Volterrani M, et al. Int J Cardiol. 2011 Sep 1;151(2):218-24.
An association is observed between heart failure (HF) patients with reduced exercise capacity. The positive impact of beta-blocker on prognosis is not coordinated by an effect on exercise capacity and quality of life. Thus, Volterrani M, et al., conducted a randomised open blinded endpoint study to analyse the impact of heart rate reduction with Carvedilol, Ivabradine, and their combination on exercise capacity in patients with HF receiving maximal dose of ACE inhibitor. Patients were randomly recruited to 3 groups after a run-in phase: 38 patients in Carvedilol group (up to 25 mg bid); 41 patients in Ivabradine (up to 7.5 mg bid) and 42 patients in Carvedilol/Ivabradine (up to 12.5/5 mg bid). The distance covered in the 6-min walking test and maximal oxygen consumption (MVO2) on the cardiopulmonary exercise test were included in the primary endpoint. Quality of life and change in NYHA class were included in the secondary endpoint. Out of 41, 36 patients receiving Ivabradine tolerated maximum dose as compared with those patients receiving Carvedilol (18/38) or combination therapy (32/42). Equal reduction was observed in heart rate among all three groups, but greater reduction was observed in the combination group. Ivabradine and combination group showed significant improvement in the peak VO2 (+3.8±2.0 mL/kg/min, p<0.01) and VAT (+2.3±1.7 mL/kg/min, p<0.03) at 3 months, whereas no change was observed in the Carvedilol group (−0.6±1.2 mL/kg/min), respectively.
Ivabradine shows significantly higher improvement in NYHA class in patients with Ivabradine and combination therapy as compared to those with Carvedilol. (Figure 1)

Figure 1: Number of patients with an improvement by at least one New York Heart Association (NYHA) class according to treatment allocation (Carvedilol, Ivabradine, or combination Carvedilol/Ivabradine). *p<0.001 Ivabradine versus Carvedilol; p<0.003 Carvedilol versus Carvedilol/Ivabradine
Ivabradine and combination group showed significant improvement in the 6-min walking test and the exercise time on MVO test as compared with baseline (p<0.01). (Figure 2)
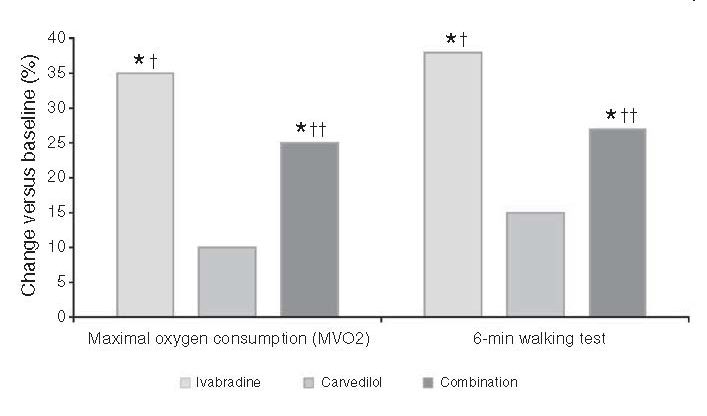
Figure 2: Effect of Carvedilol, Ivabradine, and their combination on percentage change in exercise capacity (peak oxygen consumption [MVO2] and result on 6-min walking test) over the 3 months of the study. *p<0.01 versus baseline; †p<0.01, ††p<0.02 versus Carvedilol
Better quality of life was observed in Ivabradine group patients or the combination group (p<0.01 versus baseline for Ivabradine and p<0.02 for combination), but no change was observed with Carvedilol.
This present study concludes that as compared to Carvedilol alone, Ivabradine or its combination with Carvedilol was found to be more effective in improving exercise capacity and quality of life in HF patients receiving recommended doses of ACE inhibitors. It was also observed that patients receiving Ivabradine therapy are likely to reach target therapeutic doses as compared with patients receiving Carvedilol alone.

