Agbor VN, et al. Cardiovasc Diagn Ther 2019;1-8.
Agbor VN, et al., conducted a review article to address recent data on the demographic and clinical characteristics, aetiologies, treatment, economic burden and outcomes of HF in low- and middle-income countries (LMICs).
Clinical characteristics and aetiologies of HF in LMICs
As compared to HF patients in high-income countries (HICs) with mean/ median age of 70 years, HF Patients in LMICs are probably younger with a mean/median age of 63 years and it seems to be develop from 52 years in Africa to 70 years in South America. Certainly, as per country economic index the mean age of admission for HF raises. Whereas, CVD patients who are protected and economically secured have improved their health and favourably managed their condition and will only promote ultimate complications in their later age.
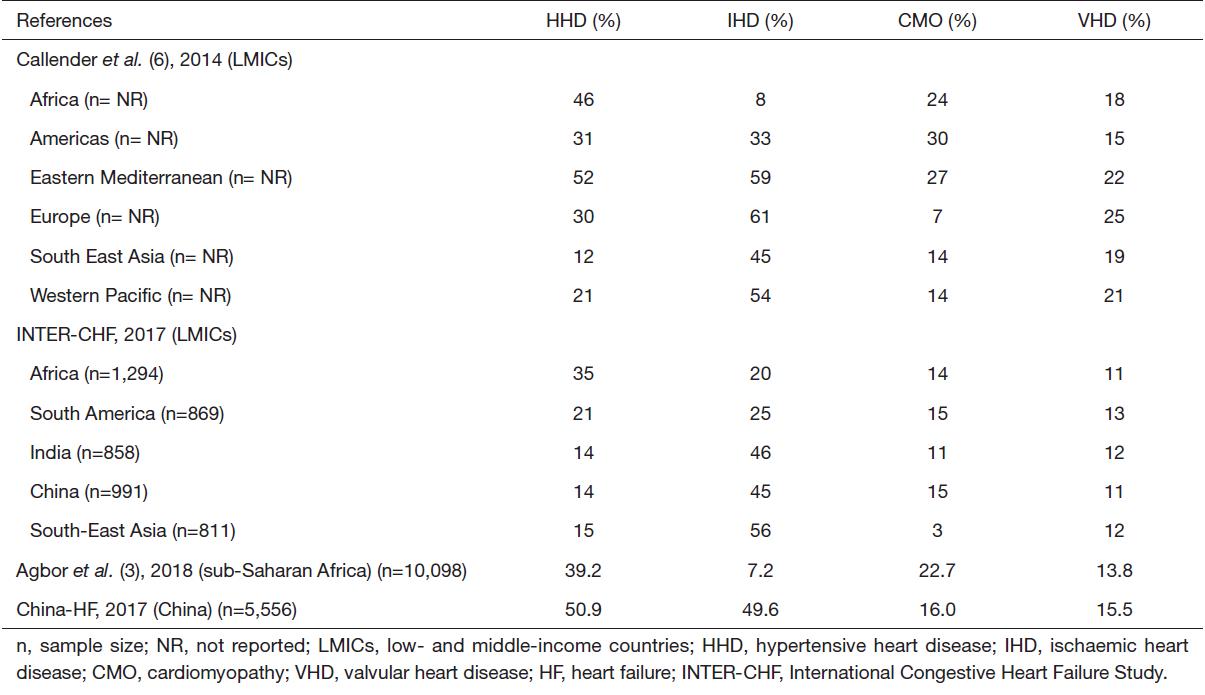
In LMICs, the four well-known causes of HF are ischemic heart disease (IHD), hypertensive heart disease (HHD), cardiomyopathies (CMOs) and rheumatic heart disease (RHD). Importantly, in most LMICs, hypertension, CMOs and RHD are more common in Africa and IHD which is the dominant root of HF seem to be less common. Apart from African counties, many other LMICs like South America, Eastern Mediterranean and even Europe endure a huge significance of HHD. In LMICs, prevalence of 3–30% CMOs and 11– 5% RHD are also essential causes of HF. In LMICs, hypertension, valvulopathies (either primary or functional), diabetes mellitus, dyslipidaemia, chronic kidney disease and smoking are the dominant comorbidities correlated with HF (Table 1).
Table 1: Major causes of HF in LMICs
Management of HF in LMICs
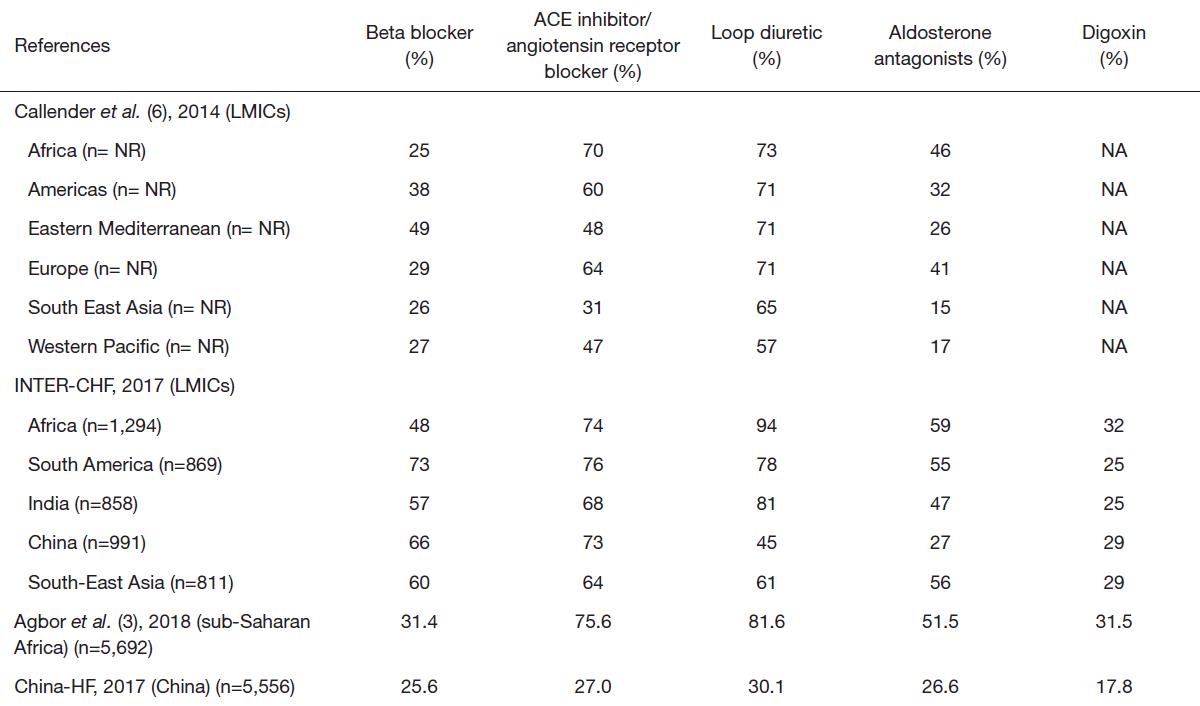
Pharmacological therapy of HF with reduced ejection fraction (HFrEF) depends on the usage of diuretics for the alleviation of congestion-related symptoms and of neurohormonal antagonists—beta-blockers, angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) and mineralocorticoid receptor antagonists (MRAs), which have been proved to enhance survival. In LMICs, the utilisation of medicine for HF alters essentially. To enhance usage of these life-saving medications, strategies comprises of cost containment and promotion of generics, as well as education of physicians on good clinical practice in the management of HF should be included (Table 2).
Table 2: Medications used for the management of HF in LMICs
Outcomes of HF in LMICs
Across LMICs, HF has poor outcomes, correlated with a prolonged hospital stay around 10 days (range, 5–35 days) and 4–25% in-hospital mortality, with the maximum rates being verified in Africa, South America and Asia. In the INTER-CHF study, it was reported that in LMICs, the overall one-year mortality rate for HF was 16.5% with Africa and more than 50% of the disease burden with India.
Economic burden of HF in LMICs
In most of LMICs, the worldwide goal in decreasing CVD mortality by 25% by the year 2025 seem to be doubtful especially due to poor governance, inadequate distribution of public funds to the health sector, shortage of evidence-based and inefficient delivery of healthcare including disease prevention, low levels of awareness, and lack of universal health coverage, among others. Almost 25–56% of the total direct cost of HF management is associated with the rate of inpatient care. As compared to HICs, most of the patients in LMICs exhibited with acute decompensated HF are not able to afford management costs which therefore results in higher rates of in-hospital mortality due to high costs of inpatient care for HF, low health insurance rates and almost absence of universal healthcare.
Thus, as compared with patients in HICs, latest evidence reported the dangerous appearance of HF in LMICs with compelling differences in sociodemographic and clinical profiles. HHD, IHD, RHD and CMOs are the four prominent root of HF in LMICs. In LMICs, Infection remains an essential factor to the evolution of HF. It is necessary to enhance the utilisation of analysis on and the utilisation of evidence-based medications such as ACEIs, ARBs, beta blockers and MRAs to contribute in invasive management of HF. Finally, for the advance understanding of the HF epidemiology in LMICs, large scale cohort and national HF registries are authorized.

