Zhang YX. Am J Hypertens. 2020 Jan 1;33(1):99-105.
A risk factor in the vulnerability and extremity of pulmonary arterial hypertension (PAH) is sex difference. Female PAH patients showed a high occurrence but greater survival rate as compared to males. In men, the higher estradiol levels are correlated with PAH. Additional studies exhibited that post-menopausal females with PAH had greater estradiol levels and estradiol levels are correlated with extremity of the disorder. Gonadotropins incorporating follicle stimulating hormone (FSH) and luteinizing hormone (LH) closely regulate the release of sex hormones in physiological conditions. But, in recent studies, levels of FSH and LH among male PAH patients and healthy controls are comparable and are not associated with clinical effects. Whether the serum levels of gonadotropins are associated with PAH in fertile females with the involvement of sex differences in PAH, is still unknown. Thus, Zhang YX et al., conducted a study to assess the correlations among gonadotropins and sex hormones with the incidence of idiopathic pulmonary arterial hypertension (IPAH) status and mortality between fertile females.
164 adult females with IPAH and 133 controls with matched age and BMI were enlisted in the matched case-control study. Patients were admitted at Shanghai Pulmonary Hospital (China) in the period of 2008 – 2014 to assess the correlation among gonadotropins, sex hormones and the incidence of IPAH. The right heart catheterization diagnosed IPAH as per the guidelines. Menstrual information was gathered. Menstrual cycle disorders included polymenorrrhea (intervals fewer than 21 days), oligomenorrhea (intervals surpassing 35 days), amenorrhea (absence of a menstrual period), and irregular menstruations (differences in menstrual cycle length of more than 8 days). Patients were followed-up prior to October 20th, 2018. A telephone interview or outpatient clinic visit was done to track the survival status of patients and dates of death.
38 of 164 (23.2%) IPAH females and 21 of 133 (15.8%) controls had menstrual cycle disease. Lower progesterone or lower testosterone levels were correlated with raised mean right atrial pressure (mRAP), pulmonary vascular resistance (PVR), WHO FC, and reduced cardiac index (CI) and 6MWD (all p ≤ 0.001). Substantial higher level of FSH was correlated with reduced CI (p = 0.019). The median duration of follow-up was 77 months. IPAH females with FSH levels over 6.71 mIU/ml (LN [FSH] = 1.90 mIU/ml) had similar age, BMI as compared to patients with lower FSH levels, however worse clinical characters and worse effect (p = 0.004). (Figure 1)
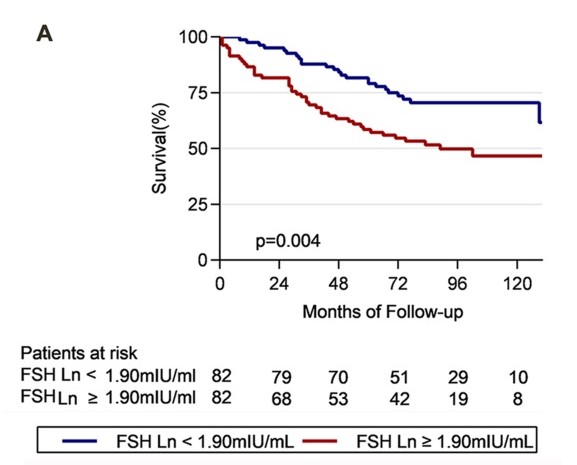
Figure 1: Survival in fertile female IPAH patients in relation to FSH Ln and progesterone Ln. Patients were grouped by median of hormone levels. After a median follow-up of 77 months, survival analyses of FSH (A) progesterone
Substantially worse clinical characters and worse effect were shown in IPAH patients with progesterone levels below 0.26 ng/ml (LN [progesterone] = -1.34 ng/ml) (p = 0.004). (Figure 2)
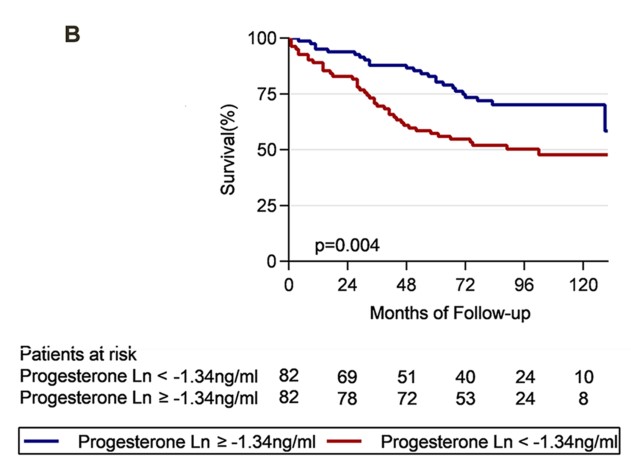
Figure 2: Survival in fertile female IPAH patients in relation to FSH Ln and progesterone Ln. Patients were grouped by median of hormone levels. After a median follow-up of 77 months, survival analyses of FSH (B) combination of FSH and progesterone
Thus, it was concluded that reproductive female with IPAH showed higher plasma levels of FSH, although levels of progesterone and testosterone were lower as compared to controls. High FSH and lower progesterone also exhibited correlation with severe clinical symptoms and greater mortality between patients.
WHO FC: World Health Organization Functional Classification; 6MWD: Six-minute Walk Distance

