Maagaard M, et al. Syst Rev. 2019 Feb 1;8(1):39.
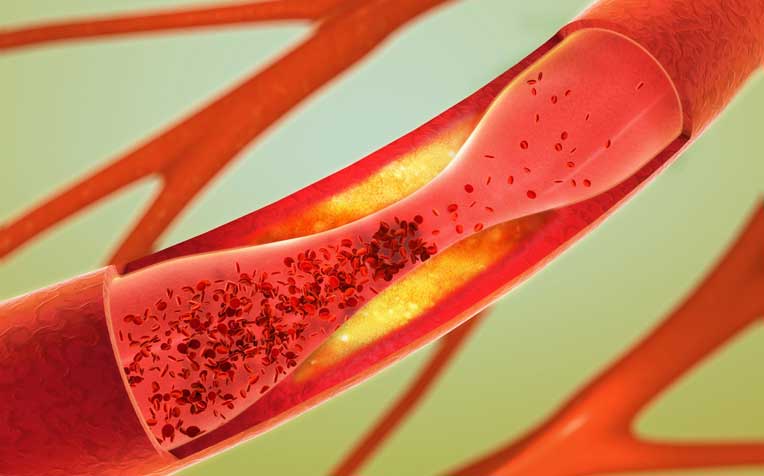
Ischaemic heart disease (e.g. coronary artery disease) is responsible for almost half of all cardiovascular deaths with around 30% of all deaths worldwide in cardiovascular diseases. The prevalence of coronary artery disease was approximately 93 million in 2013 globally, increased by 65% in between 1990 and 2013. The main aim in the treatment of coronary artery disease is preventing attacks of angina and treating attacks as they occur. The treatment of heart failure is focused on enhancing clinical status, functional capabilities, and quality of life; prevent hospitalisation; and decrease mortality. 2.5 to 7.5 mg of Ivabradine twice daily is given in tablet form for both coronary artery disease and heart failure. However, another review of randomised trials on Ivabradine for coronary artery disease with or without left ventricular dysfunction discovered that Ivabradine did not show the effect on the risk of all-cause mortality, cardiovascular death, or hospitalisation for new onset or worsening heart failure. Thus Maagaard M et al., conducted a study to analyse the advantageous and deleterious effects of Ivabradine in the treatment of coronary artery disease and/or heart failure.
Based on the PRISMA-P guidelines, the protocol for a systematic review has been developed analysing intercessions in healthcare and the Cochrane Handbook. Participants with coronary artery disease and/or heart failure, irrespective of age, sex, and comorbidities were included. The primary outcomes, secondary outcomes and exploratory outcomes were estimated. The relevant trials were searched from CENTRAL, MEDLINE, EMBASE, LILACS, Science Citation Index Expanded on Web of Science, CBM, CNKI, Chinese Science Journal Database (VIP), and BIOSIS. The review was executed with the recommendations of The Cochrane Collaboration. The Review Manager and Trial Sequential Analysis were used to execute the examinations. A trial is classified as being at overall ‘low risk of bias’, only if all bias domains are classified as ‘low risk of bias’. A trial is classified as being at overall ‘high risk of bias’, if any of the bias domains are classified as ‘unclear’ or ‘high risk of bias’. The primary conclusions will be based on the primary outcomes at overall low risk of bias.
The statistical software Review Manager 5.3 was used by Cochrane to analyse data. The intercession effects with both random effects meta-analyses and fixed effects meta-analyses were estimated. The Trial Sequential Analysis was performed on the outcomes, in order to compute the needed information size (that is the number of participants required in a meta-analysis to discover or refuse a certain intercession effect) and the cumulative Z-curve’s breach of relevant trial sequential monitoring boundaries. GRADE evaluation of imprecision was compared based on a fixed effects model calculation of the optimal information size with Trial Sequential Analysis based on a random effects model and heterogeneity correction of the needed information size. The risk of random errors and systematic errors were considered through pre-defined methodology.
The substantial overlap was found among patients with coronary artery disease and heart failure and hence, in these different patient groups, the effects of Ivabradine might be similar. A reliable evidence adjusted for bias, sparse data, and multiple testing concerning the treatment of coronary artery disease and heart failure using Ivabradine was assigned to the clinicians and decision-makers on clinical practice with this systematic review.
It was concluded that the systematic review possessed the potential to help clinicians in decision-making as Ivabradine exhibited advantages to the patients with coronary artery disease and/or heart failure.
PRISMA-P: Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols; CENTRAL: Cochrane Central Register of Controlled Trials; MEDLINE: Medical Literature Analysis and Retrieval System Online; EMBASE: Excerpta Medica database; LILACS: Latin American and Caribbean Health Sciences Literature; CBM: Chinese Biomedical Literature Database; CNKI: China National Knowledge Infrastructure.

