Givertz MM, et al. J Am Coll Cardiol. 2019 Nov 5;74(18):2295-2312.
Givertz MM, et al., conducted a review to explain advanced heart failure therapies for congenital heart disease patients which includes the general approach to estimate and manage, before and after operative care, predicted short- and long-term outcomes, and future aspects for clinical care and research.
General approach
As suggested by the Heart Failure Society of America, in spite of best medical, surgical, and device therapy, stage D advanced Heart failure (HF) known as the occurrence of progressive and/or consistent intense HF signs and symptoms. Essentially, this functional rejection should be initially undertaken by the HF syndrome demonstrated as alteration in signs and symptoms, laboratories, and hemodynamics (Figure 1).
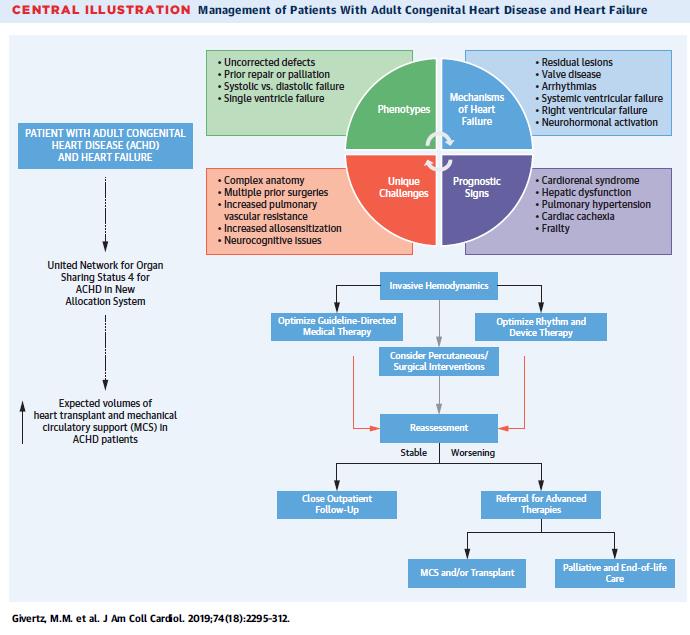
Figure 1: Management of Patients with Adult Congenital Heart Disease and Heart Failure
Various markers of progressive disease and inadequate prognosis must assist as triggers for considering estimation for advanced therapies (Table 1).
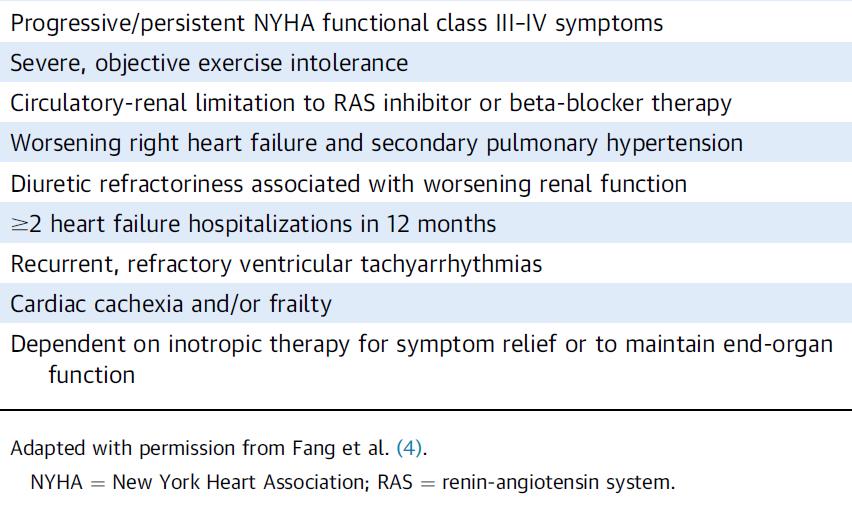
Table 1: Clinical Triggers to Consider Referral for Advanced Therapies
Heart transplant
Heart replacement treatment transformed into the standard of care for end-stage HF patients following the initial statement of successful cardiac transplantation >50 years ago. Almost 1.9% of 48,776 heart transplants were conducted for congenital heart disease (CHD) registered to the International Society for Heart and Lung Transplantation (ISHLT) registry in the period of 1992 and 2003. This percentage has risen to 3.1% of 37,703 patients in the period of 2009 and 2017, among them substantially 40% of patients had single ventricle physiology (Figure 2).
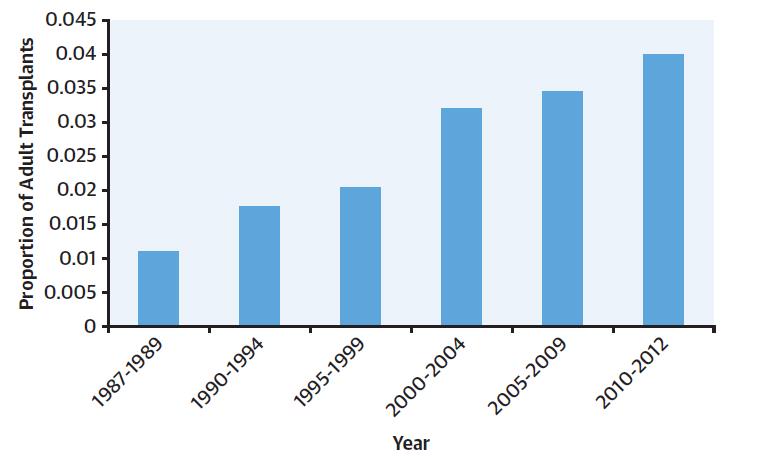
Figure 2: Proportion of ACHD Transplants
While bounding interpretations to patients surviving at least 1 year, dominant long-term outcomes were observed in CHD patients with a median survival of 20.1 years vs 4.4 and 12.0 years in patients with cardiomyopathy and coronary artery disease, respectively (Figure 3).
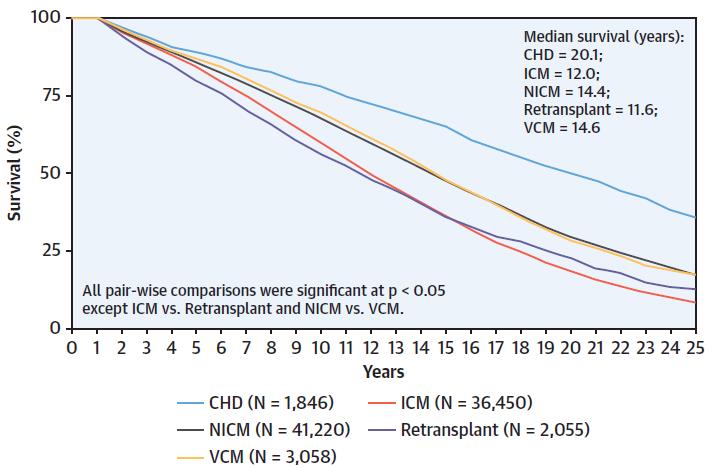
Figure 3: Heart Transplant Conditional Survival by Diagnosis
Karamlou, et al., desired to estimate the impact of single ventricle physiology on death following heart transplant in CHD patients. Significantly higher in-hospital mortality was observed in single ventricle patients (23% vs. 8%; p < 0.001) (Figure 4).
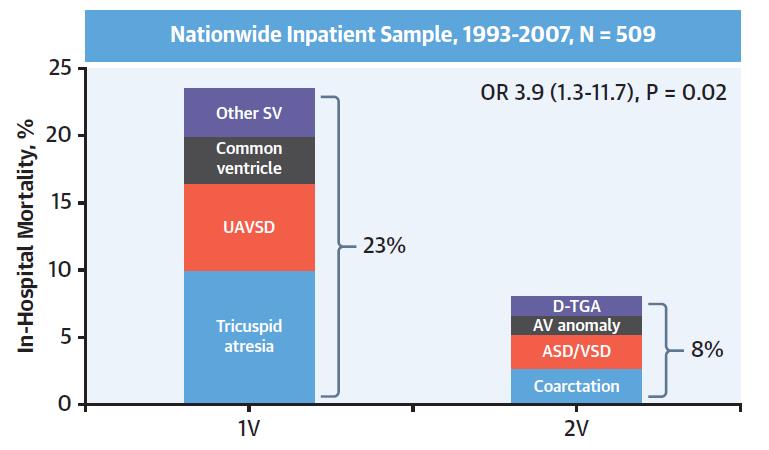
Figure 4: Impact of Single Ventricle Physiology on Death after Heart Transplant
Mechanical Circulatory Support
The HeartMate II left ventricular assist device (LVAD) was the prime continuous-flow LVAD approved in 2008 as connection to transplant. Consequently, the HeartMate 3 LVAD and HeartWare HVAD centrifugal flow pumps have become cornerstone for long-term support. During this period, there has been a gradually and significant rise in the numbers of devices embedded and the percentage of patients connected to transplant with mechanical circulatory support (MCS). During the same period, it was also observed that proportion of patients increased with adult congenital heart disease (ACHD) successfully supported with MCS (Figure 5).

Figure 5: Proportion of ACHD Transplants Supported With Mechanical Circulatory Support
The pediatric component of INTERMACS, Pedimacs, gathers details on patients age <19 years during MCS implant. In the overall population, CHD was the essential diagnosis in 21%, among these 62% had single ventricle anatomy with >90% have experienced before operation. Patients with CHD showed poor survival rate as compared to patients with cardiomyopathy suffering MCS implant.
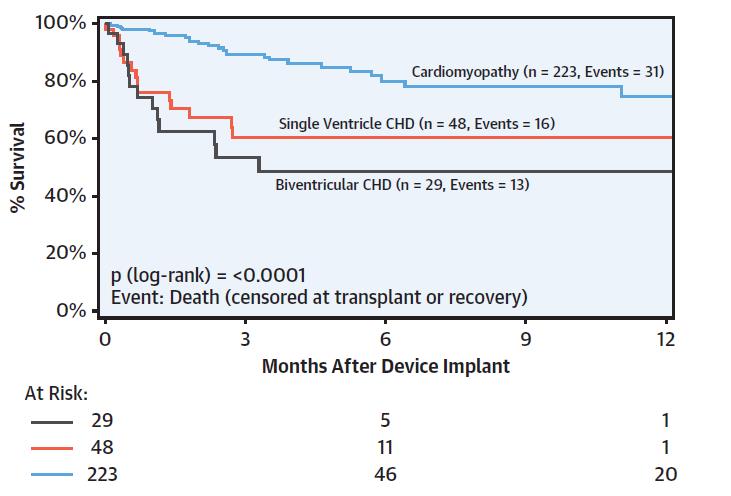
Figure 6: Survival by Etiology of Heart Disease in Pedimacs
Despite identical morbidity, patients with ACHD showed superior mortality rate than non-ACHD patients (p = 0.003) (Figure 7A). This was principally interpreted by rising number of death in the prior 5 months after implantation encompassing operative and perioperative factors. Comparing outcomes assessment for patients with ACHD (Figure 7B) showed that 52.3% were survived with device in place, 27.6% had passed away, and 20.1% had been transplanted at 12 months.
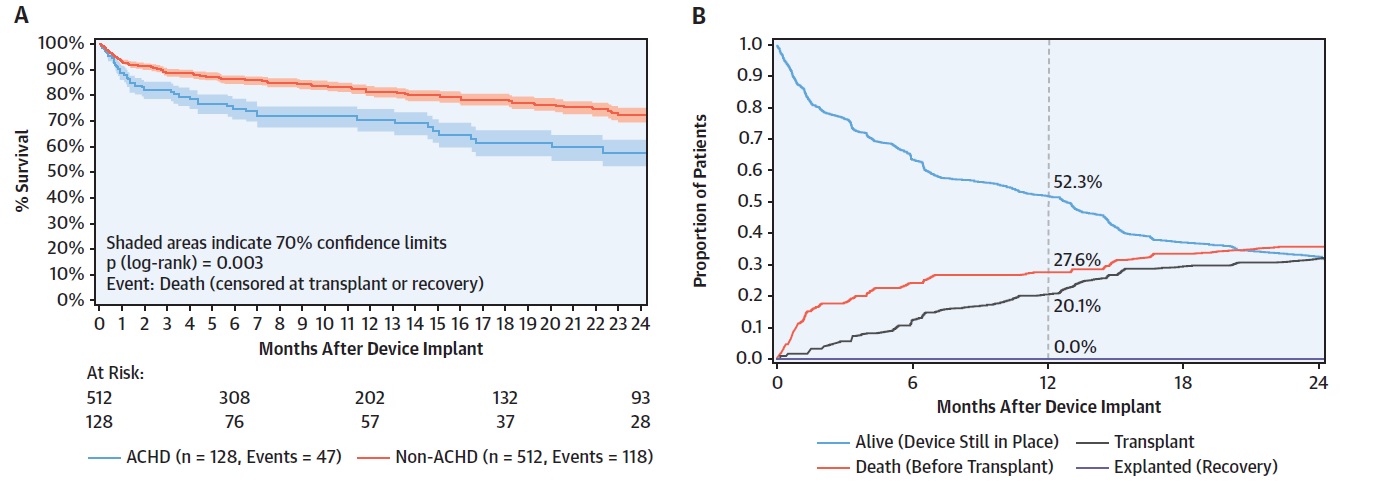
Figure 7: Outcomes Following Mechanical Circulatory Support in ACHD, Kaplan-Meier analysis (A) of overall mortality comparing adult congenital heart disease (ACHD) and non-ACHD patients in blue and red, respectively, as well as competing outcomes analysis (B) for ACHD patients.
Thus, survey of patients with ACHD showed that maximum 70% of patients are eager to contribute in advanced care planning and >90% would prefer to discuss with a palliative care specialist. Palliative care specialists that are lined up with MCS/transplant teams may perform an essential task in tackling the exceptional requirement of ACHD patients, especially in terms of their younger age, “survivor” intellect, and complicated relationship with aging parents and long-term medical providers.

