Nishiwaki H. J Clin Hypertens (Greenwich). 2021 Mar 1.
In patients with idiopathic nephrotic syndrome, a conventional or adjunctive treatments are angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs). The factors correlated with their prescription, is clinically significant as it may aid resolve the guideline-practice gap elucidating the actual prescription patterns of ACEIs and ARBs, and provide as a source for future studies on underlying glomerular diseases for which efficacy of ACEIs and ARBs remains unknown. Thus, Nishiwaki H, et al. conducted a study to analyse the prevalence and occurrence of ACEI/ARB prescription, and the clinical attributes correlated with their prescription in idiopathic nephrotic syndrome with a nationwide cohort database named Japan Nephrotic Syndrome Cohort Study (JNSCS).
1,986 patients with biopsy-confirmed primary nephrotic syndrome incorporating minimal change disease (MCD), membranous nephropathy (MN), focal segmental glomerulosclerosis (FSGS), and others were enlisted in the JNSCS, incorporating 56 facilities in the entry period among January 2009 and December 2010 with a 5-year observation period. The correlations of the candidate factors with both prevalence and occurrence of ACEI/ARB prescriptions were examined. The candidate factors, gathered at baseline, were used to analyse the correlation with the prevalence. The candidate factors are the attributes of patients with nephrotic syndrome such as age, pathology patterns, baseline systolic blood pressure (SBP), serum creatinine level, UPCR, antihypertensive drugs other than ACEI/ARB, the prescription of antidiabetic drugs, and the prescription of immunosuppressive agents incorporating glucocorticoid. The outcomes were the prevalence of ACEI/ARB prescription at baseline (date of renal biopsy or date of immunosuppressant initiation) and at 2 months following baseline
A total of 326 patients were eligible to analyse the prevalence of ACEI/ARB. 122 (37.4%) patients were already given ACEI/ARB. 204 patients were incorporated to examine the occurrence of ACEI/ARB following exclusion of those patients from the baseline population. Between those who were not prescribed ACEI/ARB at baseline, a total of 52 (34.2%) and 67 (32.8%) patients were newly prescribed within 1 and 2 months following the commencement of immunosuppressive therapy, respectively. The pathology patterns such as MN (adjusted odds ratio (AOR), 4.96; 95% confidence interval (CI), 2.53–9.72), FSGS (AOR, 3.95; 95% CI, 1.61–9.66), and other pathology patterns (AOR, 3.07; 95% CI, 1.14–8.26) were substantially correlated with a greater likelihood of being prescribed than MCD. Additionally, age (per 1-year increase, AOR, 1.02; 95% CI, 1.00–1.04), prescription of antihypertensive drugs other than ACEI/ARB (AOR, 2.18; 95% CI, 1.21–3.92), and the prescription of antidiabetic drugs (AOR, 6.57; 95% CI, 1.77–24.4) were also substantially correlated with ACEI/ARB prescription, resp. (Table 1)
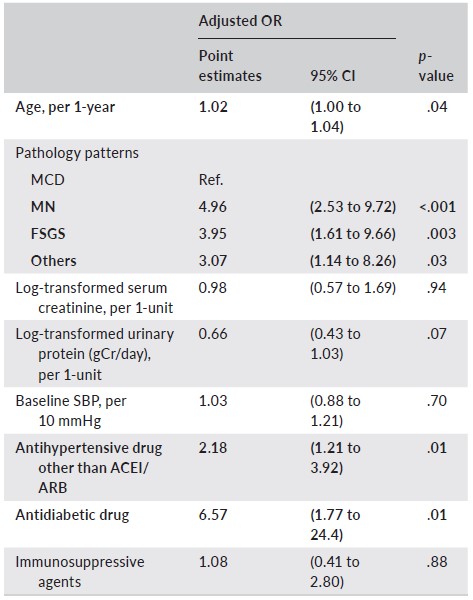
Table 1: Association of patients’ characteristics with prevalence of ACEI/ARB prescription (N = 326)
The pathology patterns of MN (AOR, 6.00; 95% CI, 2.57–14.0) and other pathology patterns (AOR, 3.89; 95% CI, 1.17–12.9) were substantially correlated with the event prescription than MCD. The correlation of FSGS with incident prescription was not apparent (AOR, 1.79; 95% CI, 0.58–5.52). Baseline SBP (AOR per 10 mmHg, 1.36; 95% CI, 1.09–1.70) was also substantially correlated with event prescription (Table 2).
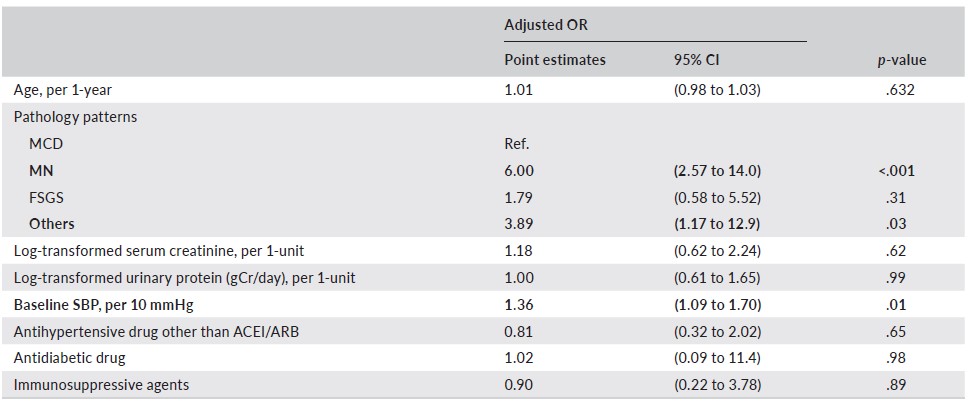
Table 2: Association of patients’ characteristics with incidence of ACEI/ARB prescription (N = 204)
On average, there was substantial increase in the occurrence of ACEI/ARB prescription as baseline SBP increased from 100 to 140 mmHg (19.2% to 40.8%) (Figure 1).
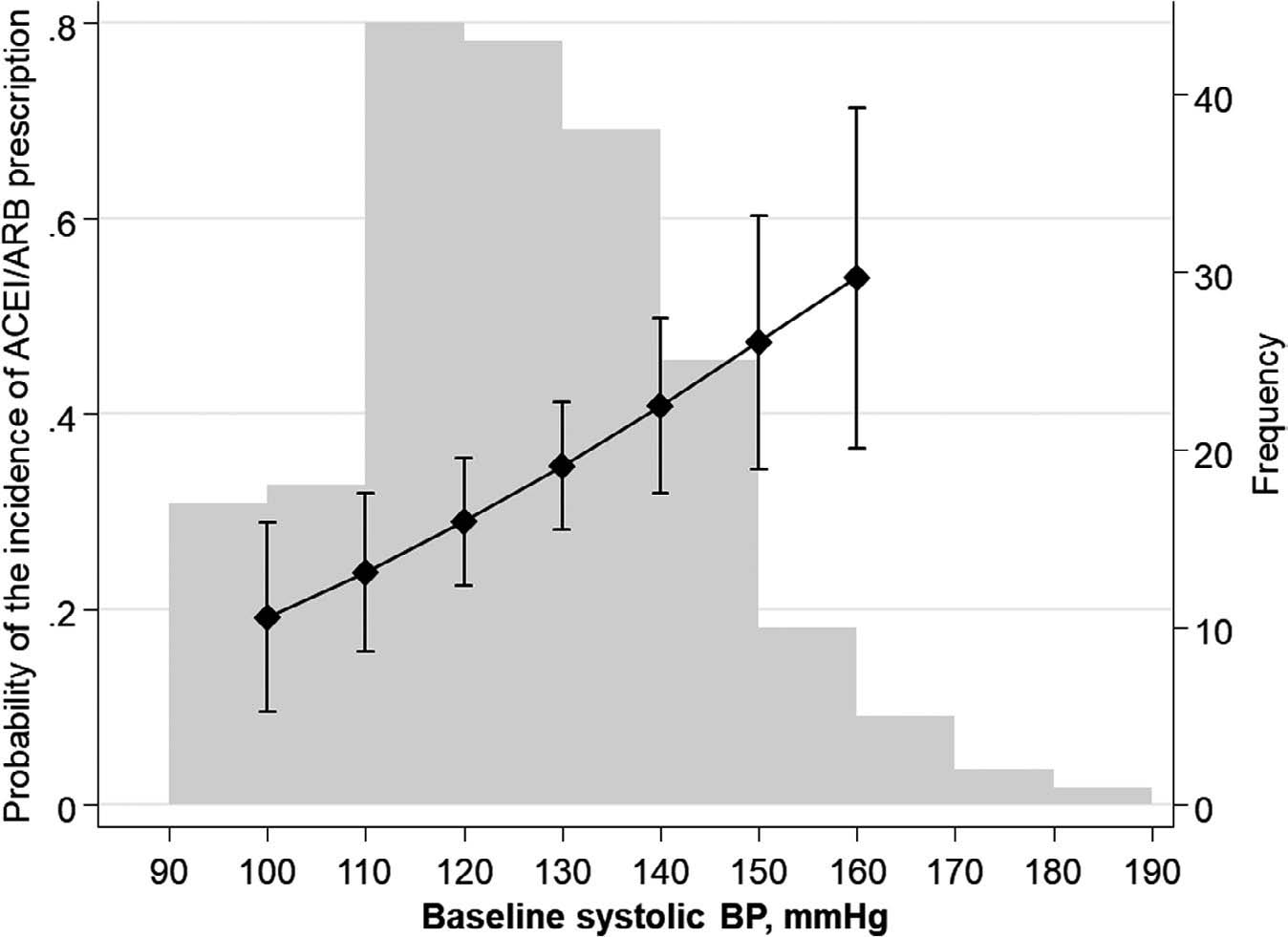
Figure 1: Probability of incident ACEI/ARB prescription by baseline Systolic Blood Pressure (SBP)
Using the multivariable adjusted logistic model, adjusted probability by baseline SBP was predicted. The left vertical axis shows probability of incident ACEI/ARB prescription. The connected line indicates point estimates. The vertical lines indicate 95% confidence intervals. Gray bars indicate frequency of the baseline SBP values. The right vertical axis shows frequency of each gray bar
Thus, it was concluded that the prevalence and occurrence of ACEI/ARB prescription was correlated with several factors. More specifically, the actual practice pattern of ACEI/ARB prescription was indicated for patients with well-controlled blood pressure. Therefore, Japanese nephrologists are likely to prescribe ACEIs/ARBs for nephrotic patients with MN or high baseline SBP, even below the hypertensive range. These findings could be beneficial for further studies to analyse the efficacy of ACEI/ARB on renal effects in patients.

