Tsutsui H, et al. Circ J. 2019 Sep 25;83(10):2049-2060.
The raised heart rate (HR) in the resting state is an independent risk factor for death and cardiovascular outcomes in patients with heart failure (HF). Ivabradine, a HR-reducing agent acts by blocking hyperpolarisation-activated cyclic nucleotide-gated (HCN) channel which is responsible for cardiac pacemaker. A multicenter, randomised, double-blind, placebo-controlled, parallel-group, Japanese SHIFT phase III study (J-SHIFT) was conducted to investigate the efficacy and safety of Ivabradine in patients with reduced ejection fraction (HFrEF). The aim of the J-SHIFT study was to confirm numerical improvement in the primary composite endpoint of cardio-vascular death or hospital admission for worsening HF as a point estimate of the hazard ratio <1 because of feasibility.
A total of 254 patients enrolled in the study were randomly divided into treatment group i.e. Ivabradine (n=127) and placebo group (n=127). Patients with stable symtomatic chronic HF of New York Heart Association (NYHA) functional class II–IV, left ventricular EF (LVEF) ≤35%, resting HR ≥75 beats/min in sinus rhythm, received optimal treatment for HF according to the Japanese Guidelines for Treatment of Chronic Heart Failure. Resting HR was significantly reduced in the Ivabradine group compared with the placebo group at final visit (15.2 vs. 6.1 beats/mins, p<0.0001) (Figure 1). The primary composite endpoint of cardiovascular death or hospital admission for worsening HF occurred at a lower rate in the Ivabradine group than in the placebo group (20.5 vs. 29.1%) (hazard ratio 0.67, 95%, CI 0.40–1.11, p=0.1179) during median follow-up of 589 days (Figure 2). Mild phosphenes were reported in 8 patients in the Ivabradine group and 4 patients in the placebo group (6.3 vs. 3.1%, p=0.3760). No cases of symptomatic bradycardia were reported in either group. Thus, the J-SHIFT study proved the efficacy and safety of Ivabradine in Japanese HFrEF patients, in consensus with the SHIFT study.

Figure 1: Time-dependent changes in resting heart rate during the treatment.
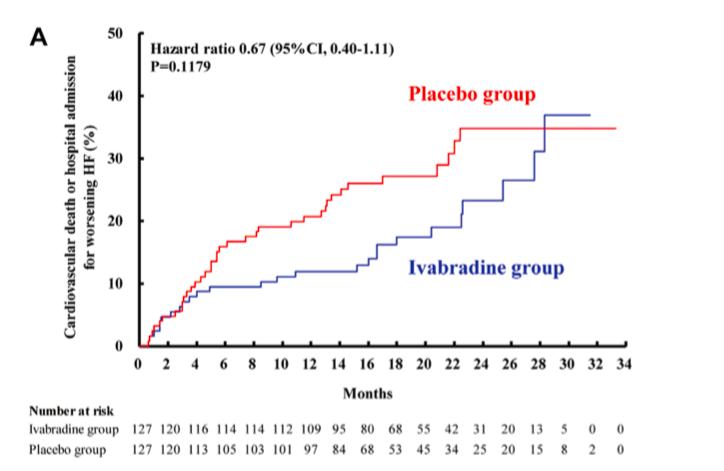
Figure 2: Kaplan-Meier cumulative event curves for the primary composite endpoint of cardiovascular death or hospital admission for worsening heart failure.

