Eur J Prev Cardiol. 2019 Dec 2:2047487319890973.
Preparticipation evaluation (PPE) offers the potential to prevent sudden cardiac death (SCD) in young athletes by early identification of cardiac diseases at risk of malignant ventricular arrhythmias (VA). According to the 1982 Italian law, the PPE protocol includes a constant-load ECG stress test (EST; modified Montoye step test), in addition to history, physical examination and resting ECG. More recently, the EST has been upgraded and is currently performed by many sports medicine centres using a bicycle or treadmill and under continuous ECG monitoring. This has allowed the occurrence, morphology and complexity of VA to be assessed during the EST, which may be the only phenotypic manifestation of an underlying disease in athletes with negative history, unremarkable physical examination and normal resting ECG. However, the effect of VA induced by EST on the diagnostic yield and the positive predictive value of PPE remains to be established. Thus, Zorzi A et al., conducted a study to assess the results of adding an EST for the evaluation of VA to the traditional PPE protocol consisting of history, physical examination and resting ECG.
The study included a consecutive series of competitive non-professional athletes from 12 to 35 years old undergoing annual PPE between 2013 and 2018. Evaluation of a consecutive cohort of young athletes with history, physical examination, resting ECG and EST was performed. Athletes with VA induced by EST underwent 24-hour 12-lead Holter monitoring and echocardiography. Cardiac magnetic resonance (CMR) was reserved for those with frequent, repetitive or exercise-worsened VA, and for athletes with echocardiographic abnormalities.
During the 5-year study period, 10,985 non-professional competitive athletes (66% males, median age 15 years, 97% White) underwent PPE. Of those, 451 (4.1%, 95% CI 3.7%–4.5%) showed positive medical history, pathological physical examination or abnormal baseline ECG. Of the remaining 10,534 athletes with a normal history, physical examination and baseline ECG, 524 (5.0%, 95% CI 4.6%–5.4%) showed PVBs at EST including 73 (14%) with couplets or non-sustained ventricular tachycardia. Arrhythmias were observed before exercise in 126 (24%) athletes, during the initial phase of the test (first and second minute) in 204 (39%), at peak of exercise (i.e. during the third minute) in 88 (17%) and during the post-exercise phase in 253 (48%). In 27 (5%) athletes VA occurred only at peak of exercise. A total of 303 (58%) athletes showed less than 10 PVBs while 107 (21%) more than 500 PVBs. Couplets or nonsustained ventricular tachycardia were recorded in 132 (25%) athletes. Among the 221 athletes with 10 PVBs or more, 164 (75%) showed monomorphic PVBs (fascicular, N=2; LBBB, N=110; and RBBB, N=52) while 57 (25%) exhibited multifocal VA. A total of 87 out of 524 (17%) athletes with VA at EST underwent CMR. Among the 87 athletes, CMR was abnormal in 18 (21%). Overall, 16/18 athletes with an abnormal CMR showed LV LGE with a non-ischaemic distribution. (Figure 1)
Overall, 23 of 10,534 (0.22%, 95% CI 0.14–0.33%) athletes with negative history, physical examination and baseline ECG received a diagnosis of a cardiac disease. This equates to a 75% increase (from 31/10.985, 0.28% to 54/10.985, 0.49%) in the diagnostic yield of a PPE protocol including EST for VA compared with history, physical examination and resting ECG only. At the same time, the number of athletes who were prescribed additional investigations that resulted negative increased from 420 (3.8%) to 921 (8.4%) and the positive predictive value of PPE decreased by 20% (from 6.9% to 5.5%). During a 32 ± 21 months follow-up, no cardiac arrests occurred among either eligible athletes or non-eligible athletes with cardiovascular disease.
Thus, it was concluded that the addition of exercise testing for the evaluation of VA inducibility to history, physical examination and ECG resulted in an increase of the diagnostic yield of PPE at the expense of an increase in false-positive findings.
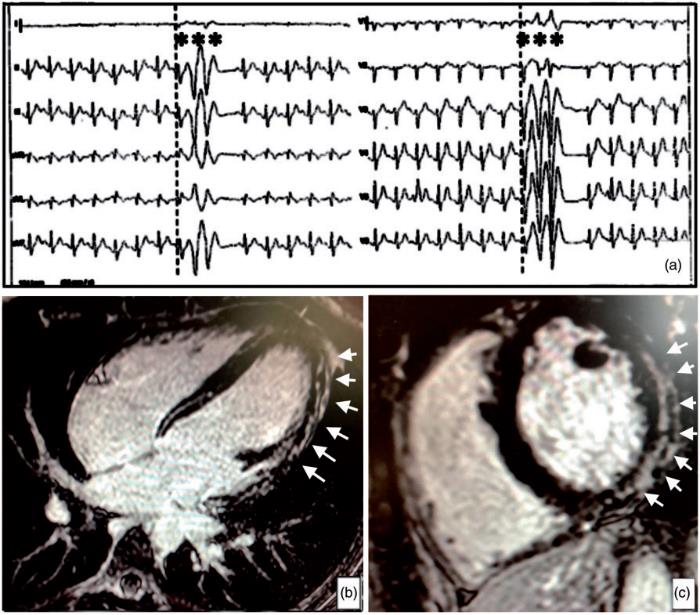
Figure 1: Representative case of a 17 year-old athlete with complex ventricular arrhythmias induced by stress testing. The athlete had negative history, unremarkable physical examination and normal resting electrocardiogram. (a) During exercise-testing, complex ventricular arrhythmias with a right-bundle-branch-block/superior axis morphology were recorded at peak of exercise. Echocardiography was normal (not shown). On post-contrast cardiac magnetic resonance sequences, a subepicardial/midmyocardial stria of late gadolinium enhancement involving the left-ventricular wall was visible on: (b) short-axis view; (c) four-chambers view.
PVBs: premature ventricular beats; LV LGE: left ventricular late gadolinium enhancement

