge).
31% patients showed a history of AF from 1,993 sequential patients of the unmatched study population presenting with ventricular tachyarrhythmias on admission at institution. Most patients experienced paroxysmal (70%), followed by permanent (21%) and persistent AF (9%). The rate of VT was substantially higher in AF patients (67% vs 59%; p = 0.001), although VF was more frequent in non-AF patients (41% vs 33%; p = 0.001). AF patients with ventricular tachyarrhythmias exhibited a higher rate of the primary endpoint of long-term all-cause mortality at 2.5 years as compared to non-AF patients (40% vs 24%; log-rank p = 0.001; HR = 1.825; 95% CI 1.548–2.153; p = 0.001) (Figure 1).
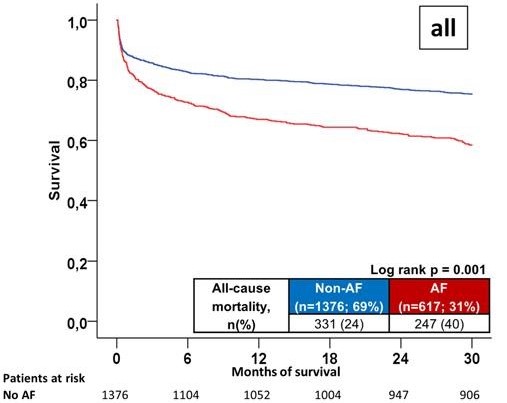
Figure 1: Primary endpoint: Long-term all-cause mortality at 2.5 years comparing AF with non-AF patients
Patients with AF showed increased mortality in VT also (mortality rate 36% vs 18%; log rank p = 0.001; HR = 2.283; 95% CI 1.817–2.869; p = 0.001) (Figure 2).
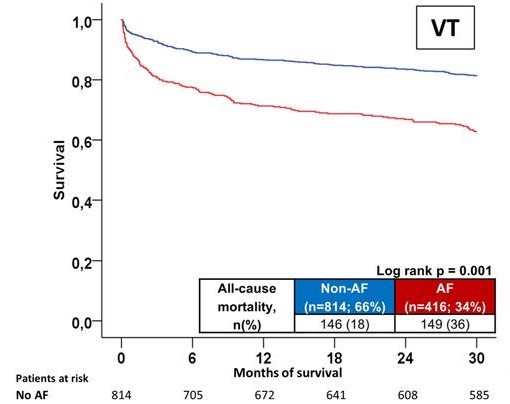
Figure 2: Primary endpoint: Stratified according to underlying ventricular tachyarrhythmias, VT
Patients with AF exhibited elevated mortality in VF also (mortality rate 49% vs 33%; log rank p = 0.001; HR = 1.572; 95% CI 1.230–2.009; p = 0.001) (Figure 3).
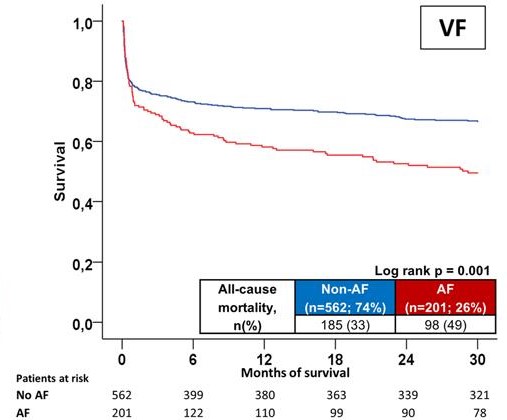
Figure 3: Primary endpoint: Stratified according to underlying ventricular fibrillation, VF
In secondary endpoints, AF patients showed increasing rates of all-cause mortality at 30 days (17% vs 12%; HR = 1.467; 95% CI 1.146–1.878; p = 0.002), at index hospitalization (19% vs 13%; HR = 1.467; 95% CI 1.146–1.878; p = 0.002), and index hospitalization (21% vs 12%; HR = 1.467; 95% CI 1.146–1.878; p = 0.002).
Thus it was concluded that AF is an independent forecaster of death in patients exhibiting sequentially with ventricular tachyarrhythmias.
RACE-IT: Registry of malignant arrhythmias and sudden cardiac death

