Stepanova N. Open Access Maced J Med Sci.2019 Aug 15; 7(15):2467-2473.
Peritoneal dialysis (PD) is a well-established way of treatment for ESRD patients. There are several factors such as age, the presence of diabetes, residual renal function (RRF), glucose degradation products, peritonitis, chronic inflammation, cardiovascular diseases (CVD) influencing PD technique survival. In PD patients, the most common causes of death are CVD because of the traditional and non-traditional risk factors. Dyslipidemia is a traditional risk factor of cardiovascular (CV) events in the general population and the HD population. It is still not clear whether dyslipidemia is correlated with PD technique survival. It was hypothesised that if all factors mentioned above correlated with dyslipidemia in PD patients were exhibited as loss of peritoneal function, then PD technique survival could not be correlated with dyslipidemia itself. Stepanova N. et al., conducted a prospective observational study to analyse whether dyslipidemia was correlated with PD technique failure.
Between January 2010 and September 2016, the prospective single-centre observational study was carried out with 40 outpatients with ESRD on PD (27 males, 13 females). Continuous ambulatory PD (CAPD) was given to all patients for more than 3 months. They were observed to analyse the effect of atherogenic lipid profile on PD technique survival in the 36-month- follow-up period. Haematological parameters of blood were calculated by an ABX Micros-60. The adequacy of dialysis was calculated by estimating the total weekly creatinine clearance (CrCl) (it was normalized to 1.73 m2 of the body surface area) and total weekly urea clearance (Kt / V) with the Watson formula for measuring body water. The 3-year PD technique survival rate dichotomised was the primary endpoint according to atherogenic dyslipidemia status. As per the atherogenic dyslipidemia presence at baseline, the patients were categorised into 2 groups. Group I comprised of 28 patients with atherogenic dyslipidemia and Group II had 12 patients without atherogenic dyslipidemia.
28/40 (70 %) patients showed atherogenic dyslipidemia associated with PD adequacy parameters. The incidence of all-cause PD technique failure was 2 times higher in the patients with atherogenic dyslipidemia as compared to the patients without dyslipidemia: 2/12 (16.6 %) versus 12/28 (42.9 %) (ϰ2 = 2.5; p = 0.12). (Figure 1)
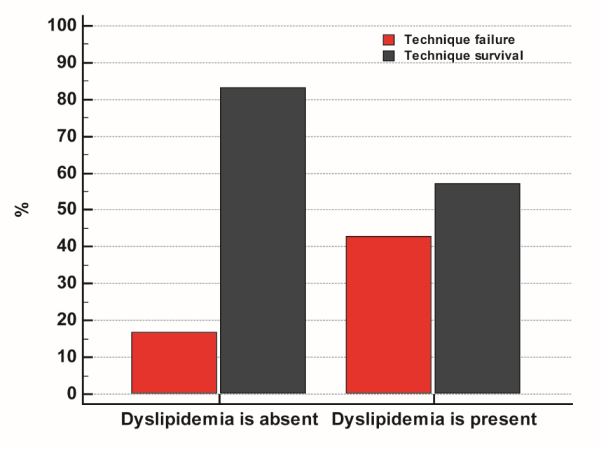
Figure 1: The incidence of all-cause PD technique failure stratified according to atherogenic dyslipidemia status
The patients with atherogenic dyslipidemia exhibited a highly significant difference in technique failure rate as compared to the patients without dyslipidemia in the Kaplan-Meier analysis (log-rank p = 0.02). (Figure 2)
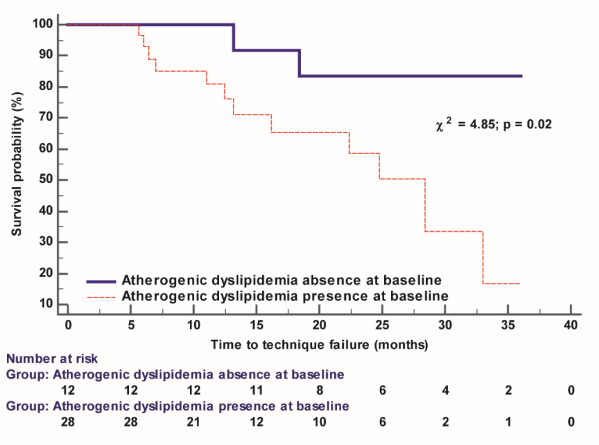
Figure 2: The Kaplan-Meier technique survival curves in PD patients dichotomised according to atherogenic dyslipidemia status
Atherogenic dyslipidemia at baseline was substantially correlated with a higher risk of all-cause PD technique failure in the univariate Cox regression model (HR 4.5; 95% CI 1.6 to 12.9; (ϰ2 = 5.5, p = 0.019).
Thus, it was concluded that the presence of atherogenic dyslipidemia was substantially correlated with a greater risk of technique failure in PD patients.

