Trends in Survival after First Myocardial Infarction in People with Diabetes
Weden L
Earlier studies have demonstrated that people with diabetes have a worse outcome after myocardial infarction (MI), compared to people without diabetes. In contrast, recent studies have shown a substantially decline in mortality and cardiovascular (CV) outcome among people with diabetes. Trends in survival after a first MI in people with diabetes and without diabetes is still not extensively studied.
Weden L, presented a session at the European Association for the Study of Diabetes (EASD) Annual Meeting held in Hamburg, Germany on 5th October 2023 which evaluated the trends in survival after a first MI in people with diabetes and without diabetes.
2,527 individuals with type 1 diabetes (T1D), 48,321 individuals with type 2 diabetes (T2D), and 243,170 individuals without diabetes with a first MI in national healthcare registries between 2006 to 2020 were enrolled in the study. Outcomes were trends in survival, i.e. death and CV death, and major cardiovascular events (MACE), i.e. non-fatal stroke, non-fatal MI, CV death and hospitalised heart failure. Multivariable-adjusted proportional hazards ratio (HR) models with 95% confidence intervals (CIs) were separately applied within people without diabetes (control group) and people with T1D, and T2D, with a maximum follow-up period of 1095 days. HRs were estimated in three-year blocks, as well as continuously by the date of entering the cohort.
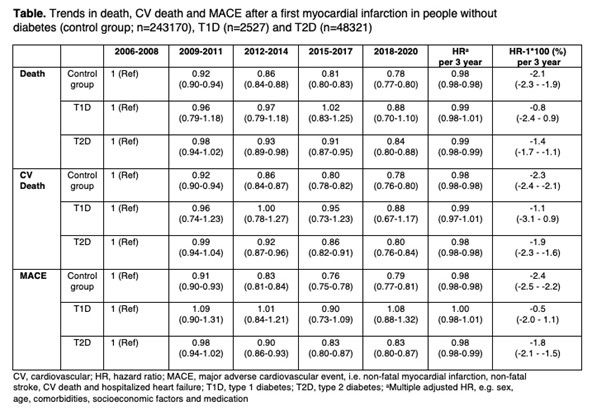
The results showed that the individuals with T1D were younger (62 years, SD ±12.2) and more often women (43.6%) compared to individuals with T2D (75 years, SD ±10.8) women (38.1%), and to control group without diabetes (73years, SD ±13.2) women (38.1%). Proportion of ST-elevated MI (STEMI vs. Non-STEMI) between groups were T1D (29% vs 71%), T2D (30% vs 70%) and control group (39 vs 61%), respectively. Three-year trends in death, CV death and MACE between groups are shown in the Table. During follow-up and after multiple adjustments (sex, age, comorbidities, socioeconomic factors and medication) there was a significant decreased annual incidence trend (HR-1 * 100 %) for all cause death in control group -1.9% (-2.1 to -1.7%) and individuals with T2D -1.3% (-1.7 to -0.9%), with no such trend in individuals with T1D 0.0 (-1.9 to 1.9%). Corresponding numbers for CV death were for control group -2.0% (-2.1 to -1.8%), T2D -1.6% (-2.0 to -1.1%), and T1D -0.5% (-2.6 to 1.2%), and for MACE control group -2.3% (-2.5 to -2.2%), T2D -1.9% (-2.3 to -1.6%) and T1D -0.6% (-2.3 to 1.1%), respectively.
During the last 15 years, the trend in death and MACE in people without diabetes and with T2D having a first time MI has decreased significantly. In contrast, such a decreased trend was absent in people with T1D. This finding highlights the urgent need for understanding the cardiovascular risk in people with T1D.
Acute Myocardial Infarction and Heart Failure in Young Patients with Type 1 and Type 2 Diabetes
Dikaiou P
Type 1 and 2 diabetes are different in several ways but both types are strongly associated with high risk of cardiovascular complications. With rising incidence of type 2 diabetes in adolescents and young adults an increasing proportion of young people with diabetes will be type 2 diabetes. Young-onset type 2 compared to type 1 diabetes has been considered the more lethal phenotype of the two but few formal comparisons between the two types exist.
Dikaiou P, presented a session at the European Association for the Study of Diabetes (EASD) Annual Meeting held in Hamburg, Germany on 5th October 2023, that compared the risk factors between young patients with type 1 diabetes and type 2 diabetes and outcomes with respect to acute myocardial infarction (AMI) and heart failure (HF).
The data from the Swedish National Diabetes Register and National Patient Register were taken to identify all patients with type 1 and 2 diabetes aged 18 to 34 years 1996 to 2019. Data on primary outcomes (acute myocardial infarction (AMI) and heart failure (HF)) was collected between 1998 and 2019.
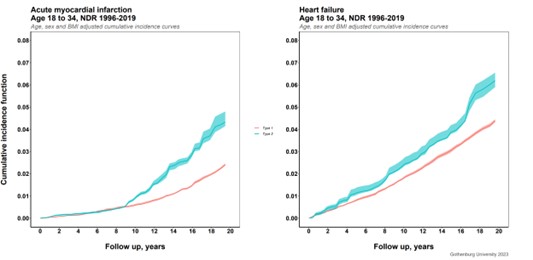
In total, 43,897 patients with diabetes, 32,208 patients (73.4% with type 1 diabetes and 11,689 (26.6%) with type 2 diabetes were included. Mean age in patients with type 1 and 2 diabetes was 23.1 (standard deviation (SD) 5.5) and 29.1 (4.4) years, respectively, with mean duration of diabetes in type 1 diabetes 8.6 (SD 7.2) and in type 2 1.7 (3.0 years). Patients with type 2, compared to type 1 diabetes had a substantially higher mean body mass index (BMI) of 34.6 (SD 9.1) and 24.3 (SD 6.2) kg/m2, respectively, and a more adverse risk factor profile with respect to lipids, blood pressure, and microalbuminuria, but lower mean HbA1c; 59.3 (SD 21.6) mmol/mol compared to 65.6 (SD 18.9) mmol/mol. During a mean follow-up of 12.2 (7.0) and 7.9 (5.6) years, for type 1 and type 2, respectively, 332 (1.0%) and 243 (2.1%) patients with type 1 and type 2, respectively, developed AMI and 142 (0.44%) and 87 (0.74%) heart failure. Cumulative incidence adjusted for age and BMI is shown in the Figure above.
Of the two types of diabetes, type 2, as expected, had the worst cardiovascular risk factor profile and more micro/macroalbuminuria despite shorter duration. In absolute terms type 2 also had higher risk of AMI and HF even after adjustment for age and BMI.
Association of Clinical Characteristics with Sudden Cardiac Arrest in People with Type 2 Diabetes with and without CVD: A Longitudinal Case-Control Study on Primary Care Data
Harms P.P.
Sudden cardiac arrest (SCA) is a substantial public health problem and the causative event of up to 50% of cardiac deaths, accounting for 20% of mortality in. high-income countries. People with type 2 diabetes have a twofold increased risk of SCA. However, predictors of SCA risk are not fully understood, specifically for those without a CVD history.
Harms P.P, presented a session at the European Association for the Study of Diabetes (EASD) Annual Meeting held in Hamburg, Germany on 5th October 2023, that assessed the (differences in) longitudinal associations of clinical characteristics recorded in primary care with SCA in people with type 2 diabetes with and without a CVD history.
A case-control study with SCA cases with type 2 diabetes from the AmsteRdam REsuscitation STtudies (ARREST) registry of out-of-hospital resuscitation attempts by emergency medical services in the Dutch region of Noord-Holland (2005-2019). We included cases with presumed cardiac cause registered at General Practice (GP) practices from the PHARMO Data Network and the academic network of general practice at Amsterdam UMC (ANHA). Cases were matched (age, sex, T2D, GP practice) with up to five non-SCA controls. From the GP files, we collected relevant clinical measurements, medication use, and medical history from before the SCA date of the case-control pairs. These measurements were grouped by year until 5 years prior the case’s SCA date, and then categorized including a ‘unknown’ category for measurements that were not recorded that year. We analysed the associations of clinical characteristics with SCA in the total sample and in subgroups with and without CVD using univariable and multivariable time-dependent Cox-regression (Hazard Ratios, 95% confidence intervals).
815 cases and 3,696 controls were included. In multivariable models, only insulin use (2.01 (1.56-2.60)) was associated with SCA in both people with and without CVD. In people with CVD (409 cases/1,392 controls), moderate (1.84 (1.19-2.84)), severe (1.96 (1.05-3.66)) and unknown (1.80 (1.21-2.68)) albuminuria, and heart failure (2.22 (1.78-2.76)) were associated with SCA. In people without CVD (406 cases/2,304 controls), current (1.68 (1.28-2.20)) and unknown (1.61 (1.30-2.00)) smoking behaviour, high LDL cholesterol (>2.6 mmol/l: 1.54 (1.00- 2.37)), and QTc prolonging anti-psychotic (2.52 (1.68- 3.77)), prokinetic (1.94 (1.23- 3.05), and anti-biotic medication use (1.41 (1.02- 1.97) were associated with SCA.
In people with type 2 diabetes with CVD, albuminuria and heart failure are signs of increased SCA risk, while in people without a CVD history current and unknown smoking behaviour, high LDL cholesterol, and QTc prolonging medication use are indicators of SCA risk.
Prescribing Trends of Anti-Diabetes Medications Near End of Life Among Older Adults with Type 2 Diabetes: A Nationwide Cohort Study
Kutz A
Although deprescribing anti-diabetes medications towards end of life has been suggested to be safe data on the extent, patterns and secular changes in discontinuation of these agents near end of life is still scarce.
Kutz A, presented a session at the European Association for the Study of Diabetes (EASD) Annual Meeting held in Hamburg, Germany on 5th October 2023, that assessed prescribing trends of anti-diabetes medications in the last year of life among older adults with type 2 diabetes and explored whether frailty is associated with differential prescribing patterns.
Using nationwide claims data from Medicare fee-for-service beneficiaries, we conducted a cohort study including older adults (≥67 years) with type 2 diabetes who died between 2015 and 2019. We plotted 6-monthly trends in prevalent and incident users of anti-diabetes medications overall and stratified by level of frailty. We also assessed differences in prescribing patterns within the last year of death (9 to 12 months vs 0 to 4 months before death).
Results: Among 975,407 Medicare beneficiaries with type 2 diabetes (mean [SD] age, 80.9 [8.2] years; 54.3% female; 34.9% frail), filled prescriptions for any anti-diabetes medication within 1 year of death increased from 71.4% in 2015 to 72.9% in 2019 (p<0.01). The most pronounced increase in use was observed for metformin (40.7% in 2015 to 46.5% in 2019, p<0.01), whereas the use of sulfonylureas decreased over time (37.0% to 31.8%, p<0.01). The proportion of people on any anti-diabetes medication decreased throughout the last year of life from 66.1% in the 9-12 months before death to 60.8% (p<0.01) in the 0-4 months before death. This decline was mainly driven by a decrease in use of non-insulin medications, whereas short-acting insulins were more likely to be prescribed towards the end of life (from 18.5% to 20.0%, p<0.01). Prescribing trends among incident users of anti-diabetes medications were similar, with short-acting (4.1% to 7.4%, p<0.01) and long-acting insulin (6.0% to 8.2%, p<0.01) more frequently initiated closer to end of life. Trends by level of frailty were similar, with a larger proportion of more frail individuals using short- and long-acting insulin near end of life. Newer medications with proven cardiovascular benefit were the least frequently prescribed agents at end of life, though their use became more frequent in recent years.
In this cohort study, the proportion of older adults with type 2 diabetes who used an anti-diabetes medication within 1 year of death increased over time. However, there was evidence of an increase in medication discontinuation towards the end of life, in accordance with practice guidelines.
Age Discrepencies in the Use of Glucose-Lowering Medications: A Nationwide Cohort Study
Johansson K
Various glucose-lowering medications are used to lower glycated haemoglobin (HbA1c) in patients with type 2 diabetes. Of the available medications, only glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose co-transporter-2 inhibitors (SGLT-2is) have documented preventive effects on cardiovascular disease events within a few years of treatment. For older patients, guidelines recommend a less strict HbA1c-target and discourage treatment with sulphonylureas due to their inherent risk of hypoglycaemia.
Johansson K, who presented a session at the European Association for the Study of Diabetes (EASD) Annual Meeting held in Hamburg, Germany on 5th October 2023, hypothesized that these guidelines are yet to be fully implemented and that older patients receive fewer and other glucose-lowering medications than younger patients.
The usage of glucose-lowering medication for all patients with type 2 diabetes in Denmark from 2018 to 2020 and related this to age and Hba1c by using regression models adjusting for: sex, renal function, comorbidities, level of education, gross household income and country of birth. A patient was considered a medication user if they redeemed a prescription of that medication class (fourth level ATC code) within three months following their Hba1c measurement were discussed.
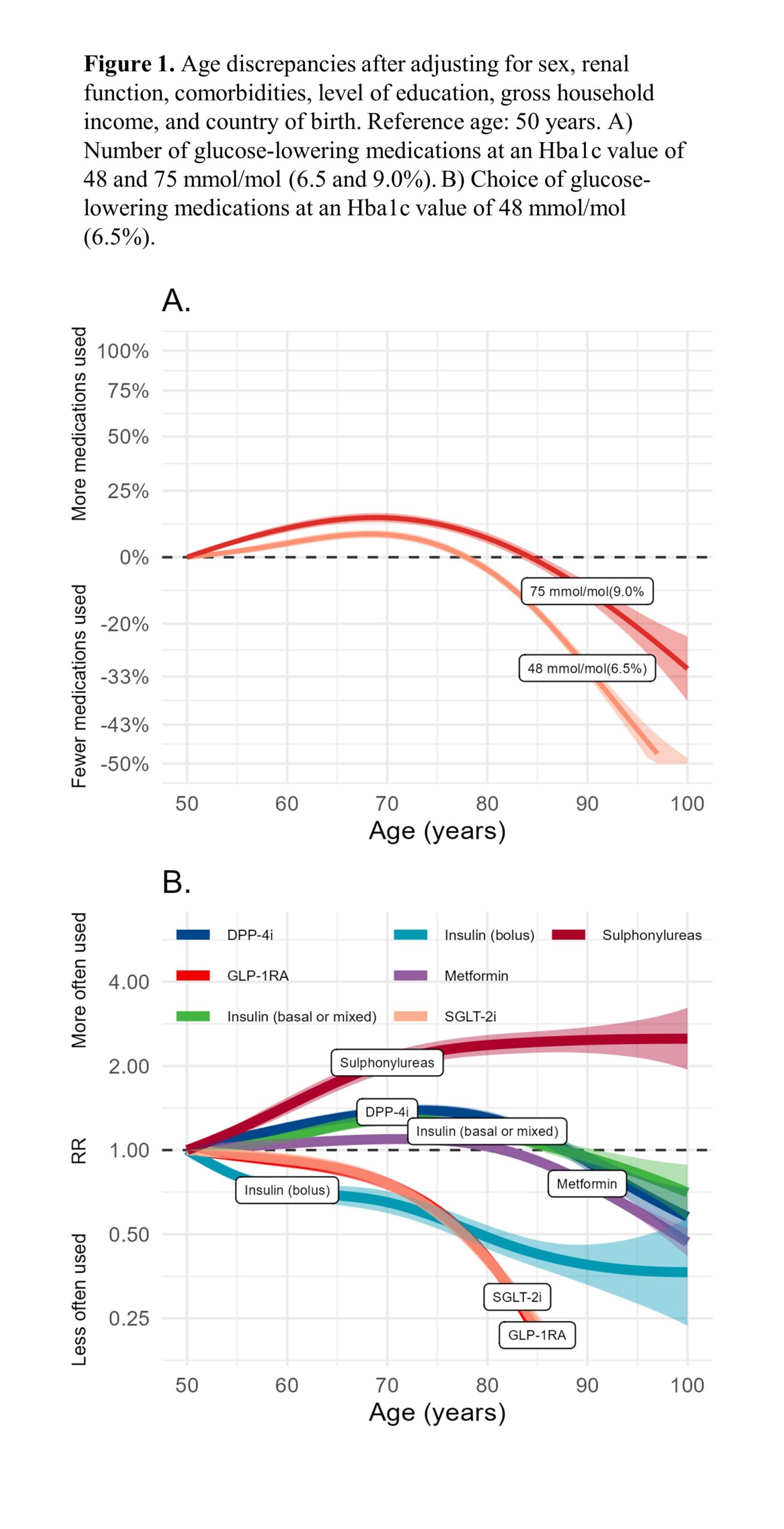
290,890 patients with type 2 diabetes in the study period were identified. The number of medications used peaked at the age of 70, whereafter it decreased (Figure 1A). For example, when comparing 80- and 90-year-old patients with 50-years-old patients at an Hba1c value of 48 mmol/mol (6.5%), 80-year-old patients used 5% (95% CI 3-6%) fewer glucose-lowering medications and 90-year-old patients 31% (95% CI 30-33%) fewer glucose-lowering medications. Older patients were generally less likely to be treated with GLP-1RAs and SGLT-2is (Figure 1B). In contrast, they were more likely to be treated with insulin, dipeptidyl peptidase-4 inhibitors, and sulphonylureas. These discrepancies were attenuated with an increasing Hba1c. For example, compared with a 50-year-old patient, an 80-year-old patient with an Hba1c-value of 48 mmol/mol (6.5%) was 59% less likely to receive either a GLP-1RA or a SGLT-2i (RR 0.41, 95% CI 0.38-0.44), but 137% more likely to receive sulphonylureas (RR 2.37, 95% CI 2.19-2.58).
In Denmark, older patients were treated with fewer glucose-lowering medications than younger patients at the same Hba1c-level. Older patients were also more likely to receive medications with a higher risk of hypoglycaemia, such as sulphonylureas and insulin, and less likely to use GLP-1RA and SGLT-2i. Our findings suggest a potential for treatment improvement and stress the importance of frequently re-evaluating glucose-lowering treatment in all patients, independent of age.
Effects of Type 2 Diabetes and Obesity on Cardiopulmonary Performance
Nesti L
Measured through oxygen uptake at peak exercise (VO2peak), effort intolerance is highly prevalent in patients with type 2 diabetes (T2D), wherein it predicts incident heart failure.
Nesti L, debated how to quantify effort intolerance at the European Association for the Study of Diabetes (EASD) Annual Meeting held in Hamburg, Germany on 5th October 2023.
Patients at high cardiovascular risk, with or without T2D, underwent pulmonary spirometry and a thorough cardiovascular characterization, including maximal combined echocardiography-cardiopulmonary exercise test (eCPET) to exclude pulmonary and/or cardiovascular disease. Overt microvascular complications were excluded as well. To isolate the effects of T2D and to identify the underpinning mechanisms, multivariable models were built accounting for the major pathophysiological determinants of VO2peak normalized for lean body weight (LBW), since fat mass has a neutral impact on oxygen uptake.
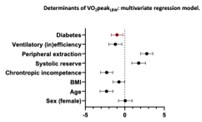
Results: A total of 109 patients with T2D and 97 non-diabetic controls (non-DM) were included in the analysis. The two groups had similar baseline characteristics except for higher body mass index (BMI) among T2D, with similar LBW. During exercise, T2D patients achieved lower VO2peak than non-diabetic subjects (T2D 26.1±5.4 vs non-DM 29.5±9.6 mL/min/kgLBW); subclinical cardiopulmonary impairments were observed, namely chronotropic incompetence, subclinical systolic dysfunction, and more marked cardiac remodeling. The main determinants of VO2peak were tested alone and in combination to identify the one(s) undermining the independent effect of T2D. Presence of T2D was an independent negative determinant of VO2peak in all models, maintaining statistical significance and a strong coefficient of determination (Figure 1). Overall, BMI reduced exercise capacity by 0.2 mL/min/kgLBW per unit, an effect that is largely explained by a combination of chronotropic incompetence, reduced peripheral oxygen extraction, impaired systolic reserve, and ventilatory (in)efficiency. On the contrary, T2D independently reduces VO2peak by 1 mL/min/kgLBW and this effect is only marginally explained by any or all the major determinants of cardiopulmonary fitness, which are additive to the effect of T2D per se.
T2D displays an independent negative effect on VO2peak even in the absence of cardiac or pulmonary disease. This effect is additive to all the other pathophysiological determinants of oxygen uptake, including obesity.

