Lu J. J Reconstr Microsurg. 2019 Feb;35(2):117-123.
Lu J, et al. conducted a single-center retrospective study to analyse reconstructive and functional outcomes in patients who underwent free tissue transfer (FTT) for recalcitrant diabetic foot ulcers (DFUs) management for advanced limb salvage. Overall 29 patients underwent lower extremity FTT for diabetic foot reconstruction. In all cases, microsurgical reconstruction was offered as an alternative to major amputation for the management of recalcitrant DFUs. Primary outcomes included overall flap survival, rates and timing of major amputation, and postoperative ambulatory status.
Functional outcomes after surgery were evaluated using the lower extremity functional scale (LEFS) score. The LEFS evaluates patients’ ability to perform 20 various ambulatory activities (i.e., performing work around the house, putting on socks/shoes, walking up/down stairs, running, etc.). Patients rate their abilities on a scale from 0 to 4, with 0 indicating extreme difficulty or inability to perform tasks, and 4 indicating no difficulty with the task. All responses are summated, giving the total LEFS score. Administration of the survey was conducted at least 9 months after FTT to assess outcomes of the reconstruction after patients had adequate time to recover and regain ambulatory capacity. Subgroup analysis of functional outcomes in patients with successful limb salvage versus those with below-knee amputation (BKA) was performed. The Fisher’s exact test was performed to evaluate correlation between patient comorbidities and primary outcomes.
Results were observed:
Primary outcomes
- Overall flap success rate was 93%
- Of the 29 free flaps performed for diabetic foot reconstruction, 4 patients (14%) required take backs to the operating room for microvascular compromise (n = 3) and hemorrhage (n = 1)
- 7 patients required major lower extremity amputation (LEA) during the follow-up period, resulting in an overall limb salvage rate of 76% for this series
- Indications for major amputation included persistent hardware infection (n = 4), recalcitrant soft tissue infection (n = 1), and chronic intractable pain (n = 1)
- Average interval between FTT and subsequent amputation was 8 ± 5.2 months (r, 0.2–15 months)
- Other postoperative complications included 4 (14%) patients with wound dehiscence, 4(14%) patients with surgical site infection, and 1 patient (3%) requiring debulking
Functional outcomes
- Overall rate of lower limb salvage was 79%
- Seven patients in this series ultimately required below-knee amputation secondary to recalcitrant infection (n = 5), intractable pain (n = 1), and limb ischemia (n = 1)
- The LEFS survey was administered to patients at a mean time of 19 ± 11 months (r, 3.5–36 months) after FTT, with an average score of 46 ± 22 (r, 12–80)
- The average LEFS score was 45 ± 22.7 (r, 12–80) in the limb salvage cohort and 49 ± 21.6 (r, 22–80) in the BKA cohort
- After FTT, patients scored on average 2.8 out of 4 points in low-demand activities, and 1.3 out of 4 points in high-demand activities
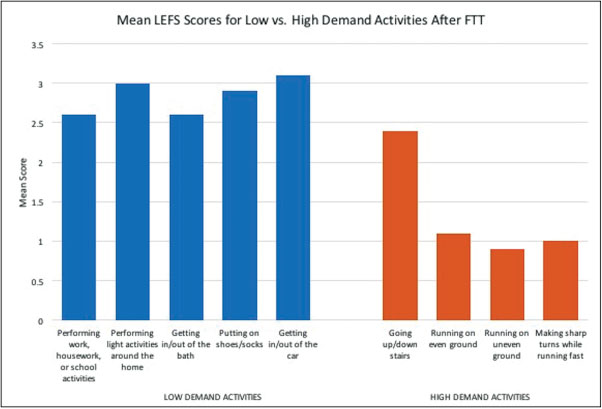
Figure 1: Mean LEFS scores after FTT for diabetic limb salvage. Higher mean scores for low-demand versus high-demand activities indicate that patients are more likely to return to independent ambulation and basic functionality after successful free flap reconstruction
Subgroup analysis
- Both subgroups were equivalent with regard to rates (86 vs. 86%, p > 0.05) and timing (3.4 vs. 2.7 months, p > 0.05) of ambulation in patients with successful limb salvage to those underwent BKA
Fisher’s exact test
- Fisher’s exact test did not find any of the above comorbidities to significantly increase risk of either flap loss (p > 0.05) or BKA (p > 0.05)
Thus, it was concluded that FTT for the management of recalcitrant DFUs is associated with high rates of reconstructive success and postoperative ambulation. However, several patients will eventually require major amputation for reasons unrelated to ultimate flap survival. These data should be used to counsel patients regarding the risks, functional implications, and prognosis of microvascular diabetic foot reconstruction.

