Novel and Emerging Therapies: Inclisiran
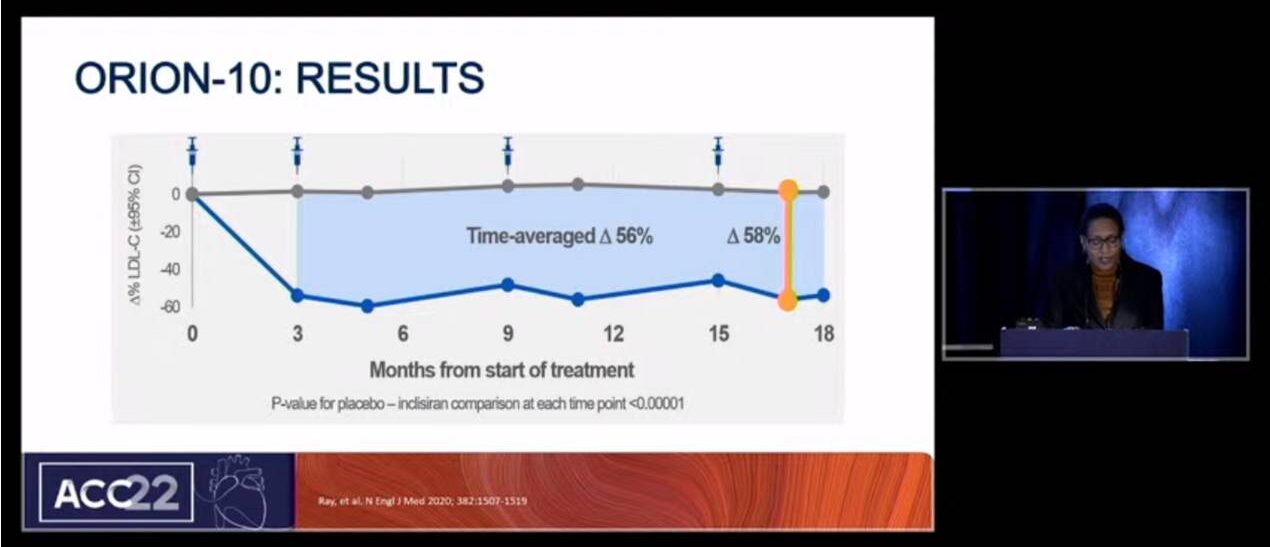
Watson K, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. LDL is the causative agent in atherosclerosis and lowering LDL-C decreases events. Proprotein convertase subtilisin/kexin type 9 (PCSK9) is a secreted protein which targets the LDL receptor for degradation. Its gain of function mutations causes high LDL-C and loss of function causes low LDL-C. Inhibition of PCSK9 lowers LDL-C levels and statin treatment can upregulated it. As per PCSK9 inhibitor RCTs, ODYSSEY trial showed that Alirocumab significantly reduces the Major adverse cardiovascular events (MACE) (RRR 15%) as compared to placebo in 18,924 patients and FOURIER trial showed that Evolocumab significantly reduces CV death, MI, stroke rate (RRR 15%) as compared to placebo in 27,564 patients. Current PCSK9i are monoclonal antibodies. These drugs are administered as SQ injections every 2-4 weeks. New approach has been introduced in the RNA interference to inhibit PCSK9 synthesis in the liver. Phase I trial of the PCSK9i Inclisiran (using the RNAi approach) 300 mg showed that LDL-C could be reduced ~50% with twice yearly injections for 4-6 months. 2 doses of Inclisiran lowered LDL-C for upto 6 months. In ORION-10 study, 1561 patients on maximally tolerated statin were randomized to Inclisiran or placebo. Inclisiran showed significant reduction in LDL-C ∆% by 58% after 17 months of treatment (p<0.00001). Also, Inclisiran had similar safety and tolerability compared with placebo.
Inclisiran is the first cholesterol-lowering agent in the siRNA class. Twice yearly injection of Inclisiran provides sustained LDL lowering. Increasing the number of effective therapeutic options available is good for the patients.
Novel and Emerging Therapies: Bempedoic Acid
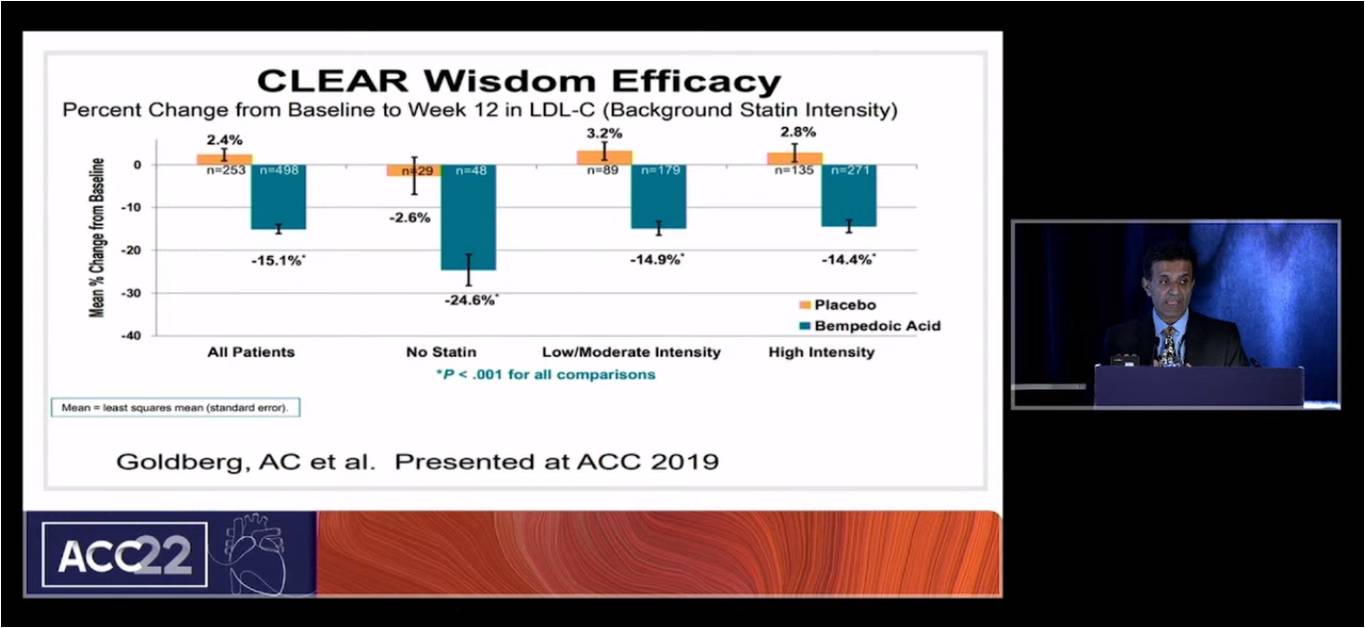
Virani S, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. In clinical trial setting, as per US guidelines, ~55% patients with high intensity statin treatment showed more than 70 mg/dL LDL-C and as per European guidelines, ~75% patients continued to high cholesterol levels. SWEDEHEART exhibited that 87% of patients receiving high intensity statin treatment in which only 17% of patients had LDL-C below 55 mg/dL and with 100% use of statin showed 21% of patients will get cholesterol target level. In USAGE study, 10,318 patients were surveyed via internet. 88% patients were current statin users. Bempedoic acid (BA) acts in the same cholesterol biosynthesis pathway as statins. Elevated LDL are causally associated with initiation and progression of ASCVD and per 38.7 mg/Dl reduction in LDL-C leads to ASCVD relative risk reduction by 22%. As per CLEAR study, Bempedoic acid significantly reduces LDL-C levels as compared to placebo in 2230 patients with no major adverse events except the increase in uric acid level than placebo. CLEAR study presented at ACC 2019 showed that Bempedoic acid significantly reduced LDL-C level from baseline to week 12 as compared to placebo. Also, Combination of Bemepedoic acid and ezetimibe substantially decreases LDL-C and hsCRP level by 35%. BA is associated with increased risk of tendon rupture or injury with 0.5% in RCT. FDA 2020 has approved Bemepedoic acid and Bemepedoic acid plus ezetimibein for the treatment of heterozygous familial hypercholesterolemia (HeFH) or established ASCVD.
Studies showed 15 to 25% LDL-C reduction on background of statin and higher LDL-C reduction in patients not on statins. Combination of bemepedoic acid and ezetimibe lowers LDL-C by 35%. Also, Bempedoic acid had good safety profile overall with small incidence of tendon rupture and increase in uric acid. The CV outcome studies of the drug is pending.
Antihypertensive Therapy for Mild Chronic Hypertension Improves Pregnancy Outcomes: A Pragmatic Multicenter RCT
Tita ATN, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022 which evaluated the hypothesis that therapy of mild Chronic hypertension (CHTN) vs. no treatment decreases the frequency of adverse pregnancy effects and is safe for the fetus.
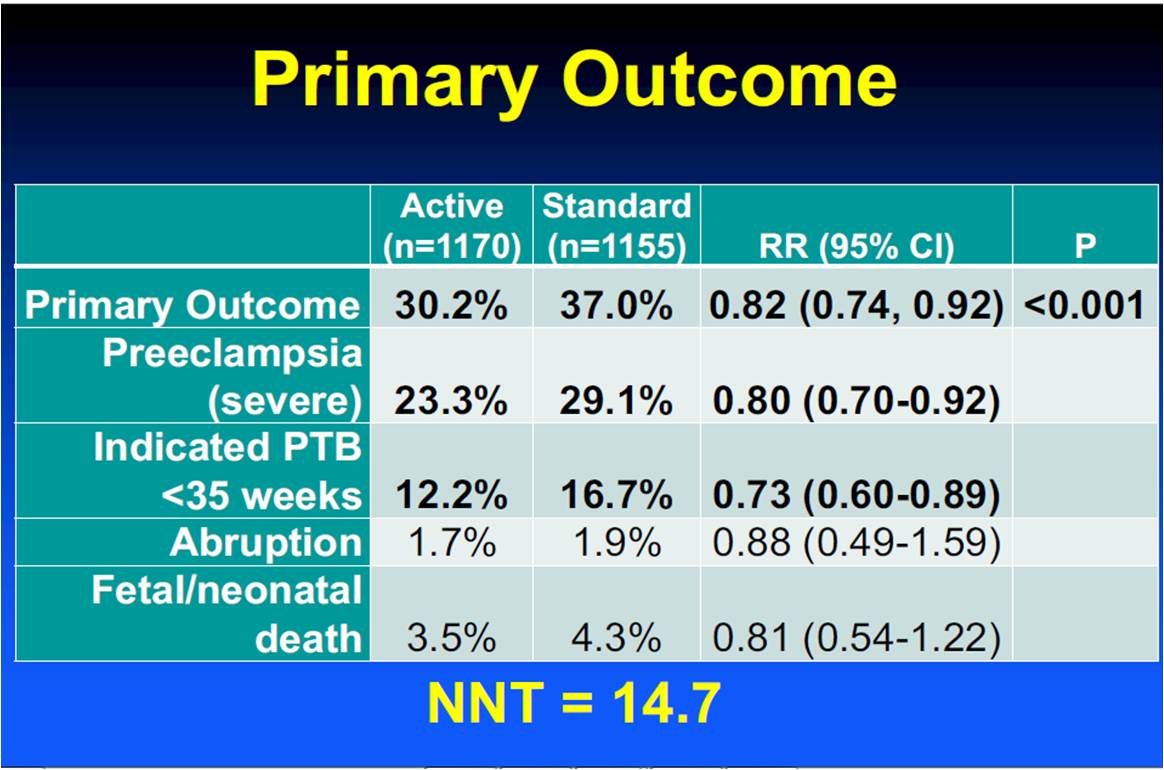
Women with mild CHTN, singleton and <23 weeks’ gestation were enrolled in the CHAP trial, an open-label multicenter RCT. Participants (center-stratified) were randomized to either treatment (with a first-line antihypertensive for pregnancy to a BP goal <140/90) or no treatment unless BP≥160/105. The centrally adjudicated primary outcome was a composite of preeclampsia with severe features, preterm birth <35weeks, abruption and neonatal/fetal death. The safety outcome was small-for-gestational age (SGA; birth weight (<37weeks) and preeclampsia. 2408 participants were effectively randomized to treatment (n=1208) and no treatment (n=1200) at 61 sites from 2015 to 2021. Groups were similar at baseline; 56% patients were on antihypertensive at enlistment, 48% Black, 28% NH White, 20% Hispanic, 16% diabetic and mean BMI of 37.6. The treatment group showed lower incidence of primary outcome as compared to standard group. Both groups showed similar SGA <10th and <5th percentile. The treatment group exhibited reduced frequency of preeclampsia and preterm birth. Primary results did not vary by therapy status prior to enlistment (p=0.115), race-ethnicity (p=0.609), BMI categories (0.074) or diabetic status (p=0.255).
Mild CHTN treatment in pregnancy to a BP goal <140/90 decreases a composite of adverse pregnancy outcomes (NNT= 14.7) and does not harm fetal growth. CHAP supports treatment of CHTN to BP<140/90 mmHg in pregnancy with continuation of established antihypertensive treatment. Long-term studies will further clarify treatment effects in maternal and childhood outcomes.
Dietary Management of Disorders of Lipid and Lipoprotein Metabolism in Youth
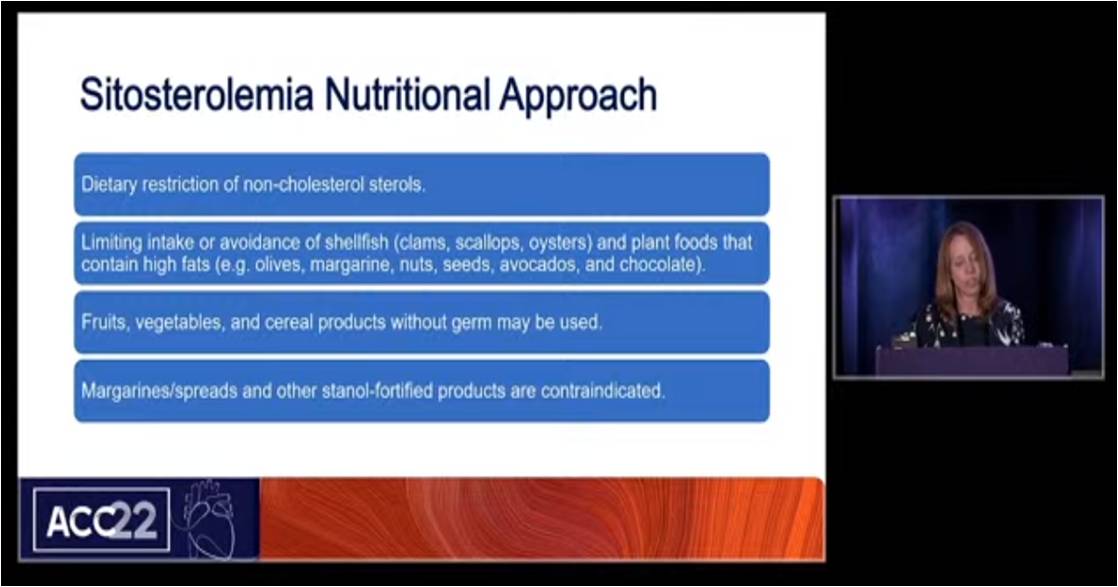
Liebeskind A, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. The objectives of the study were to identify genetic and acquired lipid disorders that may present in childhood and adolescence, discuss nutrition change that may benefit children with specific lipid disorders and incorporate healthy eating principles for all children to prevent acquire lipid disorders. Familial hypercholesterolemia (FH) is a genetic disorder characterized by moderate to severe elevation in LDL-C that increases chance of CHD. Lipid lowering medications are generally required in addition to focused nutrition and activity in order to reach optimal lipid goals. To acquire nutritions in FH, patients must reduce saturated fat to <7% daily calorie intake (8-20 g/day), avoid trans fat with <200 mg dietary cholesterol daily and increase dietary soluble fiber. Familial combined hyperlipidemia (FCHL) may present as elevated LDL-C, hypertriglyceridemia, mixed hyperlipidemia. FCHL may present in childhood generally in association with metabolic conditions such as T2DM. Nutrition recommendations are similar to those for FH with additional recommendation of reduce simple carbohydrate. Sitosterolemia is an inherited disorder of hyperabsorption and decreased biliary excretion of non-cholesterol sterol leads to accumulation of serum levels. In sitosterolemia nutritional approach, patients should restrict non-cholesterol sterols, limit intake or avoidance of shellfish. Fruits, vegetables and cereal products without germ may be used. Obesity is the most common cause of lipid disorders in children leads to mild to moderate hypertriglyceridemia. To start nutrition for youth, patient’s growth charts, medical history, causes should be reviewed. The child’s current nutritional status should be understand and review the entire family’s readiness to change. Patient’s adequate nutrition status and focus on positive reinforcement should be ensured.
Most Lipids disorders in children are associated with obesity and overweight status. Nutrition and physical activity to reach a healthy weight is essential. For LDL-C related disorders, mediations will likely be needed but a diet lower in saturated fat and higher in fiber can assist. For TG-related disorders, medications are less likely to achieve optimal goals and focused nutrition and physical activity is a mainstay. Dietary recommendations for most youth should emphasize fruits, vegetables, whole grains and varied protein foods. Avoiding added sugar in foods and beverages is always the right answer. Small lifestyle changes made in youth can impact total cholesterol years.
Management of Dyslipidemia During Reproductive Years
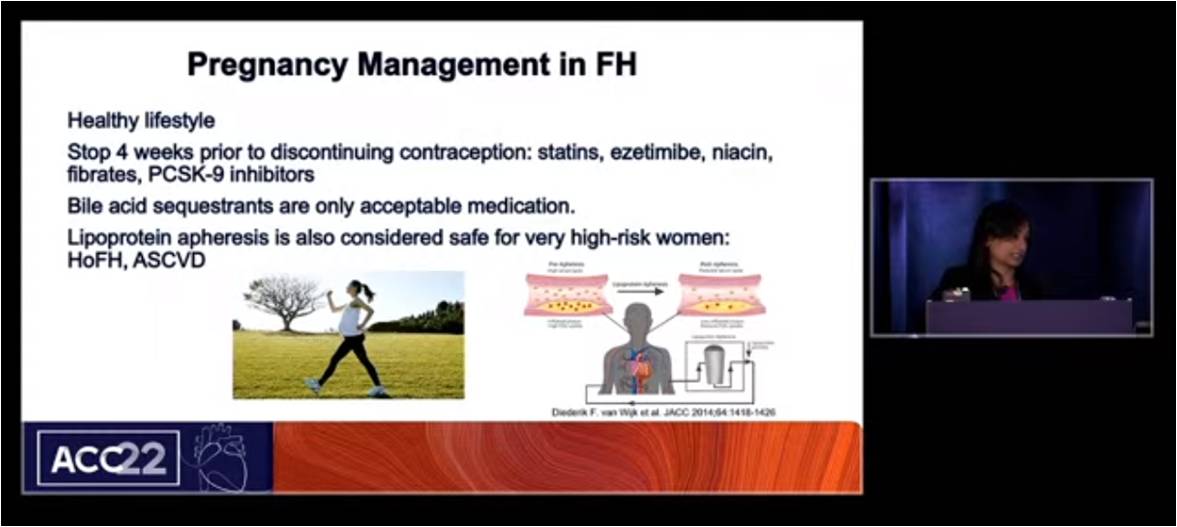
Mehta S, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. 8 out of 10 women of childbearing age have never had their cholesterol levels checked, despite clear guidelines to get a first lipid blood test early in adulthood. Previously statins are considered as X category in pregnancy. FDA requests removal of strongest warning against using cholesterol-lowering statins during pregnancy. But it is still advises most pregnant patients should stop taking statins. Breastfeeding not recommended in patients who require statins. The women with FH showed higher increase in LDL-C level during pregnancy as compared to non-FH women. Pregnancy management in FH considered with healthy lifestyle and stop statins, ezemtimibe, niacin, fibrates, PCSK9i 4 weeks prior to discontinuing contraception. Bile acid sequestrants are only acceptable medication. Lipoprotein apheresis is also considered safe for very high risk women.
Hyperlipidemia assessment and management should not be ignored during the childbearing years. Healthy lifestyle is the key for all patients during their lifetime. Women with FH do benefit from medications and possibly apheresis, however the choice does vary based on pregnancy and lactation status.
Bentracimab Immediately and Significantly Reverses the Antiplatelet Effects of Ticagrelor in Older People
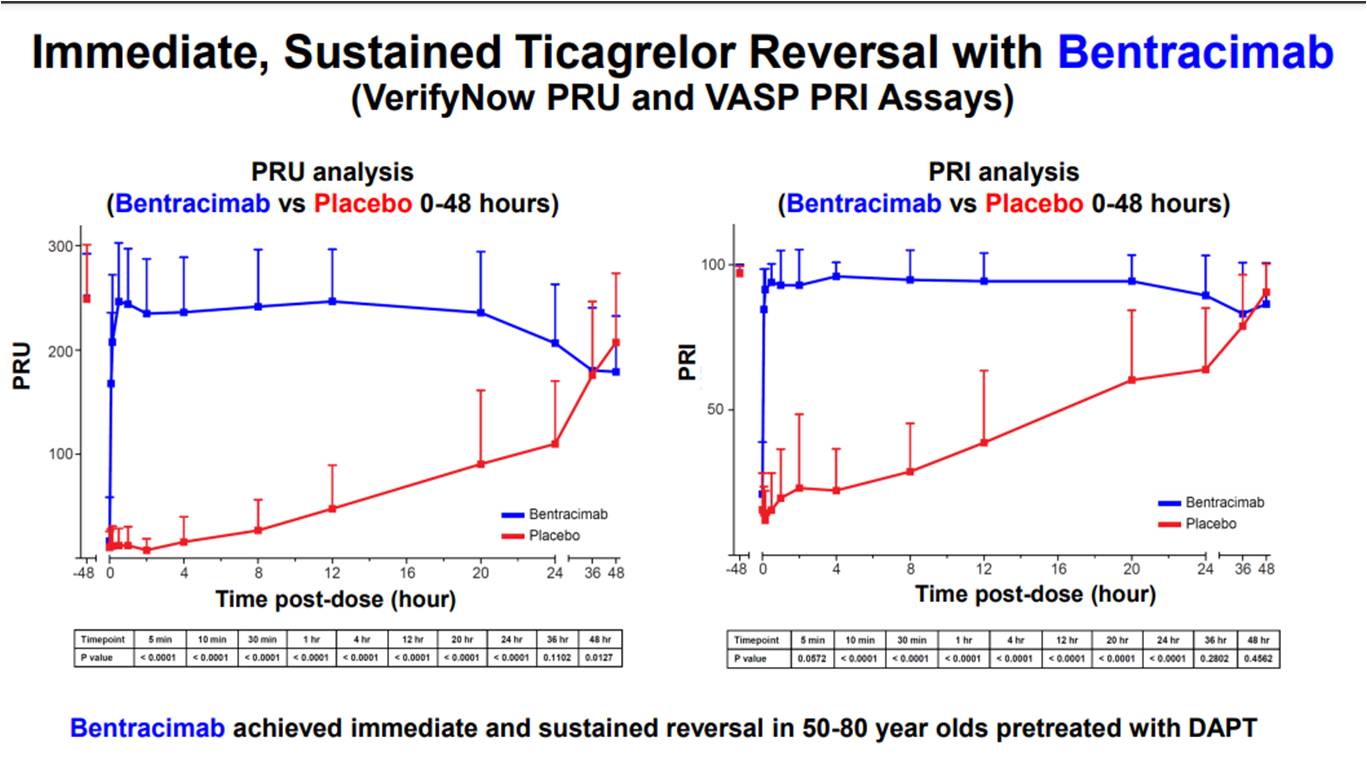
Bhatt D, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. Ticagrelor is an efficacious antiplatelet agent however if bleeding happens there is no way to reverse it. Bentracimab is a human monoclonal antibody fragment outlined to bind ticagrelor.
A double-blind, placebo-controlled, Phase 2b trial in which participants aged 50-80 years pre-treated with ticagrelor and aspirin were randomized to bentracimab bolus plus infusion or placebo. The primary outcome was percent platelet inhibition as evaluated with the VerifyNow PRU test, and the secondary outcome was percent platelet inhibition using the VASP PRI test, both evaluated via 4 hours post dose.
205 participants were enlisted in the study (154 randomized to bentracimab, 51 to placebo). The primary and secondary outcome each demonstrated highly substantial reversal of ticagrelor’s impact (p<0.0001 and p<0.0001, respectively). Platelet function was restored to fundamentally baseline immediately following the bolus, with an impact that was sustained all over the period of infusion. No incidence of platelet rebound was seen evaluated using p selectin levels or mean platelet volume. 37.7% of bentracimab and 41.2% of placebo patients showed at least one treatment-emergent adverse event; none were contemplated associated to bentracimab in the blinded trial.
Bentracimab significantly restored platelet function as measured by multiple assays by binding and eliminating free ticagrelor and ticagrelor active metabolite as compared to placebo. No thrombotic events and no SAEs reported in volunteers randomized to Bentracimab, confirming the safety profile. Bentracimab appears to be a very promising option for ticagrelor reversal.
How Should We Treat Large Thrombus Burden in 2022? (STEMI)
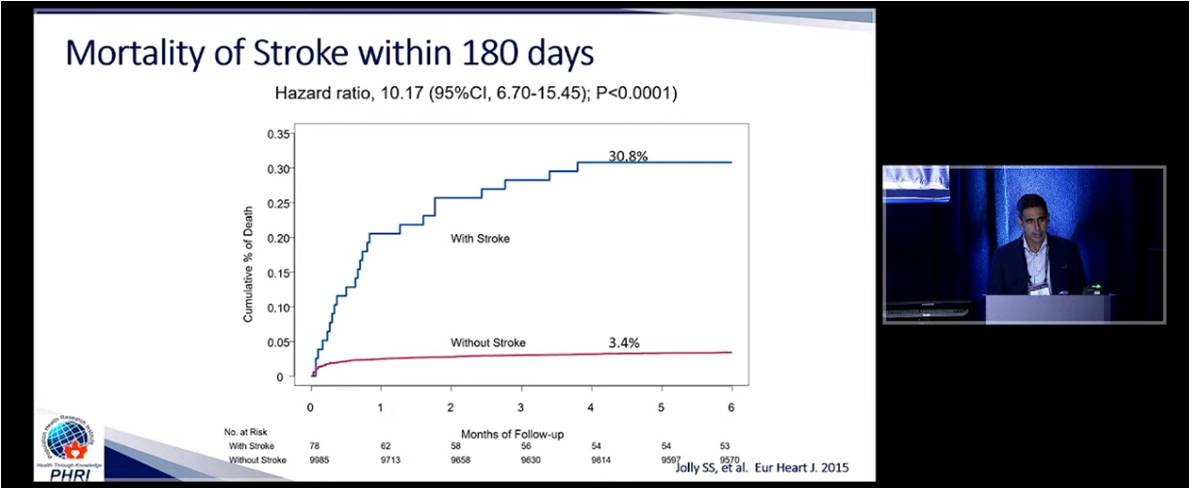
Jolly S, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. In TOTAL study, 10,700 STEMI patients with primary PCI ≤12 hours of symptom onset were enrolled. Patients were equally randomized to manual thrombectomy or PCI alone. Primary outcome was CV death, MI, cardiogenic shock and class IV HF ≤180 days. Patients with thrombectomy showed lesser rate of primary outcome as compared to patients with PCI alone. Patients with stroke showed significantly high rate of death (30.8%) as compared to patients without stroke (p<0.0001). As per ACC/AHA guidelines update, class III indication is for routine thrombus aspiration and class IIb indication for bailout or selective aspiration due to lack of data. In individual Patient Meta analysis of 19,047 patients, thrombectomy showed lower rate of CV death as compared to PCI alone treatment (p<0.16). In patients with high thrombus burden, routine TIA was associated with lower CV death but higher stroke or TIA at 30 days with no difference in mortality at 1 year. CAT RX technology showed 99.5% patients with grade 0 final TIMI thrombus and 97.5% patients with grade 3 final TIMI flow and 99.85 patients with myocardial blush. CHEETAH study showed significant reduction in CV death as compared to thrombectomy and PCI alone treatment.
Manual thrombus aspiration should not be done routinely. Routine thrombus aspiration decreases CV death in patients with high thrombus burden. CAT RX technology can provide satisfactory results in thrombectomy.
Antithrombotic Management in AF Patients Undergoing PCI: What Do Consensus and Guidelines Say?

Collet JP, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. Jean-Philippe Collet stated that there have been changes between 2018 and 2020 in the guideline recommendations for antithrombotic management of patients with atrial fibrillation undergoing percutaneous coronary intervention.
Recommendations for combining antiplatelet agents and anticoagulants in patients with non-ST-segment elevation acute coronary syndrome requiring chronic anticoagulants:
- Stroke prevention is recommended in atrial fibrillation patients with >1 non-sex CHA2DS2-VASc stroke factor (score of >1 in males or >2 in females).
- For patients with 1 non-sex stroke factor oral anti-coagulants should be considered and treatment may be individualized based on net clinical benefit and consideration of patient values and preferences.
- An early internal carotid artery should be considered in patients at risk for high bleeding, irrespective of anti-coagulant exposure, to expedite treatment allocation (medical vs. PCI vs. CABG) and to determine the optimal antithrombotic regimen.
New key recommendations for antithrombotic treatment include the following:
- In patients with atrial fibrillation, after a short period of triple antithrombotic therapy, double antithrombotic therapy is recommended as the default strategy using a new oral anticoagulant at the recommended dose for stroke prevention and single oral antiplatelet agent (preferably clopidogrel).
- Double antithrombotic therapy with an oral anticoagulant and either ticagrelor may be considered as an alternative to triple antithrombotic therapy with an oral anticoagulant, aspirin, or clopidogrel in patients with a moderate or high risk of stent thrombosis, regardless of the type of stent used.
New oral anticoagulants should be preferred over of vitamin K antagonists if not contraindicated; aspirin should be used up to one week post PCI and up to one month in case of high thrombotic risk and acceptable bleeding risk; a combination of new oral anticoagulant plus oral P2Y12 inhibitor with aspirin use limited to the peri-PCI period should be the default strategy.
Prognostic Significance of Pulmonary Hypertension in Patients with Obstructive Hypertrophic Cardiomyopathy after Septal Myectomy
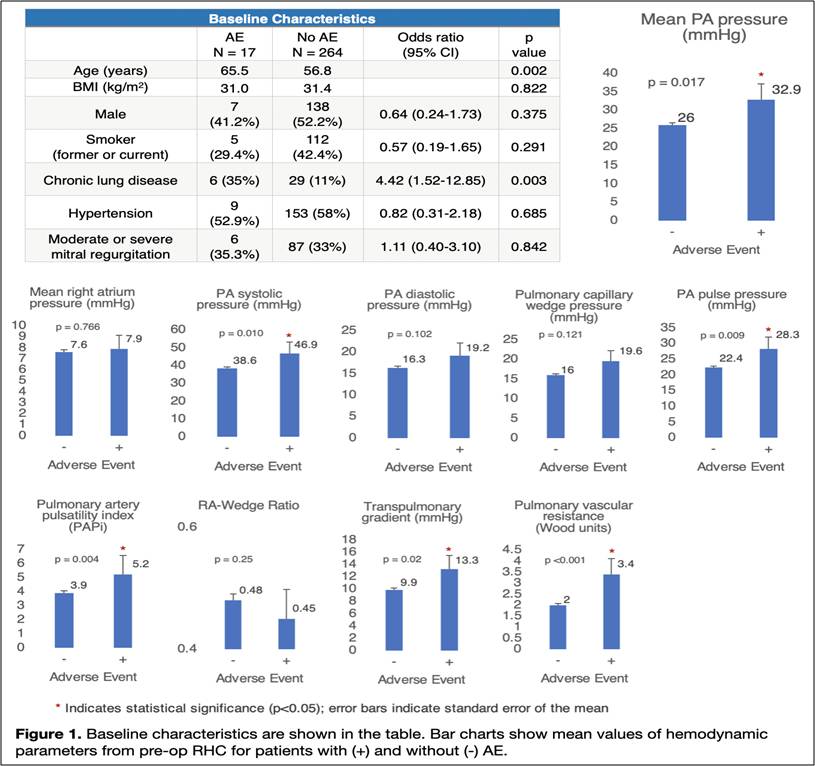
Lee A, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022. The patients with hypertrophic obstructive cardiomyopathy (HOCM) often are associated with concomitant pulmonary hypertension (PH). The study hypothesised that concomitant PH results in increased risk for short-term adverse outcomes after septal myectomy (SM).
A retrospective analysis of 758 patients who underwent SM for HOCM between 2010 and 2020 were evaluated. After excluding patients without pre-op right heart catheterization (RHC) or incomplete RHC data, final sample included 281 patients. Definition of adverse events included composite endpoint such as post-op stroke, TIA, MI, cardiac arrest, prolonged ventilation, reintubation, pneumonia, multi-organ failure and mortality and comparison was made between patients with and without AE.
The results of this study shows that the overall incidence AE was low (n=17, 6%). Among the adverse events (AE), prolonged ventilation was the most common (n=9, 3.2%). It was also found that patients with AE were older (64 vs 57, p=.015) and they were more likely to suffer from chronic lung disease (OR 4.42, 95% CI 1.5-12.8, p=.003). Patients with AE experienced greater pulmonary artery (PA) systolic pressure, mean PA pressure, PA pulsatility index, PA pulse pressure, transpulmonary gradient and pulmonary vascular on pre-op RHC.
The study concludes that increased severity of concomitant PH in HOCM patients who are undergoing SM results in increased risk of short-term AE. Before SM, screening for and treating PH can reduce the risk of complications.
Higher Cumulative Systolic Blood Pressure is Associated with Poorer Left Atrial Function in the Absence of Left Atrial Enlargement: The Atherosclerosis Risk in Communities (ARIC) Study
Left atrial (LA) function disability can predate LA enlargement and is correlated with adverse cardiovascular disease (CVD) effects. There is no information regarding risk factors for poorer LA function with normal LA size. Hof JV, presented a study in a session at American College of Cardiology (ACC) on 2nd April, 2022 which analyzed the hypothesis that higher cumulative systolic blood pressure (cSBP) is correlated with poorer LA function absent of LA enlargement in ARIC, a community-based cohort study.
3,870 participants (mean age 75 [SD 5] years, 61% female, 19% Black) were assessed excluding those with LA volume index >34 ml/m2 and prevalent atrial fibrillation at ARIC visit 5 (2011-13). 2D speckle tracking echocardiography was used to estimate LA function at visit 5. cSBP over 24 years was measured by averaging SBP at visits 1-5, standardizing by time among visits. Linear regression was used to analyse correlations among cSBP and LA function.
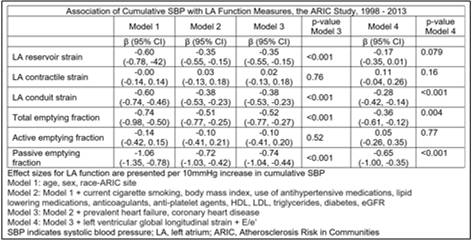
Higher cSBP was correlated with worse LA reservoir and conduit strain, and total and passive emptying fraction following adjusting for demographics and CVD risk factors. All correlations remained substantial after additional adjustment for LV function, except for LA reservoir strain. cSBP was not substantially correlated with LA contractile strain and active emptying fraction.
Higher cSBP is correlated with poorer LA function even in the absence of LA enlargement and independent of LV function. The results underscore SBP as a prevention target and justify additional research to estimate whether SBP decrease inhibits LA function reduction.

