Haugaa KH, et al. Europace. 2018 Sep 1;20(FI2):f249-f253.
Haugaa KH, et al. conducted a study to estimate the extent of the variation between daily clinical practice and the 2015 SCD ESC guidelines among electrophysiology centres in Europe.
Participating centres
An on-line questionnaire adapted by members of the Scientific Initiatives Committee of the European Heart Rhythm Association (EHRA) was issued to members of the EHRA Electrophysiology Research Network including 17 countries. From 17 different countries, of 40 centres, 91% were University hospitals, 7% were private centres, and the rest were non-University hospitals.
Screening of sudden cardiac death victims and family members
In a victim of unexplained SCD <35 years of age with no findings at autopsy, 53% of respondents would perform genetic testing of the victim and subsequent screening of the family if a positive result was found in the victim. Almost in 53% of respondents conducting genetic testing in a victim of unexplained SCD <35 years of age with no findings at autopsy and consequent screening of the family if a result was found to be positive in the victim. Of those not conducting genetic screening of the victim, half conducted clinical family screening including electrocardiogram (ECG) and echocardiography and the other half also did exercise test and Holter monitoring in the 23% of family screening.
Coronary artery disease and nonischaemic dilated cardiomyopathy
Difference between respondents were observed in the management strategy for patients with non-ischaemic dilated cardiomyopathy (DCM) with LVEF 45% and asymptomatic non-sustained VT (NSVT) on optimal medical therapy. Almost 85% of the majority of respondents chose conservative heart failure therapy with regular clinical follow-up (Figure 1).
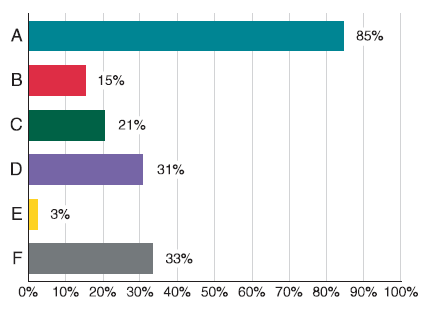
Figure 1: Which is your strategy in a patient with non-ischaemic dilated cardiomyopathy, ejection fraction 45%, and asymptomatic non-sustained ventricular tachycradia (non-bundle branch re-entry, non-outflow tract morphology) on optimal medical therapy? (multiple answers): (A) Conservative heart failure therapy with regular clinical follow-up. (B) Electrophysiological study for risk stratification. (C) Catheter ablation. (D) Amiodarone. (E) ICD implantation. (F) Perform genetic analysis for LMNA mutation and/or family history of sudden death and accordingly decide for ICD implantation. ICD, implantable cardioverter-defibrillator.
Inherited primary arrhythmia syndromes
All respondents advised ICD implantation in SCD survivors with a Brugada type ECG. Almost 76% of majority treated ICD in patients with syncope and type 1 Brugada ECG, while 24% considered ICD in the same patients only after a positive PVS (Figure 2).
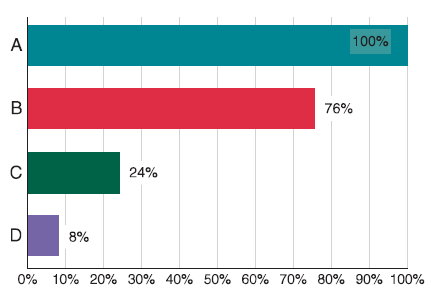
Figure 2: In patients with Brugada syndrome, I consider ICD implantation under the following scenario (multiple answers): (A) In an SCD survivor with a Brugada type ECG. (B) In a patient with syncope and a spontaneous type 1 Brugada ECG. (C) In patients with syncope and a spontaneous type 1 Brugada ECG, only after positive electrophysiological study. (D) In first-degree relatives of a Brugada patient with (aborted) SCD. ECG, electrocardiogram; ICD, implantable cardioverter-defibrillator; SCD, sudden cardiac death.
Thus, this EHRA survey provides a snap-shot brief of cardiologists’ adherence to the European SCD guidelines. The important issues examined were (i) screening of SCD victims and family members (ii) strategies in patients with coronary artery disease and non-ischaemic cardiomyopathy, (iii) risk stratification and management of patients with cardiomyopathies, and (iv) risk stratification and management of patients with ion channel disease.

