Liu Y, et al. J Cardiol. 2020 Jan;75(1):60-65.
Worldwide, coronary artery disease (CAD) is a leading cause of mortality and morbidity. Inflammation plays a pivotal role in CAD. According to many studies, high-sensitivity C-reactive protein (hs-CRP) is a characteristic and frequently used biomarker of inflammation and is related to the primary and secondary prevention of CAD. Lui Y, et al., conducted a prospective, observational study to investigate the association between hs-CRP on admission and severity of CAD as well as their impact on long-term outcomes in patients undergoing percutaneous coronary intervention (PCI).
A total of 10,020 patients with PCI treatment were divided into three groups based on hs-CRP on admission: 0–3 mg/L (n=6978, 69.6%), 3.01–10 mg/L (n=1997, 19.9%), and >10 mg/L (n=1045, 10.4%). The primary endpoint was major adverse cardiovascular events (MACEs), a composite of all-cause death, myocardial infarction (MI), revascularization, and stent thrombosis. Disease severity was determined by Synergy between PCI wi th TAXUS and Cardiac Surgery (SYNTAX) score (SS).
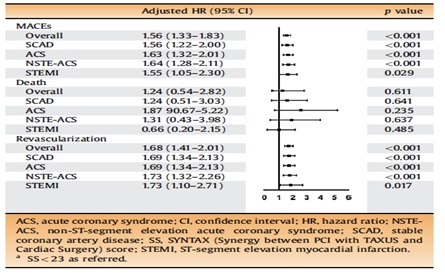
The mean follow-up period was 874 days. Patients with elevated hs-CRP were older, had more risk factors such as hypertension, cerebrovascular disease, chronic obstructive pulmonary disease, and cigarette smoking. Multivariate regression analysis showed that hs-CRP >10 mg/L (OR 1.49, 95% confidence interval 1.21–1.84, p < 0.001), age, previous myocardial infarction, serum creatinine, and left ventricular ejection fraction were independent predictors of intermediate-high SS (>22). Subgroup analysis indicated that the relation between hs-CRP and SS was also consistent in acute coronary syndrome and its subtypes. Although elevated hs-CRP was positively associated with increased rates of MACEs (11.0% versus 12.1% versus 14.3%, p = 0.006), death (1.0% versus 1.3% versus 3.0%, p < 0.001), and revascularization (8.6% versus 10.4% versus 10.0%, p = 0.032), it did not show any prognostic effect for adverse outcomes in multivariate regression analyses (all adjusted p > 0.05). While SS > 22 remained independently predictive of MACEs and revascularization after adjusting confounders, the risks of which were increased by 56% and 68%, respectively.
Thus, the level of hs-CRP is a useful parameter for indicating the severity of CAD evaluated by SS and could aid in risk stratification and prognosis prediction.
Table 1: Performance of SS in multivariate Cox regression models for outcomes