Pfeffer MA, et al. Circ Res. 2019 May 24;124(11):1598-1617.
In the past 20 years, the identification of the consequence of the problem of heart failure with preserved ejection fraction has prompted an outcome of clinical investigation and growing intensity of informative outcome trials. Pfeffer MA, et al., conducted a review article to addresses the historic development of this component of the heart failure (HF) syndrome which also includes the epidemiology, pathophysiology, and existing and planned therapeutic studies.
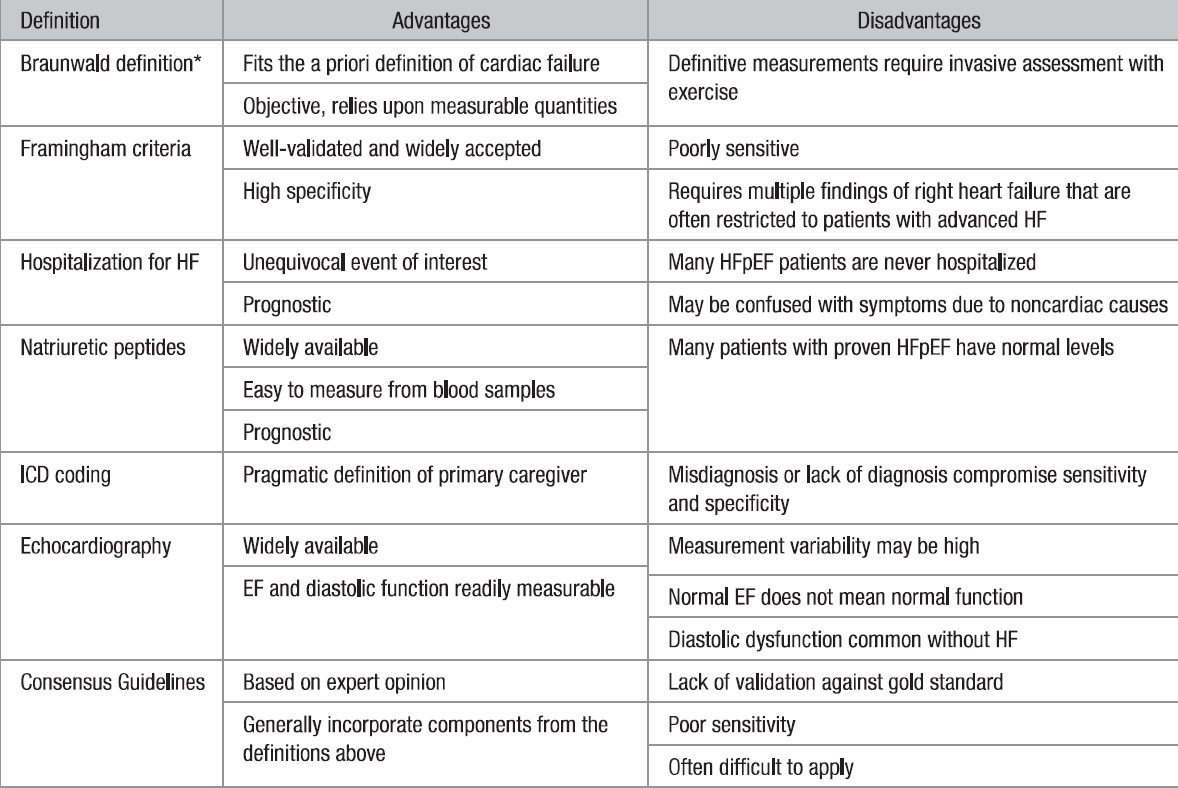
To clinically interpret the HF syndrome, multiple ways have been used based on an integration of the patient’s history, presentation, physical examination, and laboratory supportive findings to analyse if HF is present, each with its own advantages and disadvantages (Table 1).
Table 1. Controversies in the Definitions of HFpEF
Left Ventricular Ejection Fraction
To understand the activity of the LV in normal participants and in patients with different cardiovascular abnormalities, the fraction of the LV volume ejected per beat (LV ejection fraction [LVEF]) was measured. LVEF was exhibited to both preload and afterload dependent and as such, there were other invasive measurements that better reflected ventricular contractility. LVEF emerged as the leading term clinicians used to represent the LV function of their patients because of the convenience and ease of non-invasive assessment despite load-dependent shortcoming.
Diastolic HF
Initially termed diastolic HF, supporting hemodynamic studies indicates high filling pressures without notable increases in ventricular chamber size. Ventricular relaxation has been an active process with ischemia conversely impacting filling. As perception increased about the development of diastolic HF, the markedly concentrically hypertrophied LV with small to normal cavity volumes (increased mass to volume ratio) and maintained systolic function evolved in the expected trademark feature of diastolic HF.
Taxonomy Diastolic HF to HF with Preserved Ejection Fraction
The researchers labelled this component trial of those with EF >40% as CHARM-Preserved based on how these patients were being analysed for the trial. The term was to differentiate from the well-studied lower EF groups and not likely meant to involve normal LV structure or function. However this was not the first use of the term HF with preserved ejection fraction (HFpEF), the declaration of a major outcome trial using that terminology was correlated with an upsurge in its usage (Figure 1).
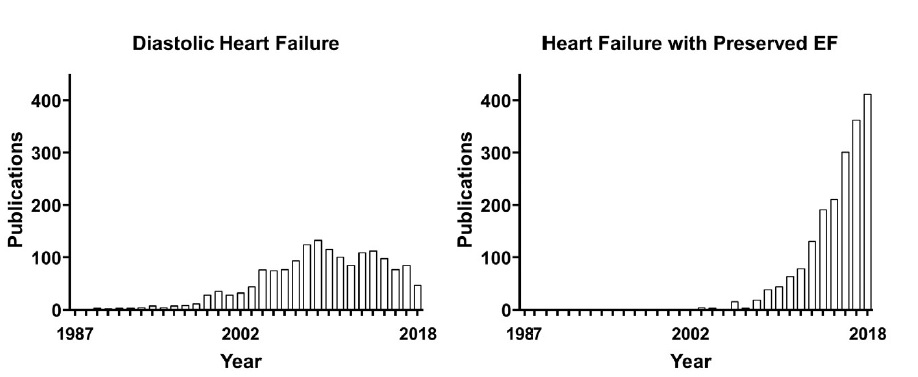
Figure 1. PubMed citations for heart failure with preserved ejection fraction (EF) from 1986 to 2018.
Demographics and Clinical Comorbidities in HFpEF
The scientific syndrome of HFpEF evolved from a complex interaction of several risk factors that results in organ dysfunction and ultimately causes clinical symptoms (Figure 2).
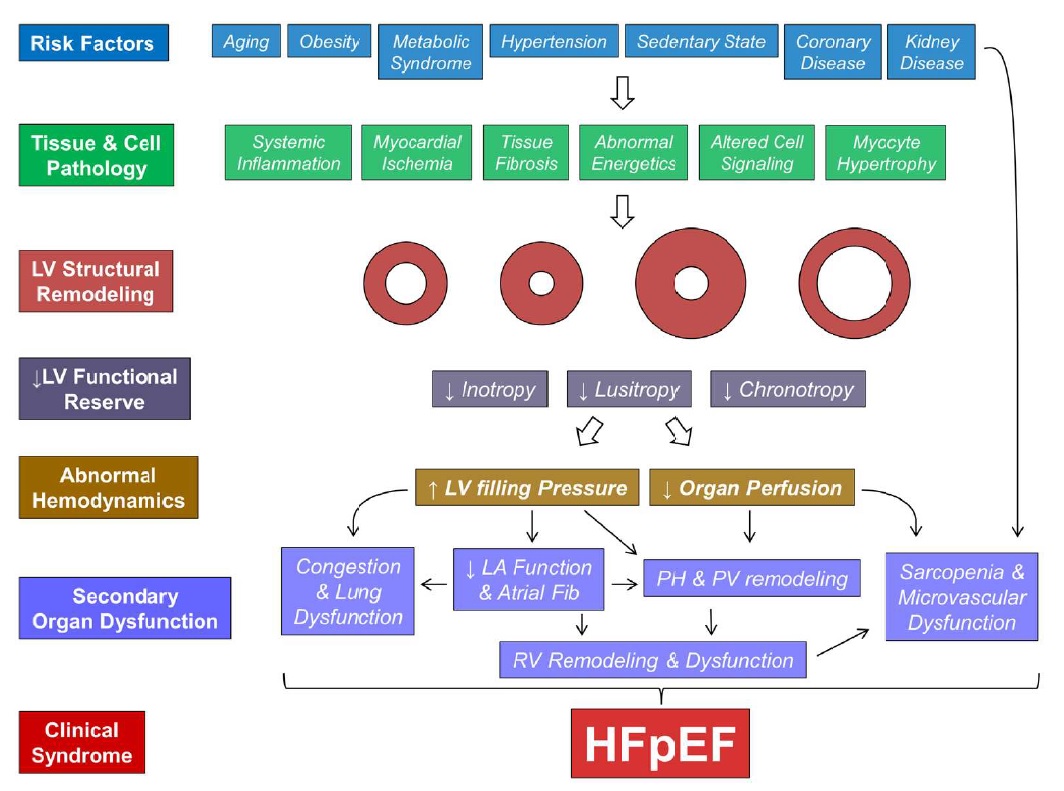
Figure 2. The Pathophysiologic Progression of heart failure with preserved ejection fraction (HFpEF).
LV Diastolic Dysfunction
In later stages of HFpEF, LVFPs are high at rest, but LVFP remain markedly elevated only through the stress of exercise in patients with earlier stages of disease. High LVFP during exertion in HFpEF are directly associated with heightened inspiratory drive, symptoms of dyspnea, alterations in gas exchange and pulmonary ventilation, and reductions in aerobic capacity (Figure 3).
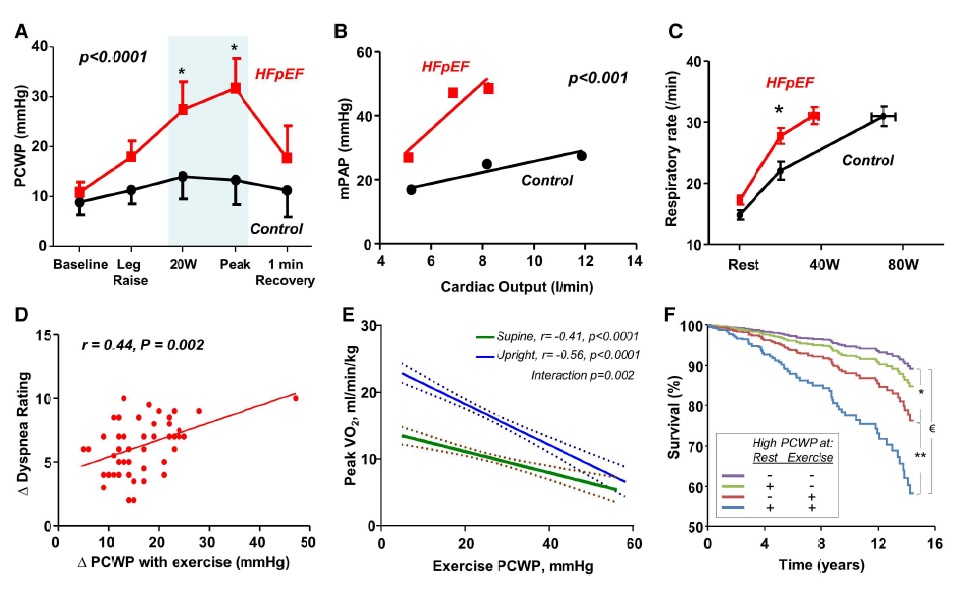
Figure 3. Relationship between exercise hemodynamics, symptoms, functional disability and outcomes in heart failure with preserved ejection fraction (HFpEF).
Thus, it was concluded from future trials that progressively, more specific phenotyping and even genotyping of sub-populations must lead to improvements in outcomes, and further decline of burden of HFpEF in their specifically targeted population as well as identify others within the broad term HFpEF for future studies.

