Nguyen VP. J Am Coll Cardiol. 2019 Dec 10;74(23):2908-2918.
Heart failure is the prime root of premature morbidity and mortality in adults with CHD (ACHD). The effectiveness of medical therapy for heart failure is not well established in CHD thus, many ACHD patients need contemplation for heart transplantation. Heart transplantation for ACHD patients indicates a high surgical risk because of complex anatomy, earlier cardiac surgery, the existence of collateral vessels, and correlated liver and renal disorder. Even though for ACHD patients had increased early post-transplant mortality, those who survived transplant have enormous long-term post-transplant effects. Nguyen VP et al., conducted a study to analyse the outcome of center CHD transplant volume and expertise on transplant effects in CHD patients. But, CHD patients exhibits anatomic and physiologic challenges that may not be familiar, even at high-volume transplant centers, except if these centers have experience and expertise in ACHD care and ACHD surgery. The effect on ACHD expertise and transplant volume on ACHD transplant outcomes has not been examined.
The study cohort consisted of 1,746 adult heart transplant candidates age ≥ 18 years with CHD listed for transplantation between January 1, 2000, and July 1, 2018 in the Scientific Registry of Transplant Recipients registry from the UNOS. The primary waitlist outcome was death or being delisted for being too sick. The primary post-transplant outcome was graft failure, specified by either death or retransplantation. A waitlist outcomes were analysed with a competing outcome of heart transplantation with fine-Gray competing risk regression analysis. The primary outcome of post-transplant was estimated with a Cox proportional hazards model.
From 1,746 patients, 1,006 (57.6%) patients were transfered at 124 transplant centers in the study period. Adult Congenital Heart Association accredited centers showed lower waitlist mortality risk after adjusting for age, sex, listing status, and inotrope need (HR: 0.730; p = 0.020). (Figure 1).
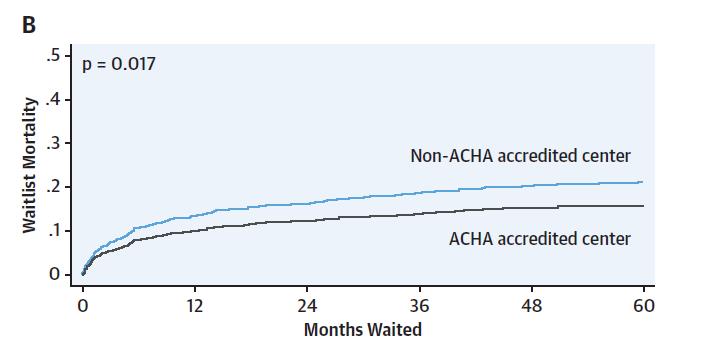
Figure 1: Cumulative Incidence of Waitlist Mortality for All Listed Congenital Heart Disease Patients Age ≥18 Years; ACHA-accredited versus not accredited of both adult and pediatric hospitals.
ACHD patients transfered at the highest volume CHD transplant center showed lower risk of graft failure /post-transplant 30-day mortality in each UNOS region (HR: 0.706; p = 0.014) and at 2 years (HR: 0.658; 95% CI: 0.443 to 0.978; p = 0.038) (Figure 2)
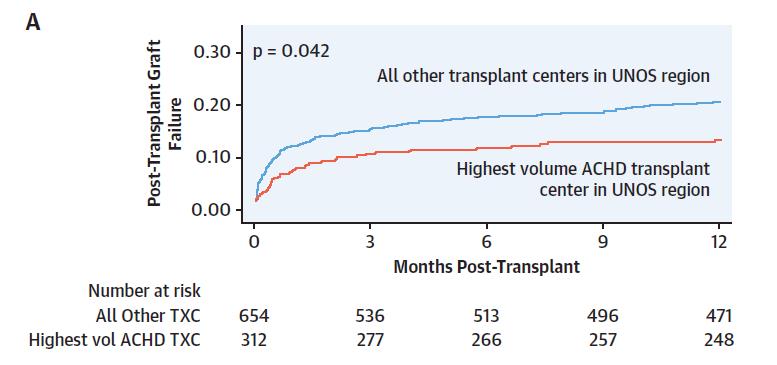
Figure 2: Post-Transplant Cumulative Hazard for Graft Failure for Transplanted Patients with Congenital Heart Disease; Highest CHD volume center in a UNOS region versus all other centers
Thus it was concluded that entitled expertise in CHD care is correlated with increased waitlist effects for CHD patients listed for transplantation. Post-transplant survival was enhanced at the highest volume regional center. A possible benefit of regionalization of CHD transplantation was recommended with these findings.
UNOS: United Network of Organ Sharing

