Spannella F. J Hypertens. 2020 Mar;38(3):546-552.
Hypercholesterolemia and hypertension normally coexist, serving as the prime alterable cardiovascular risk factors. In order to decrease the load of cardiovascular morbidity and mortality, an efficacious control of hypertension and dyslipidemia should be followed in clinical practice. The long-term advantageous impacts of statins on cardiovascular morbidity and mortality have been clearly showed and statin therapy is a cornerstone therapy of dyslipidemia. In several previous studies, statin therapy was correlated to lower BP values on hypertensive patients in addition with the reduction of blood cholesterol. But, most of these studies considered only office BP values with mixed consequences. But several confounding factors, such as the different antihypertensive drugs taken by patients influenced the relationship among ambulatory BP and statin treatment. Spannella F, et al., conducted a study to analyse the correlation among statin therapy and ambulatory BP control in a wide population of outpatients mentioned to hypertension centre. Also, a propensity score matching analysis was executed to decrease the effect of the possible confounding factors.
1827 consecutive outpatients were enrolled from January 2016 and December 2018 in a retrospective study. The inclusion criteria were as follows: essential hypertensive patients aged at least 18 years, a valid 24-h ambulatory blood pressure monitoring (ABPM), no changes in both antihypertensive and statin therapy in the previous 3 months. The following clinical parameters were analysed: patients’ medical history, laboratory measurements, anthropometric measurements, ABPM parameters and drug therapy. Three sequential oscillometric automatic BP measurements were performed on both arms concurrently with a validated device in the clinical visit. All patients with lipid-lowering therapy took their statin between 1800 and 2200 h. Antihypertensive treatment intensity (ATI) was determined to compare different drug correlations. A propensity score matching was used to compare two equally-sized groups of patients with similar characteristics as per the statin therapy. Matching was executed on log-transformed propensity score in a 1 :1 fashion with a caliper of 0.1, considering the different baseline characteristics among statin and no-statin group.
Mean age of patient was 58.1±13.8 years, with male prevalence (55%). 402 (22.0%) patients were on statin therapy. Patients on statin therapy were older and they had both greater BMI and prevalence of type 2 diabetes mellitus, as compared to no-statin group. They also had greater prevalence of previous CAD (12.7 vs. 0.7%, p<0.001) and TIA/stroke (13.7 vs. 4.1%, p<0.001), as well as lower eGFR, as compared to the no-statin group. Additionally, they took more antihypertensive drugs (2.4±1.3 vs. 1.5±1.2, p<0.001), independently from the pharmaceutical class, and they also had a greater ATI. Hence, patients on statin therapy had lower TC and LDLc. 776 (42.5%) patients had 24-h BP control. In office SBP, no difference was seen among statin and no-statin group (132.5±16.2 vs. 133.3±14.9 mmHg, p=0.354), although statin group had lower office DBP (74.4±9.9 vs. 81.1±10.5mmHg, p<0.001). No correlation was seen between office BP control and statin therapy (67.3 vs. 65.3%, p=0.480). Patients on statin treatment had lower 24-h, daytime and night-time BP as compared to patients who did not take a statin, with a higher difference for DBP (Fig. 1, panels a–c). The statin group also showed higher 24-h PP (55.6±11.9 vs. 51.3±10.2 mmHg, p<0.001). Simultaneously, statin treatment was correlated with a better ambulatory BP control (58.7 vs. 37.9%, p<0.001 for 24-h BP control; 61.7 vs. 43.4%, p<0.001 for daytime BP control; 46.5 vs. 29.8%, p<0.001 for night-time BP control). 369 patients on statin treatment were matched with as many untreated patients. The consequences were confirmed even in the propensity score matched groups. Statin treatment was correlated with lower 24-h, daytime and night-time BP, despite statistical non-significance for 24-h and daytime SBP (Fig. 1, panels d–f). Patients on statin therapy had a greater prevalence of ambulatory BP control as compared to patients not taking statins [60.6 vs. 46.2%, p<0.001, OR 1.8 (95% CI 1.3– 2.4) for 24-h BP control; 63.3 vs. 51.6%, p=0.001, OR 1.6 (95% CI 1.2–2.2) for daytime BP control; 46.2 vs. 33.2%, p<0.001, OR 1.7 (95% CI 1.3–2.3) for night-time BP control].
Thus, it was concluded that statin therapy is correlated with superior ambulatory BP control in essential hypertensive patients. The intensity of the antihypertensive therapy or the evaluation of various cofactors did not influence the consequence.
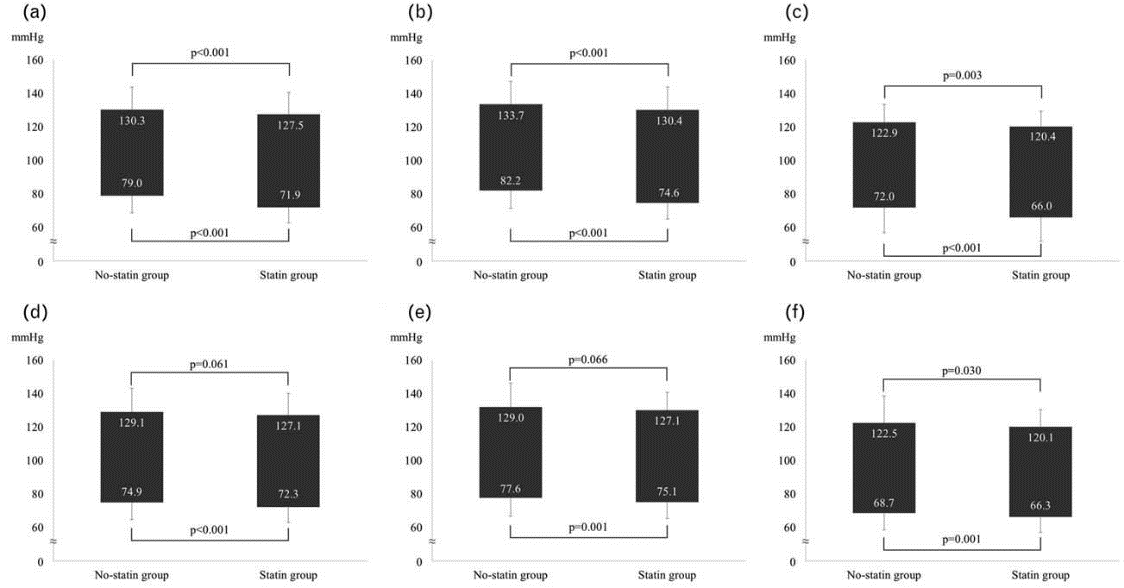
Figure 1: Ambulatory blood pressure and statin therapy. Panel a: 24-h blood pressure and statin therapy in the study population. Panel b: daytime blood pressure and statin therapy in the study population. Panel c: night-time blood pressure and statin therapy in the study population. Panel d: 24-h blood pressure and statin therapy in propensity score matched groups. Panel e: daytime blood pressure and statin therapy in propensity score matched groups. Panel f: night-time blood pressure and statin therapy in propensity score matched groups.
BP: Blood pressure; BMI: Body mass index; CAD: Coronary artery disease; TIA: Transient ischemic attack; TC: Total cholesterol: LDL-c: Low-density lipoprotein cholesterol; eGFR: estimated Glomerular filtration rate; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; PP: Pulse pressure; OR: Odd ratio; CI: Confidence interval

