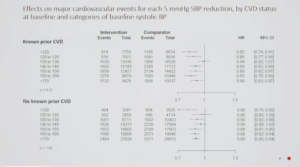
BPLTTC – Blood Pressure Lowering for Prevention of Cardiovascular Events across Different Levels of Blood Pressure
Findings from the BPLTTC trial was presented at ESC Congress 2020: A digital experience by the principal investigator Kazem Rahimi. The BPLTTC researchers conducted a meta-analysis of data from 348,854 participants from 48 clinical trials from around the world. Participants were divided into two groups: those with a prior diagnosis of cardiovascular disease and those without. Each group was then further divided into seven subgroups based on systolic blood pressure at study entry (less than 120, 120-129, 130-139, 140-149, 150-159, 160-169, and 170 and above mmHg). The average follow-up was four years.
Overall results showed a reduction in relative risk of major cardiovascular events by roughly 10% for each 5 mmHg reduction in systolic blood pressure. Risk for stroke, ischemic heart disease, heart failure, and death from cardiovascular disease were reduced by 13%, 7%, and 14%, and 5%, respectively. However, there was no evidence that proportional effects varied by baseline BP values, down to the lowest systolic BP category of <120 mmHg, in both primary and secondary prevention settings.
Conclusion: The decision to prescribe blood pressure medication should not be based simply on a prior diagnosis of cardiovascular disease or an individual’s current blood pressure. Rather, blood pressure medication should be viewed as an effective tool for reducing cardiovascular risk when an individual’s probability of having a heart attack or stroke is elevated.
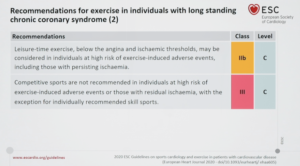
2020 – ESC Guidelines on Sports Cardiology and Exercise in Patients with CVD
The 2020 ESC Guidelines on Sports Cardiology and Exercise in Patients with CVD was presented for the first time exclusively at the ESC Congress 2020: The digital experience. The promotion of exercise is now at the forefront of all medical organisations to curb risk factors and hence these guidelines are welcome recommendations. These guidelines cater for individuals with risk factors for coronary artery disease and a diverse spectrum of cardiovascular diseases promoting safe exercise in the general population. One of the most important thing of course is to identify middle aged and older people who may have quiescent coronary artery disease that may trigger an exercise-related myocardial infarction. In this respect a pragmatic approach that utilizes the presence of symptoms and established risk factors as well as the score system to identify those that are high risk and very high risk is needed. If these individuals want to participate in exercise or competitive sport then they should have an exercise stress test or functional imaging before going into intensive exercise. When it comes to heart failure, the emphasis is on optimisation of medical therapy, risk stratification and assessment of functional capacity. In individuals with NYH functional class I and II can engage in moderate or occasionally high intensity exercise. When it comes to valve diseases, then all exercise is permissible. Conversely those with severe valvular heart disease should only engage in the current ESC recommendations of 150 to 300 minutes of moderate exercise. With emerging evidence of the past two decades the ESC guidelines suggest that people who are asymptomatic, have morphologically mild disease and a low risk profile may engage in all competitive sports except where syncope may cause trauma. It is even stricter in arrhythmogenic cardiomyopathy, those who are genotype positive and phenotype negative these individuals should only participate in mild or moderate exercises. Apart from severe valvular heart disease and arrhythmogenic cardiomyopathy individuals with poor left ventricular function and active myocarditis should not engage in high intensity exercise or high intensity competitive sports. As far as individuals with anticoagulation or implantable cardioverted defibrillators are concerned, collision sport or sport that involves bodily trauma is not advised, as it could result in a catastrophic event or even damage to the defibrillator. Most importantly and imperatively, shared decision making is encouraged, i.e. all the pros and cons of exercise and the potential risks of exercise in any one cardiovascular condition should be discussed with the individual before promoting exercise and these discussions should be documented.
Diabetes Drugs Targeting Heart Failure- State-of-the-art lecture – Diabetes drugs targeting heart failure
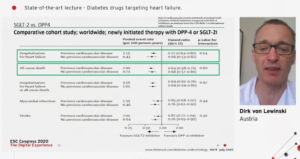
Lewinkski, presented a session on diabetes drugs targeting heart failure at the ESC Congress 2020: The digital experience. There is high prevalence of heart failure in DM patients 5-25%. However, the prevalence of DM in heart failure patients is much more i.e. 20-50%. After problems with the glitazones, every drug of diabetes is made to study the cardiovascular outcomes to show that atleast MACE is not worsened. Over the years several trials like SUSTAIN, LEADER, HARMONY and EMPA-REG have shown positive cardiovascualr outcomes in diabetes patients. ESC guidelines recommend the use of SGLT-2 inhibitors or GLP-1 anatgonist as the first line drug in drug naïve and in patients on metformin. A huge comparative cohort trial, worlwide newly initiated with DPP-4 or SGLT_2i. All major outcomes like hospitalisation for heart failure, all-cause death, stroke, hospitlisation for heart failure or all-cause deaths were significantly reduced in the SGLT-2i group.
The PIONEER trial examining semiglutide in 3283 patients demonstrated a decline in death from cardiovascular causes. Likewise the LEADER trial which investigated liraglutide in almost 10000 patients also showed favourable results depicted as decline in death from cardiovascular causes. The recent LIVE trial also demonstrated a decrease in proBNP in heart failure patients with diabetes. A recent paper comapring the effects of SGLT-2i with GLP-1 analogs proved that SGLT2i demonstrate a favourable effect on CV outcomes ranging from 3P-MACE to CV death. DAPA-HF trial also verified the efficacy of dapagliflozin in reducing CV death, HF hospitalisation and urgent HF visit. 453 trials assessing 21 antidiabetic interventions, 9 drug classess in 320474 patients divided the patients into low and increased cardiovascular risk where SGLT-2 inhibitors showed greater effects than DPP-4 inhibitors.
Conclusion: Several anti-diabetic drugs positively impact heart failure. SGLT-2 inhibitors provide the greatest benefit.
Early coronary angiography in acute ischemic heart failure is associated with improved survival and lower rates of heart failure hospitalization
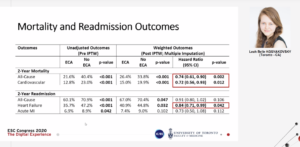
Kosyakovsy, presented a session at the ESC Congress 2020: The digital experience to identify the clinical predictors of performing early coronary angiography in acute ischemic HF and determine the association of angiography with all-cause mortality, cardiovascular death, and HF readmissions. Acute HF patients who presented to any of 70 emergency departments in Ontario, Canada were identified and determined whether they underwent early coronary angiography (defined as angiography performed within 14 days of hospital presentation) using procedural data contained in the Canadian Institute for Health Information (CIHI) database (April 2010 to March 2013). Predictors of 14-day coronary angiography were determined using multivariable logistic regression. The compared mortality and readmissions up to two-year follow-up. Inverse probability of treatment weighting (IPTW) using the propensity score was used to adjust for differences in baseline characteristics between the two cohorts. It was observed that out of 6,172 initially screened patients, 4,118 met criteria for acute ischemic HF. After exclusions, 2,994 were included in the study. Of these, 1,567 (52.3%) underwent early angiography and 1,427 (47.7%) did not (median age 75 [IQR 65-83] years and 40.9% women). Clinical factors associated with greater odds of early angiography included previous MI, anginal symptoms at presentation, New York Heart Association (NYHA) III-IV symptoms, and family history of coronary artery disease. After IPTW, early angiography was associated with lower all-cause mortality (HR 0.74, 95% CI; 0.61-0.90, p=0.002) and cardiovascular death (HR 0.72, 95% CI; 0.56-0.93, p=0.012) at two years. HF readmissions were also lower with early angiography (HR 0.84, 95% CI; 0.71-0.99, p=0.042).
Conclusion: Early coronary angiography in acute ischemic heart failure was associated with lower all-cause mortality, cardiovascular death, and HF readmissions.
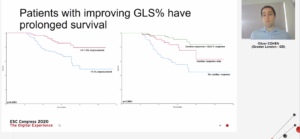
Global longitudinal strain predicts survival and response in patients with systemic AL amyloidosis, Analysis of 915 patients from the ALchemy prospective trial
Cohen, presented a session at the ESC Congress 2020: The digital experience discussing the analysis of 915 patients from the ALchemy prospective trial. This was a prospective report of a large cohort of patients assessing the utility of changes in longitudinal function by 2D strain (GLS%), impairment – a hallmark of amyloidosis. The objective of the analysis was to evaluate the prognostic role of GLS% and other echocardiographic parameters in systemic AL amyloidosis. The resutls observed were: 653/915 (71.4%) patients had cardiac involvement. Mayo stage 1, 2, 3a and 3b in 144 (15.7%), 302 (33.0%) 344 (37.6%) and 125 (13.7%) respectively. The median NT-proBNP was 2228 ng/L and TNT was 0.54 ng/ml. The GLS% significantly worsened with increasing Mayo stage (p<0.0001 between GLS% for each Mayo stage). Poorer baseline GLS% associated with significantly worse OS and stratified patients into three groups: GLS% <-12.8%: OS 69.1 months; GLS% -12.8%- -9%: OS 54.5 months; GLS% >-9%: OS 45.3 months (p<0.0001). Baseline GLS% >-17% was independent of Mayo stage in predicting survival [Mayo II: Hazard ratio (HR) 2.10 (95% CI: 1.12-3.92) p=0.02, Mayo III: HR 3.94 (95% CI 2.13-7.32) p<0.0001, Mayo IV: HR 7.49 (95% CI: 3.94-14.21) p<0.0001, GLS <17%: HR 2.14 (95% CI 1.59-2.88) p<0.0001]. At 12 months, only patients in a haematological complete response (CR) had significant improvement in overall GLS% (p=0.02) as well as baso-lateral (p=0.0004) and baso-septal (p=0.0001) GLS% and mitral annular plane systolic excursion (MAPSE) (p=0.002). The OS was significantly better in patients who achieved a minimum absolute improvement in GLS% of 1.5% improvement (not reached in those with improved GLS% vs. 72 mo in those without) (p=0.034)).
Conclusion: This study proved that baseline GLS% is an independent predictor of survival in AL amyloidosis. GLS% is the first functional marker that is independent of the Mayo staging in forecasting outcomes and must be incorporated in prognostic staging for patients with AL amyloidosis. GLS% shows improvement in patients who achieve a complete haematologic response to treatment and improvement in GLS% of 1.5% is associated with improved outcomes.
Myocardial iron depletion exacerbates end-stage heart failure by promoting adverse remodeling and worsening mitochondrial function
Zhang, presented a session at the ESC Congress 2020: The digital experience which aimed to integrate clinical information and experimental data from human explanted heart tissues: 1) to establish the defining criterion of myocardial iron depletion (MID) in advanced HF population; 2) to recapitulate the pathophysiological role MID plays in the progression of HF; and 3) to identify novel HF molecular signatures or potential cures to correct MID status underestimated in the failing hearts.
Collection of adult failing hearts (n=143), including dilated (n=76) and ischemic (n=67) cardiomyopathies, and non-failing control hearts (NFC, N=46) were done as per Human Explanted Heart Program. Iron levels were measured directly from both ventricles, which were re-evaluated by cardiac magnetic resonance imaging (CMR) mapping sequences (e.g. T1, T2*, etc.). Mitochondrial metabolic, reactive oxygen species (ROS) and ROS-scavenging profiles were assessed spectrophotometrically. confocal and electron microscopies were used to capture tissue remodeling and ultrastructure characteristics respectively. In the meantime, the patients’ clinical profiles were integrated into the analysis of molecular regulatory mechanism. Myocardial iron content in LV was significantly lower in HF versus NFC [121.4 (88.1-150.3) vs. 137.4 (109.2-165.9) µg/g dry weight, p<0.05], while both RVs showed no difference. With a cutoff of 86.1 µg/g iron level in LV, it screened ~23% HF patients with MID (HF-MID). Compared with non-MID HF patients, depleted iron store weakly correlated with systemic hemoglobin concentration (r=-0.27, p=0.13) but highly with T2* and magnetic susceptibility proving CMR as an exceptional surrogate for non-invasive diagnosis. And it was noted that MID independently predicted ominous endpoints as NYHA grade increased and LV dysfunctions worsened (all p<0.05). Mechanistically, two iron-regulatory proteins (IRP-1/2) and following iron trafficking pathways were inactivated possibly determine the restricted iron availability to advanced failing hearts.
Conclusion: HF progression is worsened by MID, fundamentally mediated by mitochondrial dysfunction and collapsed oxidative protection in LV, independently predicting an inferior prognosis. CMR establishes the clinical potential to monitor MID.

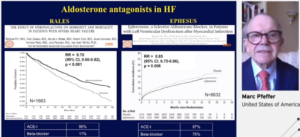
Old drugs in the modern era: ACEI/ARB, MRAs+digoxin
Marc Pfeffer presented a session on Old drugs in the modern era: ACEI/ARB, MRAs+digoxin at the ESC Congress 2020: The digital experience. In the field of heart failure, a very rich heritage exists where clinical trials with the outcome matter. Treatment with heart failure made a difference and difference was mortality. In CONSENSUS study, a new drug Enalapril, an ACEi showed survival in very sick patients and placebo deomstrated 50% mortality at the end of 6 months. In comparison of Enalapril with hydralazine-isosorbide dinitrate, the ACEi is superior in outcome of all-cause mortality (death). In SOLVD study, patients with LVEF, with or without symptomatic HF the mortality is much different in symptomatic than asymptomatic. In treatment arm, mortality shows a difference between Enalapril and placebo. In prevention arm, result was nonsignificant. But, In SOLVD trial of 1992, the outcome death or hospitalization for CHF shows upto 30% reduction. In DIGITALIS study, the outcome i.e. death or hospitalization due to worsening of heart failure was lower in the digoxin group. Beta-blockers decreases mortality in systolic HF in various trials such as by 34% in MERIT-HF and CIBIS II, by 35% in COPERNICUS trial. In RALES study, Spironolactone shows better survival as compared to placebo and in EPHESUS study, Eplerenone shows lower cumulative incidence of all-cause mortality in Eplerenone than placebo.
In conclusion, now there is a very firm foundation for new therapies and principles in place. The outcome of patients, drugs or prognosis needs to be discussed, if they do so, it’s truly an advance. New drugs have to raise the bar even higher.
Angiotensin receptor blockers and mineralocorticoid receptor antagonists’ therapy reaches better central haemodynamic parameters and avoid the episodes of atrial fibrillation
The aim of antihypertensive treatment is to inhibit complications. The harmful impacts of aldosterone are countless: influenced cardiac/renal fibrosis, sodium and water retention, inflammation, oxidative stress, arterial/myocardium stiffness, remodelling, heart failure and new-onset atrial fibrillation (AF). Thiazide diuretics can induce the neurohormonal system, impair glucose metabolism, enhance new-onset diabetes, and are definitively arrhythmogenic. Protective impact of Angiotensin Receptor Blockers (ARB) on vital cardiovascular occurrences might be partly independent of the degree of decrease in blood pressure. Mineralocorticoid Receptor Antagonists (MRA) treatment decrease arterial stiffness, plasma volume, collagen/elastin ratio and vascular/myocardial fibrosis. Paterno Marchioli CA, presented an ePoster at ESC Congress 2020: The digital experience which examined the levels reached in central haemodynamic parameters (CHP) and the existence of episodes of AF in ARB+hydrochlorothiazide (HCTZ) versus ARB+MRA treatment in hypertensive patients with normal kidney function.
108 hypertensive patient’s data were enrolled in this cross-sectional retrospective study, 62 females (ARBs+MRA/ARB+HCTZ average age 67/71), 46 males (average age ARB+MRA/ARB+HCTZ 67/71), both p=ns). The average doses of Hct between female/male were 16/19 mg and the ARB+Hctz treatment period was 37/47 months, although the ARB+MRA treatment were for 36/49 months. In all patients, 24-hours Holter monitoring was used. The group ARB+MRA before treatment showed a history of AF episodes. The SphygmoCor System PVX (AtCor-Medical, Australia) registered the CHP (Central Aortic Pressure, End-Systolic Pressure, Mean Arterial Pressure, Pulse Pressure, Augmentation Pressure, Augmentation Index), as per the system’s standard procedures. Also estimated the difference among the normal levels, and the observed values of Augmentation Index (Diff-AIx) according age. The results of CHP, Diff-AIx, systolic and diastolic blood pressure in correlation of ARB+MRA treatment exhibited the lowest values with a greatly statistically substantial difference as compared to ARB+Hct, both genders. In the group ARB+Hct therapy, the episodes of AF in 24-hours Holter monitoring in female/male were 55%/71%; rather, in the ARB+MRA treated they were not found.
Conclusion: These findings recommend that the dual block with ARB+MRA therapy showed better CHP. Reducing the stress to arterial-ventricular coupling, could be helpful to inhibit, the harmful impacts of angiotensin-aldosterone system such as the development of heart failure and atrial fibrillation.
Dapagliflozin in a real-world population with chronic heart failure: how many would be eligible?
The sodium-glucose cotransporter inhibitor (SGLT2i) Dapagliflozin has recently been shown to reduce the risk of worsening heart failure or death from cardiovascular causes in patients with heart failure (HF) and reduced left ventricle ejection fraction (LVEF), in the DAPA-HF trial. Results of SGLT2i in HF with preserved LVEF are anticipated. Maltes S, presented an ePoster at ESC Congress 2020: The digital experience which analysed how many patients would be entitled for Dapagliflozin as per the DAPA-HF criteria in a real-world setting. In a single-center retrospective study, consecutive patients were enrolled and followed in an HF Clinic from 2013 to 2019. The key DAPA-HF inclusion criteria [i.e., Left Ventricular Ejection Fraction (LVEF) <40% and NT-proBNP >600pg/mL (or >900pg/ml if AF)] and exclusion criteria [estimated glomerular filtration rate (eGFR) <30ml/kg/1.73m2, systolic blood pressure (SBP) <95mmHg] were contemplated. Altogether, 479 patients (mean age 75.7 ± 12.8 years; 50.4% male; 78.8% with hypertension; 45.0% with an eGFR <60ml/min/1.73m2; 36.5% with type 2 diabetes mellitus; 33.5% ischaemic HF) were examined. Of these, 155 (33.2%) patients showed LVEF <40%. Patients showed mean SBP of 131 ± 28 mmHg, a median eGFR of 48 (IQR 33-65) ml/min/m2 and a NT-proBNP of 2183 (IQR 1010-5310) pg/mL. Overall, 88 patients (18.3%) would be entitled for Dapagliflozin according to the DAPA-HF trial key criteria. The remainder would be excluded because of a LVEF>40% (67.5%), eGFR <30 ml/min/1.73m2 (19.4%), NT-proBNP <600 pg/mL (or <900 pg/mL if AF) (16.7%) and/or SBP <90mmHg (2.1%) (figure 1). If the analysis is limited to those with a LVEF <40%, 56.7% would be entitle for Dapagliflozin. The remainder would be excluded because of a eGFR <30ml/kg/1.73m2 (20%), NT-proBNP <600 pg/mL (or <900 pg/mL if AF) (16.1%) and/or SBP <90mmHg (8.4%) (Figure).
Conclusion: Roughly one in every five patients in our real-world HF cohort would be eligible to start dapagliflozin according to the key criteria of the DAPA-HF trial. The main reason for non-eligibility was a LVEF >40%. These findings highlight the urgent need for disease-modifying drugs in mid-range and preserved LVEF. The results of ongoing SGLT-2i trials in these LVEF subgroups are eagerly awaited.
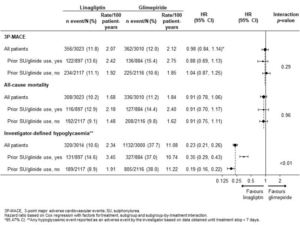
Effects of linagliptin vs glimepiride stratified by prior insulin secretagogue use in the cardiovascular outcome study of linagliptin versus glimepiride in type 2 diabetes (CAROLINA) trial
The cardiovascular outcome study of linagliptin versus glimepiride in type 2 diabetes (CAROLINA) was outlined to compare the impacts on cardiovascular (CV) occurrences, and other outcomes, of linagliptin with glimepiride in patients with relatively early type 2 diabetes with increased CV risk. McGuire DK, presented ePoster of a post hoc analyses of the CAROLINA randomized controlled trial at ESC Congress 2020: A Digital experience which investigated outcomes in subgroups differentiated by prior sulfonylurea (SU) or glinide use.
Participants with comparably early type 2 diabetes, high CV risk and HbA1c 6.5–8.5% were randomized to Linagliptin 5 mg or Glimepiride 1–4 mg once daily with standard of care. 29.5% of patients showed prior SU/glinide use. At trial entry, SU/glinides were discontinued. Outcomes incoporated time to first CV death/MI/stroke (3P-MACE), time to all-cause mortality, HbA1c change from baseline and time to first hypoglycaemia occurrence. 6033 participants acquired ≥1 study drug dose (mean [SD] age 64.0 [9.5] yrs, HbA1c 7.2 [0.6] %, median diabetes duration 6.3 yrs, 42% with CV disease); 897 linagliptin and 884 glimepiride participants showed prior SU/glinide use. Results for 3P-MACE and all-cause mortality were regular over subgroups with/without prior SU/glinide use (interaction p>0.05; Figure). After some initial differences, no meaningful difference was shown in HbA1c among Linagliptin vs Glimepiride across SU/glinide subgroups and overall. Linagliptin showed lower hypoglycaemia rates than Glimepiride overall and across SU/glinide subgroups, with some heterogeneity for earlier SU/glinide use (interaction p<0.01; Figure).
Conclusion: There was no difference on 3P-MACE and all-cause mortality in Linagliptin versus Glimepiride, with regular consequences over subgroups irrespective of earlier use of SU/glinide. Hypoglycaemia rates were constantly lower with Linagliptin vs Glimepiride, despite of earlier use of SU/glinide.
The effect of dapagliflozin across the spectrum of baseline risk: a post-hoc analysis of DAPA-HF
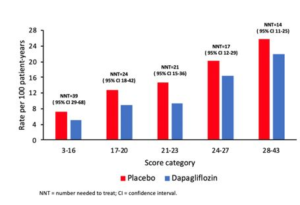
The sodium-glucose cotransporter 2 (SGLT-2) inhibitor, Dapagliflozin showed reduction in the risk of cardiovascular death or worsening heart failure in patients with heart failure with reduced ejection fraction (HFrEF) as compared to placebo in DAPA-HF. The most of patients exhibited mild functional limitation in DAPA-HF, but there is substantial heterogeneity in prognosis between these patients. Thus, Docherty K, presented an ePoster at ESC Congress 2020: A digital experience which analysed the impact of Dapagliflozin across the spectrum of baseline risk as compared with placebo in DAPA-HF.
The primary composite outcome of DAPA-HF was time-to-first cardiovascular death or worsening heart failure event (hospitalization for heart failure or outpatient visit requiring intravenous therapy). It was analysed whether the impact of Dapagliflozin was modulated by baseline risk, as measured by the MAGGIC (Meta-Analysis Global Group in Chronic Heart Failure) risk score based upon 13 predictive variables giving a potential maximum score of 57. Over a median follow-up of 18.2 months, the number needed to treat (NNT) was measured by applying the overall relative risk reduction in DAPA-HF (26%, 95%CI 15-35) to the proportion of patients with a primary outcome event in the placebo group of each MAGGIC risk score category (described by quintiles of score). The MAGGIC risk score was computable for 4740 of 4744 patients in DAPA-HF. The median score was 22 (range 3-43). The occurrence rate for the primary outcome was 7.2 per 100 patient-years in the lowest risk score quintile and 25.7 in the highest. A 1-point enhance in score was correlated with an 8% increase in the risk of a primary outcome occurrence (p<0.001). Dapagliflozin showed reduction in the risk of the primary outcome across quintiles of the MAGGIC risk score as compared to placebo (Figure – Interaction p value=0.69) and if the score was examined as a continuous variable (Interaction p value=0.56). The NNT to inhibit one primary occurrence was 39 (95%CI 29-68) in the lowest quintile of risk scores as compared to 14 (11-25) in the highest quintile (Figure). Similar consequences were shown for the individual components of the primary composite outcome and for all-cause mortality.
Conclusion: Patients with a wide spectrum of risk were included in DAPA-HF. Therapy with Dapagliflozin showed reduction in the risk of cardiovascular death or worsening heart failure as compared to placebo, regardless of baseline risk as estimated with the MAGGIC risk score.
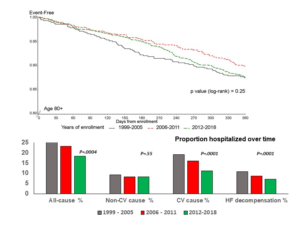
Chronic heart failure in octogenarians. Temporal trends in clinical characteristics, treatment and outcomes over two decades in a nationwide cardiology registry
Elderly > 80 years of age describe the most rapidly extending community part in Europe. Chronic heart failure (CHF) impacts over 10% of this cohort and develops a major M&M burden. Maria R De, at ESC Congress 2020: A digital Experience presented a study which examined the temporal trends in characteristics, treatment and outcomes over two decades in octogenarians enlisted in a nationwide registry.
14,283 CHF patients first enlisted in the registry since 1-1999 through 5-2018 as per the recruitment epoch. From these patients, patients with age 80+ (2520,17.6%) were divided into 3 groups: 1999-2005 (547, 10%); 2006-2011 (659, 16.5%); 2012-2018 (1314, 14.1%). The trends were analysed over time in characteristics, therapy, 1-year all-cause mortality and proportion admitted to hospital. The proportion of 80+ CHF patients (60% men, 84±3 years, LVEF 41±1%, HFrEF 49%) increased from 10% to 24% from 1999 to 2018. over the 3 epochs, a shift was observed regarding the HFpEF phenotype with arise in its driving factors (obesity, diabetes, hypertension, AFib). At the same time, the proportion treated with suggested treatment was increased. Cumulative 1-year mortality did not vary over the 3 epochs (figure top), whereas the proportion of 80+ hospitalized altogether for CV causes and for decompensated HF was decreased (figure bottom).
Conclusion: The clinical characteristics of octogenarians enlisted in a nationwide CHF registry have completely altered in 20 years, reflecting demographic differences, the development of CV risk factors and enhanced management. There was a regular execution of BB, MRA and devices. Survival of 80+ remained firm, however the proportion of those hospitalized for CV causes, and especially decompensated HF was decreased. These data recommend that cardiologists’ input may help to reduce the socioeconomic burden of CHF in the elderly.