Hermida RC, et al. Eur Heart J. 2019 Oct 22.
Hermida RC, et al., conducted a Hygia Chronotherapy Trial to estimate if administration of the entire daily dose of ≥1 blood pressure medications at bedtime will provide better ABP control and lowers CVD risk than upon awakening ingestion.
Approximately, 19,084 hypertensive patients (10 614 men/8470 women) with mean age 60.5 ± 13.7 years were enrolled in this multicentre, controlled, prospective endpoint trial. Patients were divided in a 1:1 ratio into two groups to administer the entire daily dose of ≥1 blood pressure medications at bedtime (n = 9552) and upon awakening (n = 9532). To assure proper cuff size for office BP measurements (OBPM) and ambulatory BP (ABP) evaluation, at every clinic visit the upper arm circumference was measured. To enhance the reproducibility of results, instead of the most usual 24 h, ABPM was carried out for 48 h, as an authentic estimation of ABP component which includes mean BP values and dipping classification and ABPM based CVD risk assessment which rely considerably on ABPM period. During the two consecutive days of evaluation, participants were advised to follow activities with minimal limitations like managing a similar activity–rest schedule and divert themselves from daytime sleep.
As compared to ingesting all medications upon awakening, significant reduction in the hazard ratio (HR) of the primary CVD outcome (adjusted by the only significant influential characteristics of age, sex, type 2 diabetes, CKD, smoking, HDL cholesterol, previous CVD event, asleep SBP mean, and sleep-time relative SBP decline) was observed in patients of the bedtime-treatment regimen [HR= 0.55 (95% CI 0.50–0.61), p< 0.001; Figure 1A]. For the secondary endpoints of stroke, coronary events, and cardiac events analysed separately, significantly greater risk reduction with bedtime treatment were observed (Figure 1A). The bedtime treatment promotes about 45% reduction in primary CVD outcome (Figure 1). As compared to awakening treatment, bedtime treatment provides significantly higher risk reduction mainly for CVD death [HR= 0.44 (0.34– 0.56), p< 0.001], haemorrhagic stroke [0.39 (0.23–0.65), p< 0.001], heart failure [0.58 (0.49–0.70), p< 0.001], and peripheral artery disease [0.52 (0.41–0.67), p< 0.001; Figure 1B). Significant difference was observed between patients of the bedtime treatment groups and awakening treatment groups in CVD event-free interval for CVD outcome by Kaplan–Meier survival curves (log-rank 140.1; p< 0.001; Figure 2A) and total CVD events (log-rank 174.0; p< 0.001; Figure 2B).
The prospective Hygia Chronotherapy Trial concludes that as compared to awakening treatment, routinely BP-lowering medications intake at bedtime showed an improvement in ABP control (significantly enhanced reduction in asleep BP and increased sleep-time relative BP decline, i.e. BP dipping) and, essentially, considerably declined incidence of major CVD events. The trial also determined that the safety of bedtime hypertension therapeutic scheme is similar with awakening.
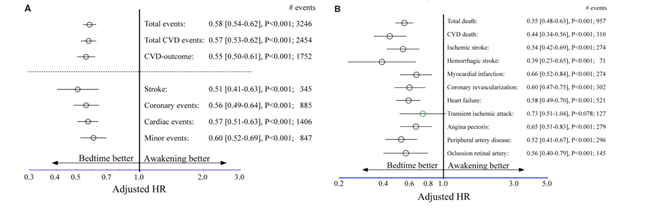
Figure 1: Adjusted hazard ratio of cardiovascular disease outcome as a function of hypertension treatment-time regimen (either upon awakening or at bedtime). (A) Adjusted hazard ratio (95% CI) of primary and secondary composite endpoints. (B) Adjusted hazard ratio (95% confidence interval) for each evaluated single endpoint.
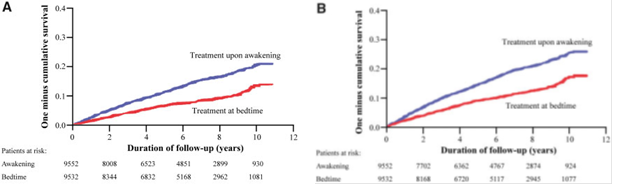
Figure 2: Kaplan–Meier cumulative hazard curves for cardiovascular disease outcome as a function of hypertension treatment-time regimen (either upon awakening or at bedtime). (A) Cardiovascular disease outcome: composite of cardiovascular disease death, myocardial infarction, coronary revascularization, heart failure, and stroke; log-rank: 140.1, p<0.001. (B) Total cardiovascular disease events: composite of cardiovascular disease death, myocardial infarction, coronary revascularization, heart failure, stroke, angina pectoris, peripheral artery disease, and transient ischaemic attack; log-rank: 174.0, p<0.001.

